

How to Write a Nursing Case Study Paper (A Guide)

Most nursing students dread writing a nursing case study analysis paper, yet it is a mandatory assignment; call it a rite of passage in nursing school. This is because it is a somewhat tricky process that is often overwhelming for nursing students. Nevertheless, by reading this guide prepared by our best nursing students, you should be able to easily and quickly write a nursing case study that can get you an excellent grade.
How different is this guide from similar guides all over the internet? Very different!
This guide provides all the pieces of information that one would need to write an A-grade nursing case study. These include the format for a nursing case study, a step-by-step guide on how to write a nursing case study, and all the important tips to follow when writing a nursing case study.
This comprehensive guide was developed by the top nursing essay writers at NurseMyGrade, so you can trust that the information herein is a gem that will catapult your grades to the next level. Expect updates as we unravel further information about writing a nursing case study.
Now that you know you’ve discovered a gold mine , let’s get right into it.
What Is a Nursing Case Study?
A nursing case study is a natural or imagined patient scenario designed to test the knowledge and skills of student nurses. Nursing case study assignments usually focus on testing knowledge and skills in areas of nursing study related to daily nursing practice.
As a nursing student, you must expect a nursing case study assignment at some point in your academic life. The fact that you are reading this post means that point is now.
While there is no standard structure for writing a nursing case study assignment, some things or elements must be present in your nursing assignment for your professor to consider it complete.
In the next section, you will discover what your instructor n expects in your nursing case study analysis. Remember, these are assignments where you are given a case study and are expected to write a case analysis report explaining how to handle such scenarios in real-life settings.
The Nursing Case Study Template
The typical nursing case study has nine sections. These are:
- Introduction
- Case presentation (Patient info, history, and medical condition)
- Diagnosis/Nursing assessment
- Intervention/Nursing care plan
- Discussion and recommendations
The Structure of a Nursing Case Study Analysis
You now know what nursing professors expect in a nursing case study analysis. In this section, we will explain what to include in each section of your nursing case study analysis to make it an excellent one.
1. Title page
The title page is essential in all types of academic writing. You must include it in your nursing case study analysis or any other essay or paper. And you must include it in the format recommended by your college.
If your college has no specific title page format, use the title page format of the style requested in the assignment prompt. In nursing college, virtually all assignments should be written in Harvard or APA format .
So, check your assignment prompt and create your title page correctly. The typical title page should include the topic of your paper, your name, the name of your professor, the course name, the date you are submitting the paper, and the name of your college.
2. Abstract
Most nursing professors require you to include an abstract in your nursing case study analysis. And even when you are not explicitly required to write one, it is good to do so. Of course, you should consult with your professor before doing so.
When writing an abstract for your paper, make sure it is about 200 words long. The abstract should include a brief summary of the case study, including all the essential information in the patient presentation, such as the history, age, and current diagnosis.
The summary should also include the nursing assessment, the current interventions, and recommendations.
3. Introduction
After writing the title page and the abstract, start writing the introduction. The introduction of a nursing case study analysis must briefly include the patient’s presentation, current diagnosis and medication, and recommendations. It must also include a strong thesis statement that shows what the paper is all about.
You shouldn’t just write an introduction for the sake of it. If you do so, your introduction will be bland. You need to put in good effort when writing your introduction. The best way to do this is to use your introduction to show you understand the case study perfectly and that you will analyze it right.
You can always write your introduction last. Many students do this because they believe writing an introduction last makes it more precise and accurate.
4. Case Presentation (Status of the Patient)
After introducing your nursing case study analysis, you should present the case where you outline the patient's status. It is usually straightforward to present a case.
You must paraphrase the patient scenario in the assignment prompt or brief. Focus on the demographic data of the patient (who they are, age, race, height, skin tone, occupation, relationships, marital status, appearance, etc.), why they are in the case study or scenario, reasons they sought medical attention, chief complaint, and current diagnosis and treatment. You should also discuss the actions performed on the patient, such as admission to the ICU, taking vital signs, recommending tests, etc.
In short, everything necessary in the patient scenario should be in your case presentation. You only need to avoid copying the patient scenario or case study word-for-word when writing your case presentation.
5. Diagnosis and Assessment
After the case presentation, you should explain the diagnosis. In other words, you should explain the condition, disease, or medical situation highlighted in the case presentation. For example, if the patient is a heavy smoker and he has COPD, it is at this point that you explain how COPD is linked to heavy smoking.
This is the section where you thoroughly discuss the disease process (pathophysiology) by highlighting the causes, symptoms, observations, and treatment methods. You should relate these to the patient’s status and give concrete evidence. You should describe the progression of the disease from when the client was admitted to a few hours or days after they were stabilized. Consider the first indication of the disease that prompted the patient to seek further medical assistance.
Your paper should also elucidate the diagnostic tests that should be conducted and the differential diagnosis. Ensure that each is given a well-founded rationale.
When explaining the condition, go deep into the pathophysiology. Focus specifically on the patient’s risk factors. Ensure you get your explanation from recent nursing literature (peer-reviewed scholarly journals published in the last 5 years). And do not forget to cite all the literature you get your facts from.
In short, this section should explain the patient’s condition or suffering.
6. Nursing Intervention
After the diagnosis and nursing assessment section, your nursing case study analysis should have an intervention section. This section is also known as the nursing care planning section. What you are supposed to do in this section is to present a nursing care plan for the patient presented in the patient scenario. You should describe the nursing care plan and goals for the patient. Record all the anticipated positive changes and assess whether the care plan addresses the patient's condition.
A good nursing care plan details the patient’s chief complaints or critical problems. It then describes the causes of these problems using evidence from recent medical or nursing literature. It then details the potential intervention for each problem. Lastly, it includes goals and evaluation strategies for the measures. Most professors, predominantly Australian and UK professors, prefer if this section is in table format.
Some nursing professors regard the intervention section (or nursing care plan section) as the most critical part of a nursing case study. This is because this part details precisely how the student nurse will react to the patient scenario (which is what the nursing professors want to know). So, ensure you make a reasonable effort when developing this section to get an excellent grade.
7. Discussion and Recommendations
The intervention section in a nursing case study is followed by a discussion and recommendations section. In this section, you are supposed to expound on the patient scenario, the diagnosis, and the nursing care plan. You should also expound on the potential outcomes if the care plan is followed correctly. The discussion should also explain the rationale for the care plan or its significant bits.
Recommendations should follow the discussion. Recommendations usually involve everything necessary that can be done or changed to manage a patient’s condition or prevent its reoccurrence. Anything that enhances the patient’s well-being can be a recommendation. Just make sure your key recommendations are supported by evidence.
8. Conclusion
This is the second last section of a typical nursing case study. What you need here is to summarize the entire case study. Ensure your summary has at least the case presentation, the nursing assessment/diagnosis, the intervention, and the key recommendations.
At the very end of your conclusion, add a closing statement. The statement should wrap up the whole thing nicely. Try to make it as impressive as possible.
9. References
This is the last section of a nursing case study. No nursing case study is complete without a references section. You should ensure your case study has in-text citations and a references page.
And you should make sure both are written as recommended in the assignment. The style section is usually Harvard or APA. Follow the recommended style to get a good grade on your essay.
Step-By-Step Guide to Writing a Nursing Case Study
You know all the key sections you must include in a nursing case study. You also know what exactly you need to do in each section. It is time to learn how to write a nursing case study. The process detailed below should be easy to follow because you know the typical nursing case study structure.
1. Understand the Assignment
When given a nursing case study assignment, the first thing you need to do is to read. You need to read two pieces of information slowly and carefully.
First, you need to read the prompt itself slowly and carefully. This is important because the prompt will have essential bits of information you need to know, including the style, the format, the word count, and the number of references needed. All these bits of information are essential to ensure your writing is correct.
Second, you need to read the patient scenario slowly and carefully. You should do this to understand it clearly so that you do not make any mistakes in your analysis.
2. Create a Rough Outline
Failure to plan is a plan to fail. That is not what you are in it for anyway! In other words, do not fail to create an outline for your case study analysis. Use the template provided in this essay to create a rough outline for your nursing case study analysis.
Ensure your outline is as detailed as it can be at this stage. You can do light research to achieve this aim. However, this is not exactly necessary because this is just a rough outline.
3. Conduct thorough research
After creating a rough outline, you should conduct thorough research. Your research should especially focus on providing a credible and evidence-based nursing assessment of the patient problem(s). You should only use evidence from recent nursing or medical literature.
You must also conduct thorough research to develop an effective intervention or nursing care plan. So when researching the patient’s problem and its diagnosis, you should also research the most suitable intervention or do it right after.
When conducting research, you should always note down your sources. So for every piece of information you find, and what to use, you should have its reference.
After conducting thorough research, you should enhance your rough outline using the new information you have discovered. Make sure it is as comprehensive as possible.
4. Write your nursing case study
You must follow your comprehensive outline to write your case study analysis at this stage. If you created a good outline, you should find it very easy to write your nursing case study analysis.
If you did not, writing your nursing case study will be challenging. Whenever you are stuck writing your case study analysis paper, you should re-read the part where we explain what to include in every section of your analysis. Doing so will help you know what to write to continue your essay. Writing a nursing case study analysis usually takes only a few hours.
5. Reference your case study
After writing your case study, ensure you add all in-text citations if you have not already. And when adding them, you should follow the style/format recommended in the assignment prompt (usually APA or Harvard style).
After adding in-text citations exactly where they need to be and in the correct format, add all the references you have used in a references page. And you should add them correctly as per the rules of the style you were asked to use.
Do not forget to organize your references alphabetically after creating your references page.
6. Thoroughly edit your case study
After STEP 5 above, you need to edit your case study. You should edit it slowly and carefully. Do this by proofreading it twice. Proofread it slowly each time to discover all the grammar, style, and punctuation errors. Remove all the errors you find.
After proofreading your essay twice, recheck it to ensure every sentence is straightforward. This will transform your ordinary case study into an A-grade one. Of course, it must also have all the standard sections expected in a case study.
Recheck your case study using a grammarly.com or a similar computer grammar checker to ensure it is perfect. Doing this will help you catch and eliminate all the remaining errors in your work.
7. Submit your case study analysis
After proofreading and editing your case study analysis, it will be 100% ready for submission. Just convert it into the format it is required in and submit it.
Nursing Case Study Tips and Tricks
The guide above and other information in this article should help you develop a good nursing case study analysis. Note that this guide focuses entirely on nursing case scenario-based papers, not research study-based nursing case studies. The tips and tricks in this section should help you ensure that the nursing case study analysis you create is excellent.
1. Begin early
The moment you see a nursing case study assignment prompt, identify a date to start writing it and create your own deadline to beat before the deadline stated in the prompt.
Do this and start writing your case study analysis early before your deadline. You will have plenty of time to do excellent research, develop an excellent paper, and edit your final paper as thoroughly as you want.
Most student nurses combine work and study. Therefore, if you decide to leave a nursing case study assignment until late to complete it, something could come up, and you could end up failing to submit it or submitting a rushed case study analysis.
2. Use the proper terminology
When writing an essay or any other academic paper, you are always encouraged to use the most straightforward language to make your work easy to understand. However, this is not true when writing a nursing case study analysis. While your work should certainly be easy to understand, you must use the right nursing terminology at every point where it is necessary. Failure to do this could damage your work or make it look less professional or convincing.
3. Avoid copying and pasting
If you are a serious nursing student, you know that copying and pasting are prohibited in assignments. However, sometimes copying and pasting can seem okay in nursing case studies. For example, it can seem okay to copy-paste the patient presentation. However, this is not okay. You are supposed to paraphrase the verbatim when presenting the patient presentation in your essay. You should also avoid copy-pasting information or texts directly. Every fact or evidence you research and find should be paraphrased to appear in your work. And it should be cited correctly.
4. Always ask for help if stuck
This is very important. Students are usually overwhelmed with academic work, especially a month or two to the end of the semester. If you are overwhelmed and think you will not have the time to complete your nursing case study analysis or submit a quality one, ask for help. Ask for help from a nursing assignment-help website like ours, and you will soon have a paper ready that you can use as you please. If you choose to get help from us, you will get a well-researched, well-planned, well-developed, and fully edited nursing case study.
5. Format your paper correctly
Many students forget to do proper formatting after writing their nursing case study analyses. Before you submit your paper, make sure you format it correctly. If you do not format your paper correctly, you will lose marks because of poor formatting. If you feel you are not very confident with your APA or Harvard formatting skills, send your paper to us to get it correctly formatted and ready for submission.
Now that you are all set up …
Our company has been among the best-rated nursing homework help companies in the last few years. Thousands of students have benefitted from our many academic writing guides. Many more have benefitted from direct help given by our experts.
- How to write a nursing philosophy statement.
- Writing an abstract poster presentation.
We have experienced nursing experts available every day of the week to provide nursing assignment help. They can easily research and write virtually any nursing assignment, including a nursing case study. So, if the information provided in this article isn’t making you feel any optimistic about writing an excellent nursing case study, get help from us.
Get help by ordering a custom nursing case study through this very website. If you do so, you will get a 100% original paper that is well-researched, well-written, well-formatted, and adequately referenced. Since the paper is original, you can use it anywhere without problems.
Thousands of students trust our company every week, month, and year. Be like them! Trust us for 100% confidentiality and speedy delivery.
Struggling with
Related Articles

How to Write a Nursing Interview Essay

Top Guide and Hints for Writing Great Nursing Competency Statements

Critical Appraisal or Article Critique Guide for Nursing Students
NurseMyGrades is being relied upon by thousands of students worldwide to ace their nursing studies. We offer high quality sample papers that help students in their revision as well as helping them remain abreast of what is expected of them.

Step-By-Step Guide to Writing a Nursing Case Study
You now know all the key sections you need to include in a nursing case study. You also know what exactly you need to do in each section. It is now time to know how exactly to write a nursing case study. The process detailed below should be easy to follow because you now know the typical structure of nursing case studies.
When given a nursing case study assignment, the first thing you need to do is to read. You need to read two pieces of information slowly and carefully.
First, you need to read the prompt itself slowly and carefully. This is important because the prompt will have important bits of information that you need to know, including the style, the format, the word count, and the number of references needed. All these bits of information are important to know to ensure what you are writing is the right thing.
Second, you need to read the patient scenario slowly and carefully. You should do this to understand it clearly so that you do not make any mistakes in your analysis.
- Create a rough outline
Failure to plan is a plan to fail. So do not fail to plan. In other words, do not fail to create an outline for your case study analysis. Use the template provided in this essay to create a rough outline for your nursing case study analysis.
Make sure your outline is as detailed as it can be at this stage. You can do light research to achieve this aim. However, this is not exactly necessary because this is just a rough outline.
- Conduct thorough research
After creating a rough outline, you should conduct thorough research. Your research should especially focus on providing a credible and evidence-based nursing assessment on the patient problem(s). The evidence you should use should only be from recent nursing or medical literature.
You will also need to conduct thorough research to come up with an effective intervention or nursing care plan. So when researching the patient’s problem and its diagnosis, you should also research the most suitable intervention or you should do it right after.
When conducting research, you should always note down your sources. So for every piece of information you find and what to use, you should have its reference.
After conducting thorough research, you should enhance your rough outline using the new pieces of information you have discovered. Make sure it is as comprehensive as possible.
- Write your nursing case study
At this stage, you simply need to follow your comprehensive outline to write your case study analysis. If you created a good outline, you should find it very easy to write your nursing case study analysis.
If you did not, you will find it difficult to write your nursing case study. Whenever you are stuck when writing your case study analysis paper, you should re-read the part of this article where we explain what to include in every section of your analysis. Doing so will help you know what exactly to write to continue with your essay. Writing a nursing case study analysis usually takes only a few hours.
- Reference your case study
After writing your case study, make sure you add all in-text citations if you had not added them already. And when adding them, you should make sure you follow the style/format recommended in the assignment prompt (usually APA or Harvard style).
After adding in-text citations exactly where they need to be and in the right format, add all the references you have used in a references page. And you should add them correctly as per the rules of the style you were asked to use.
Do not forget to organize your references alphabetically after you are done creating your references page.
- Thoroughly edit your case study
After STEP 5 above, you need to edit your case study. You should edit it slowly and carefully. Do this by proofreading it twice. Proofread it slowly each time to discover all the grammar, style, and punctuation errors. Remove all the errors you find.
After proofreading your essay twice, check it one more time to make sure every sentence is very easy to understand. This is what will transform your ordinary case study into an A-grade case study. Of course, it must also have all the standard sections expected in a case study.
Just to make sure your case study is absolutely perfect, check it one more time using a grammarly.com or a similar computer grammar checker. Doing this will help you catch and eliminate all the remaining errors in your work.
- Submit your case study analysis
After you are done proofreading and editing your case study analysis, it will be 100% ready for submission. Just convert it into the format it is required in and submit it.
Published by laura
View all posts by laura
📕 Studying HQ
10 nursing case study analysis examples [format + structure], bob cardens.
- August 6, 2022
If you are a nursing student, you may be asked to write a case study analysis. This can be a daunting task, but it is possible to do if you follow some simple steps. Here we include Nursing Case Study Analysis Examples to help you get started.
First, read the case study and make sure you understand the situation. Next, identify the key players involved and their role in the case. Finally, analyze the data presented and draw your own conclusions.
Writing a case study analysis can be challenging, but it is also an excellent way to learn more about nursing care. By taking the time to understand the situation and identify the key players, you will be able to gain valuable insights that can be applied to future cases.
What You'll Learn
10 Nursing Case Study Analysis Examples
Nursing case study analysis format and structure.
When it comes to writing a case study analysis, there is no one-size-fits-all approach. However, there is a general format and structure that you can follow to ensure your analysis is well-organized and flows smoothly. Here are the basics:
A nursing case study is a detailed study of a patient that is encountered by a nurse. The purpose of the case study is to provide a comprehensive view of the patient’s health condition and history. Nurse practitioners use case studies to enhance their ability to care for patients by providing them with a more complete picture of the patient’s health. Nurse practitioners may use different formats for their nursing case studies. However, all case studies should include certain key elements. These key elements include:
As a nursing practitioner, you will be responsible for analyzing patient cases and providing care based on your findings. There are key elements that you must take into account when performing a case analysis in order to ensure that you are providing the best possible care for your patients.
- The first element is the patient’s history. You will need to obtain a complete medical history in order to understand the background of the case and identify any potential risk factors.
- Next, you will need to perform a physical examination of the patient. This will help you to identify any physical signs or symptoms that may be related to the case.
- You will also need to order and review any laboratory tests or imaging studies that have been performed on the patient. These results can provide valuable information about the patient’s condition.
- Once you have gathered all of this information, you will need to start piecing together the puzzle to form a diagnosis. This process will involve synthesizing all of the information you have gathered and making a determination about what is causing the patient’s symptoms.
- Once you have made a diagnosis, you can start developing a treatment plan. This plan should be tailored specifically to the needs of the individual patient.
When writing a nursing case study, nurse practitioners should use a clear and concise format. The format should be easy to follow and understand. Nurse practitioners should also include all of the key elements in their nursing case studies. Nursing Case Study Analysis Examples
![10 nursing case study analysis examples [format + structure] 1 Nursing case study analysis examples](https://i0.wp.com/studyinghq.com/wp-content/uploads/2021/03/113124-84-CHECK.png?resize=84%2C84&ssl=1)
How to write a case study assignment
A case study is an in-depth analysis of a real-life situation or incident, as a way to illustrate content and theory to students. It is usually presented as a written report, but can also be done in the form of a presentation, video, or multimedia production.
Case studies are used in many different disciplines, including business, law, psychology, nursing, social work, and medical sciences.
A case study assignment is a type of paper that requires you to analyze a real-life or fictional situation and offer possible solutions. This can be a challenging task, but if you follow some basic guidelines, you can write a successful case study assignment.
Here are some tips on how to write a case study assignment:
- Read the case study carefully. Make sure you understand the situation and the problem that needs to be solved.
- Research the subject matter. You will need to have a good understanding of the relevant theories and concepts in order to offer possible solutions.
- Read the case study carefully. This may seem obvious, but it is important to get a clear understanding of the situation before you start writing. Make sure you have all the relevant facts and figures to hand before you start.
- Identify the key issues. Once you have read and understood the case study, you need to identify the key issues that it raises. These will form the basis of your analysis.
- Research the law/theory applicable to the key issues. Once you have identified the key issues, you need to research the law or theory that applies to them. This will help you to form your arguments and conclusions.
- Write your paper. Be sure to present your analysis in a clear and concise manner. Your paper should be well-organized and well-written
Start by filling this short order form order.studyinghq.com
And then follow the progressive flow.
Having an issue, chat with us here
Cathy, CS.
New Concept ? Let a subject expert write your paper for You
Have a subject expert write for you now, have a subject expert finish your paper for you, edit my paper for me, have an expert write your dissertation's chapter, popular topics.
Business Analysis Examples Essay Topics and Ideas How to Guides Nursing
- Nursing Solutions
- Study Guides
- Free College Essay Examples
- Privacy Policy
- Writing Service
- Discounts / Offers
Study Hub:
- Studying Blog
- Topic Ideas
- How to Guides
- Business Studying
- Nursing Studying
- Literature and English Studying
Writing Tools
- Citation Generator
- Topic Generator
- Paraphrasing Tool
- Conclusion Maker
- Research Title Generator
- Thesis Statement Generator
- Summarizing Tool
- Terms and Conditions
- Confidentiality Policy
- Cookies Policy
- Refund and Revision Policy
Our samples and other types of content are meant for research and reference purposes only. We are strongly against plagiarism and academic dishonesty.
Contact Us:
📞 +15512677917
2012-2024 © studyinghq.com. All rights reserved
Health Case Studies
(29 reviews)
Glynda Rees, British Columbia Institute of Technology
Rob Kruger, British Columbia Institute of Technology
Janet Morrison, British Columbia Institute of Technology
Copyright Year: 2017
Publisher: BCcampus
Language: English
Formats Available
Conditions of use.
Learn more about reviews.
Reviewed by Jessica Sellars, Medical assistant office instructor, Blue Mountain Community College on 10/11/23
This is a book of compiled and very well organized patient case studies. The author has broken it up by disease patient was experiencing and even the healthcare roles that took place in this patients care. There is a well thought out direction and... read more
Comprehensiveness rating: 5 see less
This is a book of compiled and very well organized patient case studies. The author has broken it up by disease patient was experiencing and even the healthcare roles that took place in this patients care. There is a well thought out direction and plan. There is an appendix to refer to as well if you are needing to find something specific quickly. I have been looking for something like this to help my students have a base to do their project on. This is the most comprehensive version I have found on the subject.
Content Accuracy rating: 5
This is a book compiled of medical case studies. It is very accurate and can be used to learn from great care and mistakes.
Relevance/Longevity rating: 5
This material is very relevant in this context. It also has plenty of individual case studies to utilize in many ways in all sorts of medical courses. This is a very useful textbook and it will continue to be useful for a very long time as you can still learn from each study even if medicine changes through out the years.
Clarity rating: 5
The author put a lot of thought into the ease of accessibility and reading level of the target audience. There is even a "how to use this resource" section which could be extremely useful to students.
Consistency rating: 5
The text follows a very consistent format throughout the book.
Modularity rating: 5
Each case study is individual broken up and in a group of similar case studies. This makes it extremely easy to utilize.
Organization/Structure/Flow rating: 5
The book is very organized and the appendix is through. It flows seamlessly through each case study.
Interface rating: 5
I had no issues navigating this book, It was clearly labeled and very easy to move around in.
Grammatical Errors rating: 5
I did not catch any grammar errors as I was going through the book
Cultural Relevance rating: 5
This is a challenging question for any medical textbook. It is very culturally relevant to those in medical or medical office degrees.
I have been looking for something like this for years. I am so happy to have finally found it.
Reviewed by Cindy Sun, Assistant Professor, Marshall University on 1/7/23
Interestingly, this is not a case of ‘you get what you pay for’. Instead, not only are the case studies organized in a fashion for ease of use through a detailed table of contents, the authors have included more support for both faculty and... read more
Interestingly, this is not a case of ‘you get what you pay for’. Instead, not only are the case studies organized in a fashion for ease of use through a detailed table of contents, the authors have included more support for both faculty and students. For faculty, the introduction section titled ‘How to use this resource’ and individual notes to educators before each case study contain application tips. An appendix overview lists key elements as issues / concepts, scenario context, and healthcare roles for each case study. For students, learning objectives are presented at the beginning of each case study to provide a framework of expectations.
The content is presented accurately and realistic.
The case studies read similar to ‘A Day In the Life of…’ with detailed intraprofessional communications similar to what would be overheard in patient care areas. The authors present not only the view of the patient care nurse, but also weave interprofessional vantage points through each case study by including patient interaction with individual professionals such as radiology, physician, etc.
In addition to objective assessment findings, the authors integrate standard orders for each diagnosis including medications, treatments, and tests allowing the student to incorporate pathophysiology components to their assessments.
Each case study is arranged in the same framework for consistency and ease of use.
This compilation of eight healthcare case studies focusing on new onset and exacerbation of prevalent diagnoses, such as heart failure, deep vein thrombosis, cancer, and chronic obstructive pulmonary disease advancing to pneumonia.
Each case study has a photo of the ‘patient’. Simple as this may seem, it gives an immediate mental image for the student to focus.
Interface rating: 4
As noted by previous reviewers, most of the links do not connect active web pages. This may be due to the multiple options for accessing this resource (pdf download, pdf electronic, web view, etc.).
Grammatical Errors rating: 4
A minor weakness that faculty will probably need to address prior to use is regarding specific term usages differences between Commonwealth countries and United States, such as lung sound descriptors as ‘quiet’ in place of ‘diminished’ and ‘puffers’ in place of ‘inhalers’.
The authors have provided a multicultural, multigenerational approach in selection of patient characteristics representing a snapshot of today’s patient population. Additionally, one case study focusing on heart failure is about a middle-aged adult, contrasting to the average aged patient the students would normally see during clinical rotations. This option provides opportunities for students to expand their knowledge on risk factors extending beyond age.
This resource is applicable to nursing students learning to care for patients with the specific disease processes presented in each case study or for the leadership students focusing on intraprofessional communication. Educators can assign as a supplement to clinical experiences or as an in-class application of knowledge.
Reviewed by Stephanie Sideras, Assistant Professor, University of Portland on 8/15/22
The eight case studies included in this text addressed high frequency health alterations that all nurses need to be able to manage competently. While diabetes was not highlighted directly, it was included as a potential comorbidity. The five... read more
The eight case studies included in this text addressed high frequency health alterations that all nurses need to be able to manage competently. While diabetes was not highlighted directly, it was included as a potential comorbidity. The five overarching learning objectives pulled from the Institute of Medicine core competencies will clearly resonate with any faculty familiar with Quality and Safety Education for Nurses curriculum.
The presentation of symptoms, treatments and management of the health alterations was accurate. Dialogue between the the interprofessional team was realistic. At times the formatting of lab results was confusing as they reflected reference ranges specific to the Canadian healthcare system but these occurrences were minimal and could be easily adapted.
The focus for learning from these case studies was communication - patient centered communication and interprofessional team communication. Specific details, such as drug dosing, was minimized, which increases longevity and allows for easy individualization of the case data.
While some vocabulary was specific to the Canadian healthcare system, overall the narrative was extremely engaging and easy to follow. Subjective case data from patient or provider were formatted in italics and identified as 'thoughts'. Objective and behavioral case data were smoothly integrated into the narrative.
The consistency of formatting across the eight cases was remarkable. Specific learning objectives are identified for each case and these remain consistent across the range of cases, varying only in the focus for the goals for each different health alterations. Each case begins with presentation of essential patient background and the progress across the trajectory of illness as the patient moves from location to location encountering different healthcare professionals. Many of the characters (the triage nurse in the Emergency Department, the phlebotomist) are consistent across the case situations. These consistencies facilitate both application of a variety of teaching methods and student engagement with the situated learning approach.
Case data is presented by location and begins with the patient's first encounter with the healthcare system. This allows for an examination of how specific trajectories of illness are manifested and how care management needs to be prioritized at different stages. This approach supports discussions of care transitions and the complexity of the associated interprofessional communication.
The text is well organized. The case that has two levels of complexity is clearly identified
The internal links between the table of contents and case specific locations work consistently. In the EPUB and the Digital PDF the external hyperlinks are inconsistently valid.
The grammatical errors were minimal and did not detract from readability
Cultural diversity is present across the cases in factors including race, ethnicity, socioeconomic status, family dynamics and sexual orientation.
The level of detail included in these cases supports a teaching approach to address all three spectrums of learning - knowledge, skills and attitudes - necessary for the development of competent practice. I also appreciate the inclusion of specific assessment instruments that would facilitate a discussion of evidence based practice. I will enjoy using these case to promote clinical reasoning discussions of data that is noticed and interpreted with the resulting prioritizes that are set followed by reflections that result from learner choices.
Reviewed by Chris Roman, Associate Professor, Butler University on 5/19/22
It would be extremely difficult for a book of clinical cases to comprehensively cover all of medicine, and this text does not try. Rather, it provides cases related to common medical problems and introduces them in a way that allows for various... read more
Comprehensiveness rating: 4 see less
It would be extremely difficult for a book of clinical cases to comprehensively cover all of medicine, and this text does not try. Rather, it provides cases related to common medical problems and introduces them in a way that allows for various learning strategies to be employed to leverage the cases for deeper student learning and application.
The narrative form of the cases is less subject to issues of accuracy than a more content-based book would be. That said, the cases are realistic and reasonable, avoiding being too mundane or too extreme.
These cases are narrative and do not include many specific mentions of drugs, dosages, or other aspects of clinical care that may grow/evolve as guidelines change. For this reason, the cases should be “evergreen” and can be modified to suit different types of learners.
Clarity rating: 4
The text is written in very accessible language and avoids heavy use of technical language. Depending on the level of learner, this might even be too simplistic and omit some details that would be needed for physicians, pharmacists, and others to make nuanced care decisions.
The format is very consistent with clear labeling at transition points.
The authors point out in the introductory materials that this text is designed to be used in a modular fashion. Further, they have built in opportunities to customize each cases, such as giving dates of birth at “19xx” to allow for adjustments based on instructional objectives, etc.
The organization is very easy to follow.
I did not identify any issues in navigating the text.
The text contains no grammatical errors, though the language is a little stiff/unrealistic in some cases.
Cases involve patients and members of the care team that are of varying ages, genders, and racial/ethnic backgrounds
Reviewed by Trina Larery, Assistant Professor, Pittsburg State University on 4/5/22
The book covers common scenarios, providing allied health students insight into common health issues. The information in the book is thorough and easily modified if needed to include other scenarios not listed. The material was easy to understand... read more
The book covers common scenarios, providing allied health students insight into common health issues. The information in the book is thorough and easily modified if needed to include other scenarios not listed. The material was easy to understand and apply to the classroom. The E-reader format included hyperlinks that bring the students to subsequent clinical studies.
Content Accuracy rating: 4
The treatments were explained and rationales were given, which can be very helpful to facilitate effective learning for a nursing student or novice nurse. The case studies were accurate in explanation. The DVT case study incorrectly identifies the location of the clot in the popliteal artery instead of in the vein.
The content is relevant to a variety of different types of health care providers and due to the general nature of the cases, will remain relevant over time. Updates should be made annually to the hyperlinks and to assure current standard of practice is still being met.
Clear, simple and easy to read.
Consistent with healthcare terminology and framework throughout all eight case studies.
The text is modular. Cases can be used individually within a unit on the given disease process or relevant sections of a case could be used to illustrate a specific point providing great flexibility. The appendix is helpful in locating content specific to a certain diagnosis or a certain type of health care provider.
The book is well organized, presenting in a logical clear fashion. The appendix allows the student to move about the case study without difficulty.
The interface is easy and simple to navigate. Some links to external sources might need to be updated regularly since those links are subject to change based on current guidelines. A few hyperlinks had "page not found".
Few grammatical errors were noted in text.
The case studies include people of different ethnicities, socioeconomic status, ages, and genders to make this a very useful book.
I enjoyed reading the text. It was interesting and relevant to today's nursing student. There are roughly 25 broken online links or "pages not found", care needs to be taken to update at least annually and assure links are valid and utilizing the most up to date information.
Reviewed by Benjamin Silverberg, Associate Professor/Clinician, West Virginia University on 3/24/22
The appendix reviews the "key roles" and medical venues found in all 8 cases, but is fairly spartan on medical content. The table of contents at the beginning only lists the cases and locations of care. It can be a little tricky to figure out what... read more
Comprehensiveness rating: 3 see less
The appendix reviews the "key roles" and medical venues found in all 8 cases, but is fairly spartan on medical content. The table of contents at the beginning only lists the cases and locations of care. It can be a little tricky to figure out what is going on where, especially since each case is largely conversation-based. Since this presents 8 cases (really 7 with one being expanded upon), there are many medical topics (and venues) that are not included. It's impossible to include every kind of situation, but I'd love to see inclusion of sexual health, renal pathology, substance abuse, etc.
Though there are differences in how care can be delivered based on personal style, changing guidelines, available supplies, etc, the medical accuracy seems to be high. I did not detect bias or industry influence.
Relevance/Longevity rating: 4
Medications are generally listed as generics, with at least current dosing recommendations. The text gives a picture of what care looks like currently, but will be a little challenging to update based on new guidelines (ie, it can be hard to find the exact page in which a medication is dosed/prescribed). Even if the text were to be a little out of date, an instructor can use that to point out what has changed (and why).
Clear text, usually with definitions of medical slang or higher-tier vocabulary. Minimal jargon and there are instances where the "characters" are sorting out the meaning as well, making it accessible for new learners, too.
Overall, the style is consistent between cases - largely broken up into scenes and driven by conversation rather than descriptions of what is happening.
There are 8 (well, again, 7) cases which can be reviewed in any order. Case #2 builds upon #1, which is intentional and a good idea, though personally I would have preferred one case to have different possible outcomes or even a recurrence of illness. Each scene within a case is reasonably short.
Organization/Structure/Flow rating: 4
These cases are modular and don't really build on concepts throughout. As previously stated, case #2 builds upon #1, but beyond that, there is no progression. (To be sure, the authors suggest using case #1 for newer learners and #2 for more advanced ones.) The text would benefit from thematic grouping, a longer introduction and debriefing for each case (there are learning objectives but no real context in medical education nor questions to reflect on what was just read), and progressively-increasing difficulty in medical complexity, ethics, etc.
I used the PDF version and had no interface issues. There are minimal photographs and charts. Some words are marked in blue but those did not seem to be hyperlinked anywhere.
No noticeable errors in grammar, spelling, or formatting were noted.
I appreciate that some diversity of age and ethnicity were offered, but this could be improved. There were Canadian Indian and First Nations patients, for example, as well as other characters with implied diversity, but there didn't seem to be any mention of gender diverse or non-heterosexual people, or disabilities. The cases tried to paint family scenes (the first patient's dog was fairly prominently mentioned) to humanize them. Including more cases would allow for more opportunities to include sex/gender minorities, (hidden) disabilities, etc.
The text (originally from 2017) could use an update. It could be used in conjunction with other Open Texts, as a compliment to other coursework, or purely by itself. The focus is meant to be on improving communication, but there are only 3 short pages at the beginning of the text considering those issues (which are really just learning objectives). In addition to adding more cases and further diversity, I personally would love to see more discussion before and after the case to guide readers (and/or instructors). I also wonder if some of the ambiguity could be improved by suggesting possible health outcomes - this kind of counterfactual comparison isn't possible in real life and could be really interesting in a text. Addition of comprehension/discussion questions would also be worthwhile.
Reviewed by Danielle Peterson, Assistant Professor, University of Saint Francis on 12/31/21
This text provides readers with 8 case studies which include both chronic and acute healthcare issues. Although not comprehensive in regard to types of healthcare conditions, it provides a thorough look at the communication between healthcare... read more
This text provides readers with 8 case studies which include both chronic and acute healthcare issues. Although not comprehensive in regard to types of healthcare conditions, it provides a thorough look at the communication between healthcare workers in acute hospital settings. The cases are primarily set in the inpatient hospital setting, so the bulk of the clinical information is basic emergency care and inpatient protocol: vitals, breathing, medication management, etc. The text provides a table of contents at opening of the text and a handy appendix at the conclusion of the text that outlines each case’s issue(s), scenario, and healthcare roles. No index or glossary present.
Although easy to update, it should be noted that the cases are taking place in a Canadian healthcare system. Terms may be unfamiliar to some students including “province,” “operating theatre,” “physio/physiotherapy,” and “porter.” Units of measurement used include Celsius and meters. Also, the issue of managed care, health insurance coverage, and length of stay is missing for American students. These are primary issues that dictate much of the healthcare system in the US and a primary job function of social workers, nurse case managers, and medical professionals in general. However, instructors that wish to add this to the case studies could do so easily.
The focus of this text is on healthcare communication which makes it less likely to become obsolete. Much of the clinical information is stable healthcare practice that has been standard of care for quite some time. Nevertheless, given the nature of text, updates would be easy to make. Hyperlinks should be updated to the most relevant and trustworthy sources and checked frequently for effectiveness.
The spacing that was used to note change of speaker made for ease of reading. Although unembellished and plain, I expect students to find this format easy to digest and interesting, especially since the script is appropriately balanced with ‘human’ qualities like the current TV shows and songs, the use of humor, and nonverbal cues.
A welcome characteristic of this text is its consistency. Each case is presented in a similar fashion and the roles of the healthcare team are ‘played’ by the same character in each of the scenarios. This allows students to see how healthcare providers prioritize cases and juggle the needs of multiple patients at once. Across scenarios, there was inconsistency in when clinical terms were hyperlinked.
The text is easily divisible into smaller reading sections. However, since the nature of the text is script-narrative format, if significant reorganization occurs, one will need to make sure that the communication of the script still makes sense.
The text is straightforward and presented in a consistent fashion: learning objectives, case history, a script of what happened before the patient enters the healthcare setting, and a script of what happens once the patient arrives at the healthcare setting. The authors use the term, “ideal interactions,” and I would agree that these cases are in large part, ‘best case scenarios.’ Due to this, the case studies are well organized, clear, logical, and predictable. However, depending on the level of student, instructors may want to introduce complications that are typical in the hospital setting.
The interface is pleasing and straightforward. With exception to the case summary and learning objectives, the cases are in narrative, script format. Each case study supplies a photo of the ‘patient’ and one of the case studies includes a link to a 3-minute video that introduces the reader to the patient/case. One of the highlights of this text is the use of hyperlinks to various clinical practices (ABG, vital signs, transfer of patient). Unfortunately, a majority of the links are broken. However, since this is an open text, instructors can update the links to their preference.
Although not free from grammatical errors, those that were noticed were minimal and did not detract from reading.
Cultural Relevance rating: 4
Cultural diversity is visible throughout the patients used in the case studies and includes factors such as age, race, socioeconomic status, family dynamics, and sexual orientation. A moderate level of diversity is noted in the healthcare team with some stereotypes: social workers being female, doctors primarily male.
As a social work instructor, I was grateful to find a text that incorporates this important healthcare role. I would have liked to have seen more content related to advance directives, mediating decision making between the patient and care team, emotional and practical support related to initial diagnosis and discharge planning, and provision of support to colleagues, all typical roles of a medical social worker. I also found it interesting that even though social work was included in multiple scenarios, the role was only introduced on the learning objectives page for the oncology case.
Reviewed by Crystal Wynn, Associate Professor, Virginia State University on 7/21/21
The text covers a variety of chronic diseases within the cases; however, not all of the common disease states were included within the text. More chronic diseases need to be included such as diabetes, cancer, and renal failure. Not all allied... read more
The text covers a variety of chronic diseases within the cases; however, not all of the common disease states were included within the text. More chronic diseases need to be included such as diabetes, cancer, and renal failure. Not all allied health care team members are represented within the case study. Key terms appear throughout the case study textbook and readers are able to click on a hyperlink which directs them to the definition and an explanation of the key term.
Content is accurate, error-free and unbiased.
The content is up-to-date, but not in a way that will quickly make the text obsolete within a short period of time. The text is written and/or arranged in such a way that necessary updates will be relatively easy and straightforward to implement.
The text is written in lucid, accessible prose, and provides adequate context for any jargon/technical terminology used
The text is internally consistent in terms of terminology and framework.
The text is easily and readily divisible into smaller reading sections that can be assigned at different points within the course. Each case can be divided into a chronic disease state unit, which will allow the reader to focus on one section at a time.
Organization/Structure/Flow rating: 3
The topics in the text are presented in a logical manner. Each case provides an excessive amount of language that provides a description of the case. The cases in this text reads more like a novel versus a clinical textbook. The learning objectives listed within each case should be in the form of questions or activities that could be provided as resources for instructors and teachers.
Interface rating: 3
There are several hyperlinks embedded within the textbook that are not functional.
The text contains no grammatical errors.
Cultural Relevance rating: 3
The text is not culturally insensitive or offensive in any way. More examples of cultural inclusiveness is needed throughout the textbook. The cases should be indicative of individuals from a variety of races and ethnicities.
Reviewed by Rebecca Hillary, Biology Instructor, Portland Community College on 6/15/21
This textbook consists of a collection of clinical case studies that can be applicable to a wide range of learning environments from supplementing an undergraduate Anatomy and Physiology Course, to including as part of a Medical or other health... read more
This textbook consists of a collection of clinical case studies that can be applicable to a wide range of learning environments from supplementing an undergraduate Anatomy and Physiology Course, to including as part of a Medical or other health care program. I read the textbook in E-reader format and this includes hyperlinks that bring the students to subsequent clinical study if the book is being used in a clinical classroom. This book is significantly more comprehensive in its approach from other case studies I have read because it provides a bird’s eye view of the many clinicians, technicians, and hospital staff working with one patient. The book also provides real time measurements for patients that change as they travel throughout the hospital until time of discharge.
Each case gave an accurate sense of the chaos that would be present in an emergency situation and show how the conditions affect the practitioners as well as the patients. The reader gets an accurate big picture--a feel for each practitioner’s point of view as well as the point of view of the patient and the patient’s family as the clock ticks down and the patients are subjected to a number of procedures. The clinical information contained in this textbook is all in hyperlinks containing references to clinical skills open text sources or medical websites. I did find one broken link on an external medical resource.
The diseases presented are relevant and will remain so. Some of the links are directly related to the Canadian Medical system so they may not be applicable to those living in other regions. Clinical links may change over time but the text itself will remain relevant.
Each case study clearly presents clinical data as is it recorded in real time.
Each case study provides the point of view of several practitioners and the patient over several days. While each of the case studies covers different pathology they all follow this same format, several points of view and data points, over a number of days.
The case studies are divided by days and this was easy to navigate as a reader. It would be easy to assign one case study per body system in an Anatomy and Physiology course, or to divide them up into small segments for small in class teaching moments.
The topics are presented in an organized way showing clinical data over time and each case presents a large number of view points. For example, in the first case study, the patient is experiencing difficulty breathing. We follow her through several days from her entrance to the emergency room. We meet her X Ray Technicians, Doctor, Nurses, Medical Assistant, Porter, Physiotherapist, Respiratory therapist, and the Lab Technicians running her tests during her stay. Each practitioner paints the overall clinical picture to the reader.
I found the text easy to navigate. There were not any figures included in the text, only clinical data organized in charts. The figures were all accessible via hyperlink. Some figures within the textbook illustrating patient scans could have been helpful but I did not have trouble navigating the links to visualize the scans.
I did not see any grammatical errors in the text.
The patients in the text are a variety of ages and have a variety of family arrangements but there is not much diversity among the patients. Our seven patients in the eight case studies are mostly white and all cis gendered.
Some of the case studies, for example the heart failure study, show clinical data before and after drug treatments so the students can get a feel for mechanism in physiological action. I also liked that the case studies included diet and lifestyle advice for the patients rather than solely emphasizing these pharmacological interventions. Overall, I enjoyed reading through these case studies and I plan to utilize them in my Anatomy and Physiology courses.
Reviewed by Richard Tarpey, Assistant Professor, Middle Tennessee State University on 5/11/21
As a case study book, there is no index or glossary. However, medical and technical terms provide a useful link to definitions and explanations that will prove useful to students unfamiliar with the terms. The information provided is appropriate... read more
As a case study book, there is no index or glossary. However, medical and technical terms provide a useful link to definitions and explanations that will prove useful to students unfamiliar with the terms. The information provided is appropriate for entry-level health care students. The book includes important health problems, but I would like to see coverage of at least one more chronic/lifestyle issue such as diabetes. The book covers adult issues only.
Content is accurate without bias
The content of the book is relevant and up-to-date. It addresses conditions that are prevalent in today's population among adults. There are no pediatric cases, but this does not significantly detract from the usefulness of the text. The format of the book lends to easy updating of data or information.
The book is written with clarity and is easy to read. The writing style is accessible and technical terminology is explained with links to more information.
Consistency is present. Lack of consistency is typically a problem with case study texts, but this book is consistent with presentation, format, and terminology throughout each of the eight cases.
The book has high modularity. Each of the case studies can be used independently from the others providing flexibility. Additionally, each case study can be partitioned for specific learning objectives based on the learning objectives of the course or module.
The book is well organized, presenting students conceptually with differing patient flow patterns through a hospital. The patient information provided at the beginning of each case is a wonderful mechanism for providing personal context for the students as they consider the issues. Many case studies focus on the problem and the organization without students getting a patient's perspective. The patient perspective is well represented in these cases.
The navigation through the cases is good. There are some terminology and procedure hyperlinks within the cases that do not work when accessed. This is troubling if you intend to use the text for entry-level health care students since many of these links are critical for a full understanding of the case.
There are some non-US variants of spelling and a few grammatical errors, but these do not detract from the content of the messages of each case.
The book is inclusive of differing backgrounds and perspectives. No insensitive or offensive references were found.
I like this text for its application flexibility. The book is useful for non-clinical healthcare management students to introduce various healthcare-related concepts and terminology. The content is also helpful for the identification of healthcare administration managerial issues for students to consider. The book has many applications.
Reviewed by Paula Baldwin, Associate Professor/Communication Studies, Western Oregon University on 5/10/21
The different case studies fall on a range, from crisis care to chronic illness care. read more
The different case studies fall on a range, from crisis care to chronic illness care.
The contents seems to be written as they occurred to represent the most complete picture of each medical event's occurence.
These case studies are from the Canadian medical system, but that does not interfere with it's applicability.
It is written for a medical audience, so the terminology is mostly formal and technical.
Some cases are shorter than others and some go in more depth, but it is not problematic.
The eight separate case studies is the perfect size for a class in the quarter system. You could combine this with other texts, videos or learning modalities, or use it alone.
As this is a case studies book, there is not a need for a logical progression in presentation of topics.
No problems in terms of interface.
I have not seen any grammatical errors.
I did not see anything that was culturally insensitive.
I used this in a Health Communication class and it has been extraordinarily successful. My studies are analyzing the messaging for the good, the bad, and the questionable. The case studies are widely varied and it gives the class insights into hospital experiences, both front and back stage, that they would not normally be able to examine. I believe that because it is based real-life medical incidents, my students are finding the material highly engaging.
Reviewed by Marlena Isaac, Instructor, Aiken Technical College on 4/23/21
This text is great to walk through patient care with entry level healthcare students. The students are able to take in the information, digest it, then provide suggestions to how they would facilitate patient healing. Then when they are faced with... read more
This text is great to walk through patient care with entry level healthcare students. The students are able to take in the information, digest it, then provide suggestions to how they would facilitate patient healing. Then when they are faced with a situation in clinical they are not surprised and now how to move through it effectively.
The case studies provided accurate information that relates to the named disease.
It is relevant to health care studies and the development of critical thinking.
Cases are straightforward with great clinical information.
Clinical information is provided concisely.
Appropriate for clinical case study.
Presented to facilitate information gathering.
Takes a while to navigate in the browser.
Cultural Relevance rating: 1
Text lacks adequate representation of minorities.
Reviewed by Kim Garcia, Lecturer III, University of Texas Rio Grande Valley on 11/16/20
The book has 8 case studies, so obviously does not cover the whole of medicine, but the cases provided are descriptive and well developed. Cases are presented at different levels of difficulty, making the cases appropriate for students at... read more
The book has 8 case studies, so obviously does not cover the whole of medicine, but the cases provided are descriptive and well developed. Cases are presented at different levels of difficulty, making the cases appropriate for students at different levels of clinical knowledge. The human element of both patient and health care provider is well captured. The cases are presented with a focus on interprofessional interaction and collaboration, more so than teaching medical content.
Content is accurate and un-biased. No errors noted. Most diagnostic and treatment information is general so it will remain relevant over time. The content of these cases is more appropriate for teaching interprofessional collaboration and less so for teaching the medical care for each diagnosis.
The content is relevant to a variety of different types of health care providers (nurses, radiologic technicians, medical laboratory personnel, etc) and due to the general nature of the cases, will remain relevant over time.
Easy to read. Clear headings are provided for sections of each case study and these section headings clearly tell when time has passed or setting has changed. Enough description is provided to help set the scene for each part of the case. Much of the text is written in the form of dialogue involving patient, family and health care providers, making it easy to adapt for role play. Medical jargon is limited and links for medical terms are provided to other resources that expound on medical terms used.
The text is consistent in structure of each case. Learning objectives are provided. Cases generally start with the patient at home and move with the patient through admission, testing and treatment, using a variety of healthcare services and encountering a variety of personnel.
The text is modular. Cases could be used individually within a unit on the given disease process or relevant sections of a case could be used to illustrate a specific point. The appendix is helpful in locating content specific to a certain diagnosis or a certain type of health care provider.
Each case follows a patient in a logical, chronologic fashion. A clear table of contents and appendix are provided which allows the user to quickly locate desired content. It would be helpful if the items in the table of contents and appendix were linked to the corresponding section of the text.
The hyperlinks to content outside this book work, however using the back arrow on your browser returns you to the front page of the book instead of to the point at which you left the text. I would prefer it if the hyperlinks opened in a new window or tab so closing that window or tab would leave you back where you left the text.
No grammatical errors were noted.
The text is culturally inclusive and appropriate. Characters, both patients and care givers are of a variety of races, ethnicities, ages and backgrounds.
I enjoyed reading the cases and reviewing this text. I can think of several ways in which I will use this content.
Reviewed by Raihan Khan, Instructor/Assistant Professor, James Madison University on 11/3/20
The book contains several important health issues, however still missing some chronic health issues that the students should learn before they join the workforce, such as diabetes-related health issues suffered by the patients. read more
The book contains several important health issues, however still missing some chronic health issues that the students should learn before they join the workforce, such as diabetes-related health issues suffered by the patients.
The health information contained in the textbook is mostly accurate.
I think the book is written focusing on the current culture and health issues faced by the patients. To keep the book relevant in the future, the contexts especially the culture/lifestyle/health care modalities, etc. would need to be updated regularly.
The language is pretty simple, clear, and easy to read.
There is no complaint about consistency. One of the main issues of writing a book, consistency was well managed by the authors.
The book is easy to explore based on how easy the setup is. Students can browse to the specific section that they want to read without much hassle of finding the correct information.
The organization is simple but effective. The authors organized the book based on what can happen in a patient's life and what possible scenarios students should learn about the disease. From that perspective, the book does a good job.
The interface is easy and simple to navigate. Some links to external sources might need to be updated regularly since those links are subject to change that is beyond the author's control. It's frustrating for the reader when the external link shows no information.
The book is free of any major language and grammatical errors.
The book might do a little better in cultural competency. e.g. Last name Singh is mainly for Sikh people. In the text Harj and Priya Singh are Muslim. the authors can consult colleagues who are more familiar with those cultures and revise some cultural aspects of the cases mentioned in the book.
The book is a nice addition to the open textbook world. Hope to see more health issues covered by the book.
Reviewed by Ryan Sheryl, Assistant Professor, California State University, Dominguez Hills on 7/16/20
This text contains 8 medical case studies that reflect best practices at the time of publication. The text identifies 5 overarching learning objectives: interprofessional collaboration, client centered care, evidence-based practice, quality... read more
This text contains 8 medical case studies that reflect best practices at the time of publication. The text identifies 5 overarching learning objectives: interprofessional collaboration, client centered care, evidence-based practice, quality improvement, and informatics. While the case studies do not cover all medical conditions or bodily systems, the book is thorough in conveying details of various patients and medical team members in a hospital environment. Rather than an index or glossary at the end of the text, it contains links to outside websites for more information on medical tests and terms referenced in the cases.
The content provided is reflective of best practices in patient care, interdisciplinary collaboration, and communication at the time of publication. It is specifically accurate for the context of hospitals in Canada. The links provided throughout the text have the potential to supplement with up-to-date descriptions and definitions, however, many of them are broken (see notes in Interface section).
The content of the case studies reflects the increasingly complex landscape of healthcare, including a variety of conditions, ages, and personal situations of the clients and care providers. The text will require frequent updating due to the rapidly changing landscape of society and best practices in client care. For example, a future version may include inclusive practices with transgender clients, or address ways medical racism implicitly impacts client care (see notes in Cultural Relevance section).
The text is written clearly and presents thorough, realistic details about working and being treated in an acute hospital context.
The text is very straightforward. It is consistent in its structure and flow. It uses consistent terminology and follows a structured framework throughout.
Being a series of 8 separate case studies, this text is easily and readily divisible into smaller sections. The text was designed to be taken apart and used piece by piece in order to serve various learning contexts. The parts of each case study can also be used independently of each other to facilitate problem solving.
The topics in the case studies are presented clearly. The structure of each of the case studies proceeds in a similar fashion. All of the cases are set within the same hospital so the hospital personnel and service providers reappear across the cases, giving a textured portrayal of the experiences of the various service providers. The cases can be used individually, or one service provider can be studied across the various studies.
The text is very straightforward, without complex charts or images that could become distorted. Many of the embedded links are broken and require updating. The links that do work are a very useful way to define and expand upon medical terms used in the case studies.
Grammatical errors are minimal and do not distract from the flow of the text. In one instance the last name Singh is spelled Sing, and one patient named Fred in the text is referred to as Frank in the appendix.
The cases all show examples of health care personnel providing compassionate, client-centered care, and there is no overt discrimination portrayed. Two of the clients are in same-sex marriages and these are shown positively. It is notable, however, that the two cases presenting people of color contain more negative characteristics than the other six cases portraying Caucasian people. The people of color are the only two examples of clients who smoke regularly. In addition, the Indian client drinks and is overweight, while the First Nations client is the only one in the text to have a terminal diagnosis. The Indian client is identified as being Punjabi and attending a mosque, although there are only 2% Muslims in the Punjab province of India. Also, the last name Singh generally indicates a person who is a Hindu or Sikh, not Muslim.
Reviewed by Monica LeJeune, RN Instructor, LSUE on 4/24/20
Has comprehensive unfolding case studies that guide the reader to recognize and manage the scenario presented. Assists in critical thinking process. read more
Has comprehensive unfolding case studies that guide the reader to recognize and manage the scenario presented. Assists in critical thinking process.
Accurately presents health scenarios with real life assessment techniques and patient outcomes.
Relevant to nursing practice.
Clearly written and easily understood.
Consistent with healthcare terminology and framework
Has a good reading flow.
Topics presented in logical fashion
Easy to read.
No grammatical errors noted.
Text is not culturally insensitive or offensive.
Good book to have to teach nursing students.
Reviewed by april jarrell, associate professor, J. Sargeant Reynolds Community College on 1/7/20
The text is a great case study tool that is appropriate for nursing school instructors to use in aiding students to learn the nursing process. read more
The text is a great case study tool that is appropriate for nursing school instructors to use in aiding students to learn the nursing process.
The content is accurate and evidence based. There is no bias noted
The content in the text is relevant, up to date for nursing students. It will be easy to update content as needed because the framework allows for addition to the content.
The text is clear and easy to understand.
Framework and terminology is consistent throughout the text; the case study is a continual and takes the student on a journey with the patient. Great for learning!
The case studies can be easily divided into smaller sections to allow for discussions, and weekly studies.
The text and content progress in a logical, clear fashion allowing for progression of learning.
No interface issues noted with this text.
No grammatical errors noted in the text.
No racial or culture insensitivity were noted in the text.
I would recommend this text be used in nursing schools. The use of case studies are helpful for students to learn and practice the nursing process.
Reviewed by Lisa Underwood, Practical Nursing Instructor, NTCC on 12/3/19
The text provides eight comprehensive case studies that showcase the different viewpoints of the many roles involved in patient care. It encompasses the most common seen diagnoses seen across healthcare today. Each case study comes with its own... read more
The text provides eight comprehensive case studies that showcase the different viewpoints of the many roles involved in patient care. It encompasses the most common seen diagnoses seen across healthcare today. Each case study comes with its own set of learning objectives that can be tweaked to fit several allied health courses. Although the case studies are designed around the Canadian Healthcare System, they are quite easily adaptable to fit most any modern, developed healthcare system.
Content Accuracy rating: 3
Overall, the text is quite accurate. There is one significant error that needs to be addressed. It is located in the DVT case study. In the study, a popliteal artery clot is mislabeled as a DVT. DVTs are located in veins, not in arteries. That said, the case study on the whole is quite good. This case study could be used as a learning tool in the classroom for discussion purposes or as a way to test student understanding of DVTs, on example might be, "Can they spot the error?"
At this time, all of the case studies within the text are current. Healthcare is an ever evolving field that rests on the best evidence based practice. Keeping that in mind, educators can easily adapt the studies as the newest evidence emerges and changes practice in healthcare.
All of the case studies are well written and easy to understand. The text includes several hyperlinks and it also highlights certain medical terminology to prompt readers as a way to enhance their learning experience.
Across the text, the language, style, and format of the case studies are completely consistent.
The text is divided into eight separate case studies. Each case study may be used independently of the others. All case studies are further broken down as the focus patient passes through each aspect of their healthcare system. The text's modularity makes it possible to use a case study as individual work, group projects, class discussions, homework or in a simulation lab.
The case studies and the diagnoses that they cover are presented in such a way that educators and allied health students can easily follow and comprehend.
The book in itself is free of any image distortion and it prints nicely. The text is offered in a variety of digital formats. As noted in the above reviews, some of the hyperlinks have navigational issues. When the reader attempts to access them, a "page not found" message is received.
There were minimal grammatical errors. Some of which may be traced back to the differences in our spelling.
The text is culturally relevant in that it includes patients from many different backgrounds and ethnicities. This allows educators and students to explore cultural relevance and sensitivity needs across all areas in healthcare. I do not believe that the text was in any way insensitive or offensive to the reader.
By using the case studies, it may be possible to have an open dialogue about the differences noted in healthcare systems. Students will have the ability to compare and contrast the Canadian healthcare system with their own. I also firmly believe that by using these case studies, students can improve their critical thinking skills. These case studies help them to "put it all together".
Reviewed by Melanie McGrath, Associate Professor, TRAILS on 11/29/19
The text covered some of the most common conditions seen by healthcare providers in a hospital setting, which forms a solid general base for the discussions based on each case. read more
The text covered some of the most common conditions seen by healthcare providers in a hospital setting, which forms a solid general base for the discussions based on each case.
I saw no areas of inaccuracy
As in all healthcare texts, treatments and/or tests will change frequently. However, everything is currently up-to-date thus it should be a good reference for several years.
Each case is written so that any level of healthcare student would understand. Hyperlinks in the text is also very helpful.
All of the cases are written in a similar fashion.
Although not structured as a typical text, each case is easily assigned as a stand-alone.
Each case is organized clearly in an appropriate manner.
I did not see any issues.
I did not see any grammatical errors
The text seemed appropriately inclusive. There are no pediatric cases and no cases of intellectually-impaired patients, but those types of cases introduce more advanced problem-solving which perhaps exceed the scope of the text. May be a good addition to the text.
I found this text to be an excellent resource for healthcare students in a variety of fields. It would be best utilized in inter professional courses to help guide discussion.
Reviewed by Lynne Umbarger, Clinical Assistant Professor, Occupational Therapy, Emory and Henry College on 11/26/19
While the book does not cover every scenario, the ones in the book are quite common and troublesome for inexperienced allied health students. The information in the book is thorough enough, and I have found the cases easy to modify for educational... read more
While the book does not cover every scenario, the ones in the book are quite common and troublesome for inexperienced allied health students. The information in the book is thorough enough, and I have found the cases easy to modify for educational purposes. The material was easily understood by the students but challenging enough for classroom discussion. There are no mentions in the book about occupational therapy, but it is easy enough to add a couple words and make inclusion simple.
Very nice lab values are provided in the case study, making it more realistic for students.
These case studies focus on commonly encountered diagnoses for allied health and nursing students. They are comprehensive, realistic, and easily understood. The only difference is that the hospital in one case allows the patient's dog to visit in the room (highly unusual in US hospitals).
The material is easily understood by allied health students. The cases have links to additional learning materials for concepts that may be less familiar or should be explored further in a particular health field.
The language used in the book is consistent between cases. The framework is the same with each case which makes it easier to locate areas that would be of interest to a particular allied health profession.
The case studies are comprehensive but well-organized. They are short enough to be useful for class discussion or a full-blown assignment. The students seem to understand the material and have not expressed that any concepts or details were missing.
Each case is set up like the other cases. There are learning objectives at the beginning of each case to facilitate using the case, and it is easy enough to pull out material to develop useful activities and assignments.
There is a quick chart in the Appendix to allow the reader to determine the professions involved in each case as well as the pertinent settings and diagnoses for each case study. The contents are easy to access even while reading the book.
As a person who attends carefully to grammar, I found no errors in all of the material I read in this book.
There are a greater number of people of different ethnicities, socioeconomic status, ages, and genders to make this a very useful book. With each case, I could easily picture the person in the case. This book appears to be Canadian and more inclusive than most American books.
I was able to use this book the first time I accessed it to develop a classroom activity for first-year occupational therapy students and a more comprehensive activity for second-year students. I really appreciate the links to a multitude of terminology and medical lab values/issues for each case. I will keep using this book.
Reviewed by Cindy Krentz, Assistant Professor, Metropolitan State University of Denver on 6/15/19
The book covers eight case studies of common inpatient or emergency department scenarios. I appreciated that they had written out the learning objectives. I liked that the patient was described before the case was started, giving some... read more
The book covers eight case studies of common inpatient or emergency department scenarios. I appreciated that they had written out the learning objectives. I liked that the patient was described before the case was started, giving some understanding of the patient's background. I think it could benefit from having a glossary. I liked how the authors included the vital signs in an easily readable bar. I would have liked to see the labs also highlighted like this. I also felt that it would have been good written in a 'what would you do next?' type of case study.
The book is very accurate in language, what tests would be prudent to run and in the day in the life of the hospital in all cases. One inaccuracy is that the authors called a popliteal artery clot a DVT. The rest of the DVT case study was great, though, but the one mistake should be changed.
The book is up to date for now, but as tests become obsolete and new equipment is routinely used, the book ( like any other health textbook) will need to be updated. It would be easy to change, however. All that would have to happen is that the authors go in and change out the test to whatever newer, evidence-based test is being utilized.
The text is written clearly and easy to understand from a student's perspective. There is not too much technical jargon, and it is pretty universal when used- for example DVT for Deep Vein Thrombosis.
The book is consistent in language and how it is broken down into case studies. The same format is used for highlighting vital signs throughout the different case studies. It's great that the reader does not have to read the book in a linear fashion. Each case study can be read without needing to read the others.
The text is broken down into eight case studies, and within the case studies is broken down into days. It is consistent and shows how the patient can pass through the different hospital departments (from the ER to the unit, to surgery, to home) in a realistic manner. The instructor could use one or more of the case studies as (s)he sees fit.
The topics are eight different case studies- and are presented very clearly and organized well. Each one is broken down into how the patient goes through the system. The text is easy to follow and logical.
The interface has some problems with the highlighted blue links. Some of them did not work and I got a 'page not found' message. That can be frustrating for the reader. I'm wondering if a glossary could be utilized (instead of the links) to explain what some of these links are supposed to explain.
I found two or three typos, I don't think they were grammatical errors. In one case I think the Canadian spelling and the United States spelling of the word are just different.
This is a very culturally competent book. In today's world, however, one more type of background that would merit delving into is the trans-gender, GLBTQI person. I was glad that there were no stereotypes.
I enjoyed reading the text. It was interesting and relevant to today's nursing student. Since we are becoming more interprofessional, I liked that we saw what the phlebotomist and other ancillary personnel (mostly different technicians) did. I think that it could become even more interdisciplinary so colleges and universities could have more interprofessional education- courses or simulations- with the addition of the nurse using social work, nutrition, or other professional health care majors.
Reviewed by Catherine J. Grott, Interim Director, Health Administration Program, TRAILS on 5/5/19
The book is comprehensive but is specifically written for healthcare workers practicing in Canada. The title of the book should reflect this. read more
The book is comprehensive but is specifically written for healthcare workers practicing in Canada. The title of the book should reflect this.
The book is accurate, however it has numerous broken online links.
Relevance/Longevity rating: 3
The content is very relevant, but some links are out-dated. For example, WHO Guidelines for Safe Surgery 2009 (p. 186) should be updated.
The book is written in clear and concise language. The side stories about the healthcare workers make the text interesting.
The book is consistent in terms of terminology and framework. Some terms that are emphasized in one case study are not emphasized (with online links) in the other case studies. All of the case studies should have the same words linked to online definitions.
Modularity rating: 3
The book can easily be parsed out if necessary. However, the way the case studies have been written, it's evident that different authors contributed singularly to each case study.
The organization and flow are good.
Interface rating: 1
There are numerous broken online links and "pages not found."
The grammar and punctuation are correct. There are two errors detected: p. 120 a space between the word "heart" and the comma; also a period is needed after Dr (p. 113).
I'm not quite sure that the social worker (p. 119) should comment that the patient and partner are "very normal people."
There are roughly 25 broken online links or "pages not found." The BC & Canadian Guidelines (p. 198) could also include a link to US guidelines to make the text more universal . The basilar crackles (p. 166) is very good. Text could be used compare US and Canadian healthcare. Text could be enhanced to teach "soft skills" and interdepartmental communication skills in healthcare.
Reviewed by Lindsey Henry, Practical Nursing Instructor, Fletcher on 5/1/19
I really appreciated how in the introduction, five learning objectives were identified for students. These objectives are paramount in nursing care and they are each spelled out for the learner. Each Case study also has its own learning... read more
I really appreciated how in the introduction, five learning objectives were identified for students. These objectives are paramount in nursing care and they are each spelled out for the learner. Each Case study also has its own learning objectives, which were effectively met in the readings.
As a seasoned nurse, I believe that the content regarding pathophysiology and treatments used in the case studies were accurate. I really appreciated how many of the treatments were also explained and rationales were given, which can be very helpful to facilitate effective learning for a nursing student or novice nurse.
The case studies are up to date and correlate with the current time period. They are easily understood.
I really loved how several important medical terms, including specific treatments were highlighted to alert the reader. Many interventions performed were also explained further, which is great to enhance learning for the nursing student or novice nurse. Also, with each scenario, a background and history of the patient is depicted, as well as the perspectives of the patient, patients family member, and the primary nurse. This really helps to give the reader a full picture of the day in the life of a nurse or a patient, and also better facilitates the learning process of the reader.
These case studies are consistent. They begin with report, the patient background or updates on subsequent days, and follow the patients all the way through discharge. Once again, I really appreciate how this book describes most if not all aspects of patient care on a day to day basis.
Each case study is separated into days. While they can be divided to be assigned at different points within the course, they also build on each other. They show trends in vital signs, what happens when a patient deteriorates, what happens when they get better and go home. Showing the entire process from ER admit to discharge is really helpful to enhance the students learning experience.
The topics are all presented very similarly and very clearly. The way that the scenarios are explained could even be understood by a non-nursing student as well. The case studies are very clear and very thorough.
The book is very easy to navigate, prints well on paper, and is not distorted or confusing.
I did not see any grammatical errors.
Each case study involves a different type of patient. These differences include race, gender, sexual orientation and medical backgrounds. I do not feel the text was offensive to the reader.
I teach practical nursing students and after reading this book, I am looking forward to implementing it in my classroom. Great read for nursing students!
Reviewed by Leah Jolly, Instructor, Clinical Coordinator, Oregon Institute of Technology on 4/10/19
Good variety of cases and pathologies covered. read more
Good variety of cases and pathologies covered.
Content Accuracy rating: 2
Some examples and scenarios are not completely accurate. For example in the DVT case, the sonographer found thrombus in the "popliteal artery", which according to the book indicated presence of DVT. However in DVT, thrombus is located in the vein, not the artery. The patient would also have much different symptoms if located in the artery. Perhaps some of these inaccuracies are just typos, but in real-life situations this simple mistake can make a world of difference in the patient's course of treatment and outcomes.
Good examples of interprofessional collaboration. If only it worked this way on an every day basis!
Clear and easy to read for those with knowledge of medical terminology.
Good consistency overall.
Broken up well.
Topics are clear and logical.
Would be nice to simply click through to the next page, rather than going through the table of contents each time.
Minor typos/grammatical errors.
No offensive or insensitive materials observed.
Reviewed by Alex Sargsyan, Doctor of Nursing Practice/Assistant Professor , East Tennessee State University on 10/8/18
Because of the case study character of the book it does not have index or glossary. However it has summary for each health case study outlining key elements discussed in each case study. read more
Because of the case study character of the book it does not have index or glossary. However it has summary for each health case study outlining key elements discussed in each case study.
Overall the book is accurately depicting the clinical environment. There are numerous references to external sites. While most of them are correct, some of them are not working. For example Homan’s test link is not working "404 error"
Book is relevant in its current version and can be used in undergraduate and graduate classes. That said, the longevity of the book may be limited because of the character of the clinical education. Clinical guidelines change constantly and it may require a major update of the content.
Cases are written very clearly and have realistic description of an inpatient setting.
The book is easy to read and consistent in the language in all eight cases.
The cases are very well written. Each case is subdivided into logical segments. The segments reflect different setting where the patient is being seen. There is a flow and transition between the settings.
Book has eight distinct cases. This is a great format for a book that presents distinct clinical issues. This will allow the students to have immersive experiences and gain better understanding of the healthcare environment.
Book is offered in many different formats. Besides the issues with the links mentioned above, overall navigation of the book content is very smooth.
Book is very well written and has no grammatical errors.
Book is culturally relevant. Patients in the case studies come different cultures and represent diverse ethnicities.
Reviewed by Justin Berry, Physical Therapist Assistant Program Director, Northland Community and Technical College, East Grand Forks, MN on 8/2/18
This text provides eight patient case studies from a variety of diagnoses, which can be utilized by healthcare students from multiple disciplines. The cases are comprehensive and can be helpful for students to determine professional roles,... read more
This text provides eight patient case studies from a variety of diagnoses, which can be utilized by healthcare students from multiple disciplines. The cases are comprehensive and can be helpful for students to determine professional roles, interprofessional roles, when to initiate communication with other healthcare practitioners due to a change in patient status, and treatment ideas. Some additional patient information, such as lab values, would have been beneficial to include.
Case study information is accurate and unbiased.
Content is up to date. The case studies are written in a way so that they will not be obsolete soon, even with changes in healthcare.
The case studies are well written, and can be utilized for a variety of classroom assignments, discussions, and projects. Some additional lab value information for each patient would have been a nice addition.
The case studies are consistently organized to make it easy for the reader to determine the framework.
The text is broken up into eight different case studies for various patient diagnoses. This design makes it highly modular, and would be easy to assign at different points of a course.
The flow of the topics are presented consistently in a logical manner. Each case study follows a patient chronologically, making it easy to determine changes in patient status and treatment options.
The text is free of interface issues, with no distortion of images or charts.
The text is not culturally insensitive or offensive in any way. Patients are represented from a variety of races, ethnicities, and backgrounds
This book would be a good addition for many different health programs.
Reviewed by Ann Bell-Pfeifer, Instructor/Program Director, Minnesota State Community and Technical College on 5/21/18
The book gives a comprehensive overview of many types of cases for patient conditions. Emergency Room patients may arrive with COPD, heart failure, sepsis, pneumonia, or as motor vehicle accident victims. It is directed towards nurses, medical... read more
The book gives a comprehensive overview of many types of cases for patient conditions. Emergency Room patients may arrive with COPD, heart failure, sepsis, pneumonia, or as motor vehicle accident victims. It is directed towards nurses, medical laboratory technologists, medical radiology technologists, and respiratory therapists and their roles in caring for patients. Most of the overview is accurate. One suggestion is to provide an embedded radiologist interpretation of the exams which are performed which lead to the patients diagnosis.
Overall the book is accurate. Would like to see updates related to the addition of direct radiography technology which is commonly used in the hospital setting.
Many aspects of medicine will remain constant. The case studies seem fairly accurate and may be relevant for up to 3 years. Since technology changes so quickly in medicine, the CT and x-ray components may need minor updates within a few years.
The book clarity is excellent.
The case stories are consistent with each scenario. It is easy to follow the structure and learn from the content.
The book is quite modular. It is easy to break it up into cases and utilize them individually and sequentially.
The cases are listed by disease process and follow a logical flow through each condition. They are easy to follow as they have the same format from the beginning to the end of each case.
The interface seems seamless. Hyperlinks are inserted which provide descriptions and references to medical procedures and in depth definitions.
The book is free of most grammatical errors. There is a place where a few words do not fit the sentence structure and could be a typo.
The book included all types of relationships and ethnic backgrounds. One type which could be added is a transgender patient.
I think the book was quite useful for a variety of health care professionals. The authors did an excellent job of integrating patient cases which could be applied to the health care setting. The stories seemed real and relevant. This book could be used to teach health care professionals about integrated care within the emergency department.
Reviewed by Shelley Wolfe, Assistant Professor, Winona State University on 5/21/18
This text is comprised of comprehensive, detailed case studies that provide the reader with multiple character views throughout a patient’s encounter with the health care system. The Table of Contents accurately reflected the content. It should... read more
This text is comprised of comprehensive, detailed case studies that provide the reader with multiple character views throughout a patient’s encounter with the health care system. The Table of Contents accurately reflected the content. It should be noted that the authors include a statement that conveys that this text is not like traditional textbooks and is not meant to be read in a linear fashion. This allows the educator more flexibility to use the text as a supplement to enhance learning opportunities.
The content of the text appears accurate and unbiased. The “five overarching learning objectives” provide a clear aim of the text and the educator is able to glean how these objectives are captured into each of the case studies. While written for the Canadian healthcare system, this text is easily adaptable to the American healthcare system.
Overall, the content is up-to-date and the case studies provide a variety of uses that promote longevity of the text. However, not all of the blue font links (if using the digital PDF version) were still in working order. I encountered links that led to error pages or outdated “page not found” websites. While the links can be helpful, continued maintenance of these links could prove time-consuming.
I found the text easy to read and understand. I enjoyed that the viewpoints of all the different roles (patient, nurse, lab personnel, etc.) were articulated well and allowed the reader to connect and gain appreciation of the entire healthcare team. Medical jargon was noted to be appropriate for the intended audience of this text.
The terminology and organization of this text is consistent.
The text is divided into 8 case studies that follow a similar organizational structure. The case studies can further be divided to focus on individual learning objectives. For example, the case studies could be looked at as a whole for discussing communication or could be broken down into segments to focus on disease risk factors.
The case studies in this text follow a similar organizational structure and are consistent in their presentation. The flow of individual case studies is excellent and sets the reader on a clear path. As noted previously, this text is not meant to be read in a linear fashion.
This text is available in many different forms. I chose to review the text in the digital PDF version in order to use the embedded links. I did not encounter significant interface issues and did not find any images or features that would distract or confuse a reader.
No significant grammatical errors were noted.
The case studies in this text included patients and healthcare workers from a variety of backgrounds. Educators and students will benefit from expanding the case studies to include discussions and other learning opportunities to help develop culturally-sensitive healthcare providers.
I found the case studies to be very detailed, yet written in a way in which they could be used in various manners. The authors note a variety of ways in which the case studies could be employed with students; however, I feel the authors could also include that the case studies could be used as a basis for simulated clinical experiences. The case studies in this text would be an excellent tool for developing interprofessional communication and collaboration skills in a variety healthcare students.
Reviewed by Darline Foltz, Assistant Professor, University of Cincinnati - Clermont College on 3/27/18
This book covers all areas listed in the Table of Contents. In addition to the detailed patient case studies, there is a helpful section of "How to Use this Resource". I would like to note that this resource "aligns with the open textbooks... read more
This book covers all areas listed in the Table of Contents. In addition to the detailed patient case studies, there is a helpful section of "How to Use this Resource". I would like to note that this resource "aligns with the open textbooks Clinical Procedures for Safer Patient Care and Anatomy and Physiology: OpenStax" as noted by the authors.
The book appears to be accurate. Although one of the learning outcomes is as follows: "Demonstrate an understanding of the Canadian healthcare delivery system.", I did not find anything that is ONLY specific to the Canadian healthcare delivery system other than some of the terminology, i.e. "porter" instead of "transporter" and a few french words. I found this to make the book more interesting for students rather than deter from it. These are patient case studies that are relevant in any country.
The content is up-to-date. Changes in medical science may occur, i.e. a different test, to treat a diagnosis that is included in one or more of the case studies, however, it would be easy and straightforward to implement these changes.
This book is written in lucid, accessible prose. The technical/medical terminology that is used is appropriate for medical and allied health professionals. Something that would improve this text would to provide a glossary of terms for the terms in blue font.
This book is consistent with current medical terminology
This text is easily divided into each of the 6 case studies. The case studies can be used singly according to the body system being addressed or studied.
Because this text is a collection of case studies, flow doesn't pertain, however the organization and structure of the case studies are excellent as they are clear and easy to read.
There are no distractions in this text that would distract or confuse the reader.
I did not identify any grammatical errors.
This text is not culturally insensitive or offensive in any way and uses patients and healthcare workers that are of a variety of races, ethnicities and backgrounds.
I believe that this text would not only be useful to students enrolled in healthcare professions involved in direct patient care but would also be useful to students in supporting healthcare disciplines such as health information technology and management, medical billing and coding, etc.
Table of Contents
- Introduction
Case Study #1: Chronic Obstructive Pulmonary Disease (COPD)
- Learning Objectives
- Patient: Erin Johns
- Emergency Room
Case Study #2: Pneumonia
- Day 0: Emergency Room
- Day 1: Emergency Room
- Day 1: Medical Ward
- Day 2: Medical Ward
- Day 3: Medical Ward
- Day 4: Medical Ward
Case Study #3: Unstable Angina (UA)
- Patient: Harj Singh
Case Study #4: Heart Failure (HF)
- Patient: Meryl Smith
- In the Supermarket
- Day 0: Medical Ward
Case Study #5: Motor Vehicle Collision (MVC)
- Patient: Aaron Knoll
- Crash Scene
- Operating Room
- Post Anaesthesia Care Unit (PACU)
- Surgical Ward
Case Study #6: Sepsis
- Patient: George Thomas
- Sleepy Hollow Care Facility
Case Study #7: Colon Cancer
- Patient: Fred Johnson
- Two Months Ago
- Pre-Surgery Admission
Case Study #8: Deep Vein Thrombosis (DVT)
- Patient: Jamie Douglas
Appendix: Overview About the Authors
Ancillary Material
About the book.
Health Case Studies is composed of eight separate health case studies. Each case study includes the patient narrative or story that models the best practice (at the time of publishing) in healthcare settings. Associated with each case is a set of specific learning objectives to support learning and facilitate educational strategies and evaluation.
The case studies can be used online in a learning management system, in a classroom discussion, in a printed course pack or as part of a textbook created by the instructor. This flexibility is intentional and allows the educator to choose how best to convey the concepts presented in each case to the learner.
Because these case studies were primarily developed for an electronic healthcare system, they are based predominantly in an acute healthcare setting. Educators can augment each case study to include primary healthcare settings, outpatient clinics, assisted living environments, and other contexts as relevant.
About the Contributors
Glynda Rees teaches at the British Columbia Institute of Technology (BCIT) in Vancouver, British Columbia. She completed her MSN at the University of British Columbia with a focus on education and health informatics, and her BSN at the University of Cape Town in South Africa. Glynda has many years of national and international clinical experience in critical care units in South Africa, the UK, and the USA. Her teaching background has focused on clinical education, problem-based learning, clinical techniques, and pharmacology.
Glynda‘s interests include the integration of health informatics in undergraduate education, open accessible education, and the impact of educational technologies on nursing students’ clinical judgment and decision making at the point of care to improve patient safety and quality of care.
Faculty member in the critical care nursing program at the British Columbia Institute of Technology (BCIT) since 2003, Rob has been a critical care nurse for over 25 years with 17 years practicing in a quaternary care intensive care unit. Rob is an experienced educator and supports student learning in the classroom, online, and in clinical areas. Rob’s Master of Education from Simon Fraser University is in educational technology and learning design. He is passionate about using technology to support learning for both faculty and students.
Part of Rob’s faculty position is dedicated to providing high fidelity simulation support for BCIT’s nursing specialties program along with championing innovative teaching and best practices for educational technology. He has championed the use of digital publishing and was the tech lead for Critical Care Nursing’s iPad Project which resulted in over 40 multi-touch interactive textbooks being created using Apple and other technologies.
Rob has successfully completed a number of specialist certifications in computer and network technologies. In 2015, he was awarded Apple Distinguished Educator for his innovation and passionate use of technology to support learning. In the past five years, he has presented and published abstracts on virtual simulation, high fidelity simulation, creating engaging classroom environments, and what the future holds for healthcare and education.
Janet Morrison is the Program Head of Occupational Health Nursing at the British Columbia Institute of Technology (BCIT) in Burnaby, British Columbia. She completed a PhD at Simon Fraser University, Faculty of Communication, Art and Technology, with a focus on health information technology. Her dissertation examined the effects of telehealth implementation in an occupational health nursing service. She has an MA in Adult Education from St. Francis Xavier University and an MA in Library and Information Studies from the University of British Columbia.
Janet’s research interests concern the intended and unintended impacts of health information technologies on healthcare students, faculty, and the healthcare workforce.
She is currently working with BCIT colleagues to study how an educational clinical information system can foster healthcare students’ perceptions of interprofessional roles.
Contribute to this Page
Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
Nursing Case Study

For accessible versions of these activities, please refer to our document Step 1: Ask – Accessible Case Studies .
Evidence-Based Practice Copyright © by Various Authors - See Each Chapter Attribution is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License , except where otherwise noted.

How to Write a Case Study Paper for Nursing
A well-written case study paper for a nursing program requires some planning and consideration. All too often, students begin writing before they complete appropriate, preliminary steps. Ideally, before you start a paper, you should already have determined the focus and format of it. You will then follow this up with a fact-gathering step in which you will gather and collate the content of your paper. Finally, there is the construction/execution step in which you will write the paper in a standard format (such as the APA style) and edit it.
A nursing case study paper contains several sections that fall into three categories:
1. The status of the patient
- Demographic data
- Medical History
- Current diagnosis and treatment
2. The nursing assessment of the patient
- Vital signs and test results
- Nursing observations (i.e., range of motion, mental state)
3. Current Care Plan and Recommendations
- Details of the nursing care plan (including nursing goals and interventions)
- Evaluation of the current care plan
- Recommendations for changes in the current care plan
Patient Status
The first portion of the case study paper will talk about the patient — who they are, why they are being included in the study, their demographic data (i.e., age, race), the reason(s) they sought medical attention and the subsequent diagnosis. It will also discuss the role that nursing plays in the care of this patient.
Next, thoroughly discuss any disease process. Make sure you outline causes, symptoms, observations, and how preferred treatments can affect nursing care. Also, describe the history and progression of the disease. Some important questions for you to answer are: 1) What were the first indications that there was something wrong, and 2) What symptoms convinced the patient to seek help?
Nursing Assessment
When you are discussing the nursing assessment of the patient, describe the patientΓÇÖs problems in terms of nursing diagnoses. Be specific as to why you have identified a particular diagnosis. For example, is frequent urination causing an alteration in the patientΓÇÖs sleep patterns? The nursing diagnoses you identify in your assessment will help form the nursing care plan.
Current Care Plan and Recommendations for Improvement
Describe the nursing care plan and goals, and explain how the nursing care plan improves the quality of the patientΓÇÖs life. What positive changes does the nursing care plan hope to achieve in the patientΓÇÖs life? How will the care plan be executed? Who will be responsible for the delivery of the care plan? What measurable goals will they track to determine the success of the plan?
The final discussion should be your personal recommendations. Based on the current status of the patient, the diagnosis, prognosis, and the nursing care plan, what other actions do you recommend can be taken to improve the patientΓÇÖs chances of recovery? You must support your recommendations with authoritative sources and cite appropriately per APA style guidelines.
Creating a well-written nursing case study paper doesnΓÇÖt need to be a grueling challenge. It can be gratifying, and itΓÇÖs good practice for assessing patients while out in the field, too. Keep in mind that your instructor will not only grade you on the quality of the content of your paper but by how you apply the APA style, as well. If you find that you are spending too much time formatting your paper, consider using formatting software as a helpful tool to ensure accuracy, so you donΓÇÖt lose points on a well-written paper because of some formatting errors.
For more information about APA or MLA formats, contact us today.
David Plaut
David Plaut is the founder of Reference Point Software (RPS). RPS offers a complete suite of easy-to-use formatting template products featuring MLA and APA style templates, freeing up time to focus on substance while ensuring formatting accuracy. 
Reference Point Software is not associated with, endorsed by, or affiliated with the American Psychological Association (APA) or with the Modern Language Association (MLA).
Tags: medical writing tips , nurse writing tips , reference point software
Comments are closed.

Nursing Case Study Examples and Solutions
- Premium Academia
- August 17, 2023
- Nursing Essay Examples
NursingStudy.org is your ultimate resource for nursing case study examples and solutions. Whether you’re a nursing student, a seasoned nurse looking to enhance your skills, or a healthcare professional seeking in-depth case studies, our comprehensive collection has got you covered. Explore our extensive category of nursing case study examples and solutions to gain valuable insights, improve your critical thinking abilities, and enhance your overall clinical knowledge.
Comprehensive Nursing Case Studies
Discover a wide range of comprehensive nursing case study examples and solutions that cover various medical specialties and scenarios. These meticulously crafted case studies offer real-life patient scenarios, providing you with a deeper understanding of nursing practices and clinical decision-making processes. Each case study presents a unique set of challenges and opportunities for learning, making them an invaluable resource for nursing education and professional development.
- Nursing Case Study Analysis [10 Examples & How-To Guides] What is a case study analysis? A case study analysis is a detailed examination of a specific real-world situation or event. It is typically used in business or nursing school to help students learn how to analyze complex problems and make decisions based on limited information.
- State three nursing diagnoses using taxonomy of North American Nursing Diagnosis Association (NANDA) that are appropriate, formatted correctly, prioritized, and are based on the case study. NUR 403 Week 2 Individual Assignment Case Study comprises: Resources: The case study found on p. 131 in Nursing Theory and the Case Study Grid on the Materials page of the student website Complete the Case Study Grid. List five factors of patient history that demonstrates nursing needs.
- Neuro Case Study
- Endocrine Case Study
- Anxiety & Depression Case Study
- Ethical dilemma
- A Puerto Rican Woman With Comorbid Addiction
- Tina Jones Comprehensive SOAP Note
- Insomnia 31 year old Male
- Chest Pain Assessment
Pediatric Nursing Case Studies

In this section, delve into the world of pediatric nursing through our engaging and informative case studies. Gain valuable insights into caring for infants, children, and adolescents, as you explore the complexities of pediatric healthcare. Our pediatric nursing case studies highlight common pediatric conditions, ethical dilemmas, and evidence-based interventions, enabling you to enhance your pediatric nursing skills and deliver optimal care to young patients.
- Case on Pediatrics : Part 1& 2 Solutions
- Pediatric Infant Reflux : History and Physical – Assignment 1 Solution
- Otitis Media Pediatrics Toddler – NSG 5441 Reflection Assignment/Discussion – Solution
- Pediatric Patient With Strep – NSG 5441 Reflection Assignment/Discussion
- Pediatric Urinary Tract infections (UTI) -NSG 5441 Reflection Assignment/Discussion – Solution
- Week 3 discussion-Practical Application in critical care/pediatrics
- Cough Assessmen t
Mental Health Nursing Case Study Examples
Mental health nursing plays a crucial role in promoting emotional well-being and providing care for individuals with mental health conditions. Immerse yourself in our mental health nursing case studies, which encompass a wide range of psychiatric disorders, therapeutic approaches, and psychosocial interventions. These case studies offer a holistic view of mental health nursing, equipping you with the knowledge and skills to support individuals on their journey to recovery.
- Psychiatric Nursing: Roles and Importance in Providing Mental Health Care
- Mental Health Access and Gun Violence Prevention
- Fundamentals of neurotransmission as it relates to prescribing psychotropic medications for clients with acute and chronic mental health conditions – Unit 8 Discussion – Reflection
- Unit 7 Discussion- Complementary and Alternative Medicine in Mental Health Care – Solution
- Ethical and Legal Foundations of PMHNP Care Across the Lifespan Assignment – Analyze salient ethical and legal issues in psychiatric-mental health practice | Solution
- Pathways Mental Health Case Study – Review evaluation and management documentation for a patient and perform a crosswalk of codes – Solution
- Analyze salient ethical and legal issues in psychiatric-mental health practice
- SOAP notes for Mental Health Examples
- compare and contrast two mental health theories
- Environmental Factors and Health Promotion Presentation: Accident Prevention and Safety Promotion for Parents and Caregivers of Infants
Geriatric Nursing Case Studies
As the population ages, the demand for geriatric nursing expertise continues to rise. Our geriatric nursing case studies focus on the unique challenges faced by older adults, such as chronic illnesses, cognitive impairments, and end-of-life care. By exploring these case studies, you’ll develop a deeper understanding of geriatric nursing principles, evidence-based gerontological interventions, and strategies for promoting optimal health and well-being in older adults.
- M5 Assignment: Elderly Driver
- HE003: Delivery of Services – Emmanuel is 55-year-old man Case – With Solution The Extent of Evidence-Based Data for Proposed Interventions – Sample Assignment 1 Solution
- Planning Model for Population Health Management Veterans Diagnosed with Non cancerous chronic pain – Part 1 & 2 Solutions
- PHI 413 Case Study Fetal Abnormality Essay
- Insomnia Response and Insomnia
- Analysis of a Pertinent Healthcare Issue: Short Staffing
- Paraphrenia as a Side of the Schizophrenia – Week 4 Solution
- Module 6 Pharm Assignment: Special Populations
- Public Health Nursing Roles and Responsibilities in Disaster Response – Assignment 2 Solution
- Theory Guided Practice – Assignment 2 Solution
- How can healthcare facilities establish a culture of safety – Solution
- Discuss the types of consideration a nurse must be mindful of while performing a health assessment on a geriatric patient as compared to a middle-aged adult – Solution
- Promoting And Protecting Vulnerable Populations – Describe what is meant by vulnerable populations and explain strategies you, as the public health nurse, could use to best facilitate the achievement of healthful outcomes in this population?
Community Health Nursing Case Studies
Community health nursing plays a vital role in promoting health, preventing diseases, and advocating for underserved populations. Dive into our collection of community health nursing case studies, which explore diverse community settings, public health issues, and population-specific challenges. Through these case studies, you’ll gain insights into the role of community health nurses, interdisciplinary collaboration, health promotion strategies, and disease prevention initiatives.
- Community and Target Aggregate: Residents of the community health center, particularly those aged 65 and above Topic: Secondary Prevention/Screenings for a Vulnerable Population
- Tools For Community Health Nursing Practice2
- 5 Theories in Community Health Nursing: A Complete Guide
- Role of community health nursing and community partnerships as they apply to the participating family’s community – Assignment 1 Solution
- Community/Public Health Nursing DQ2
- CSU-Community healthcare Presentation – Assignment 1 Solution
- Community Healthcare Presentation – Domestic Violence And Level Of Prevention – Solution
Critical Care Nursing Case Study Examples
Critical care nursing demands swift decision-making, advanced technical skills, and the ability to provide intensive care to acutely ill patients. Our critical care nursing case studies encompass a range of high-acuity scenarios, including trauma, cardiac emergencies, and respiratory distress. These case studies simulate the fast-paced critical care environment, enabling you to sharpen your critical thinking skills, enhance your clinical judgment, and deliver exceptional care to critically ill patients.
- Nursing Case Study Parkinsons Disease
- Nursing Case Study: Patient with Drug and Alcohol Induced Paranoid Schizophrenia
- Neonatal Hypothermia and Neonatal Sepsis: Nursing Case Study
- Chronic Obstructive Pulmonary Disease Nursing Case Study
Maternal and Child Health Nursing Case Study Examples
The field of maternal and child health nursing requires specialized knowledge and skills to support the health and well-being of women and children throughout their lifespan. Explore our collection of maternal and child health nursing case studies, which encompass prenatal care, labor and delivery, postpartum care, and pediatric nursing. These case studies provide a comprehensive view of maternal and child health, allowing you to develop expertise in this essential area of nursing practice.
You can also check out Patient Safety in High-Tech Settings PICOT Questions Examples
Surgical Nursing Case Studies
Surgical nursing involves caring for patients before, during, and after surgical procedures. Our surgical nursing case studies cover a wide range of surgical specialties, including orthopedics, cardiovascular, and gastrointestinal surgeries. Delve into these case studies to gain insights into preoperative assessment, perioperative management, and postoperative care. By examining real-life surgical scenarios, you’ll develop a comprehensive understanding of surgical nursing principles and refine your skills in providing exceptional care to surgical patients.
- Discuss DI in relation to a postoperative neurosurgical patient – Week 2, 3, 4 Solution
- DISCUSSION WK 3
- Career Planning & Professional Identity Paper
- N ursing Case Analysis
- Ethical Dilemma on Robotic Surgery and ACS Codes of Ethics – Post 2
- NURS – 6521C Advanced Pharmacology
- Essay on Alterations in Neurological and Endocrine Functions
- Clinical Preparation Tool – Child and Adolescent Symptom Inventory – Unit
- Initial Psychiatric Interview/SOAP Note – Assignment 1 Solution
- Current Trends in Nursing Practice: Electronic Prescriptions for Opioids – Week 4 Solution
- Nurse-Sensitive Indicators -Week 3 Solution
- Theory–Practice Gap in Jean Watson Theory of Human Caring – Assignment 1 Solution
- Bowel Obstruction Case Video Presentation – Week 4 Solution
- Appendicitis SOAP Note – Sample SOAP Solution 1
- Week 4: GERD SOAP Note Assignment Solution
Obstetric Nursing Case Study
Obstetric nursing focuses on providing care to women during pregnancy, childbirth, and the postpartum period. Our obstetric nursing case studies explore various aspects of prenatal care, labor and delivery, and postpartum recovery. Gain valuable knowledge about common obstetric complications, evidence-based interventions, and strategies for promoting maternal and fetal well-being. These case studies will enhance your obstetric nursing skills and prepare you to deliver compassionate and competent care to expectant mothers.
- Capstone Proposal: Postpartum Hemorrhage Education To Nursing Students
- Progress Evaluation Telecommunication: Teleconference on Post-Partum Hemorrhage
- Case Study 5.2 the Moral and Ethical Questions of Aborting an Anencephalic Baby
- Holistic intervention plan design to improve the quality of outcomes – Problem Statement (PICOT)
- ADV HEALTH ASSESSMENT: TJ a 32-year-old pregnant lesbian, is being seen for an annual physical exam and has been having vaginal discharge – Solution
- Facilitative Communication and Helping Skills in Nursing & Decision Making Assignment Solution
- Benchmark – Evidence-Based Practice Proposal Paper Example
- Three nursing diagnoses for this client based on the health history and screening (one actual nursing diagnosis, one wellness nursing diagnosis, and one “risk for” nursing diagnosis)
- Identify two or more issues with the existing system
- Differences between inpatient and outpatient coding
Nursing Ethics Case Study
Ethical dilemmas are an inherent part of nursing practice. Our nursing ethics case studies shed light on complex ethical issues that nurses encounter in their daily work. Explore thought-provoking scenarios involving patient autonomy, confidentiality, end-of-life decisions, and resource allocation. By examining these case studies, you’ll develop a deeper understanding of ethical principles, ethical decision-making frameworks, and strategies for navigating ethical challenges in nursing practice.
- Ethics in Complementary Therapies
- Ethics Case Study Analysis
- Ethics in Practice
- Ethical Dilemma on Robotic Surgery and ACS Codes of Ethics – Post 1
- Case Study on Biomedical Ethics in the Christian Narrative
- Academic Success and Professional Development Plan Part 2: Strategies to Promote Academic Integrity and Professional Ethics
- Week 9 Assignment 9.1: Mercy Killing Ethics – Using one theory that you have studied that you agree with and one theory that you disagree with, describe how Officer Jones would act in each case – Solution
- Deliverable 4 – Code of Ethics Intake Packet
- Ethics in the Workplace
- code of ethics for nurses
- Applying the ANA Code of Ethics
Health Promotion Case Study
Community health promotion plays a crucial role in improving the health and well-being of populations. Our community health promotion case studies highlight successful initiatives aimed at preventing diseases, promoting healthy lifestyles, and addressing social determinants of health. Explore strategies for community engagement, health education, and collaborative interventions that make a positive impact on the well-being of individuals and communities.
- Health Promotion in Minority Populations
- Environmental Factors and Health Promotion Presentation: Accident Prevention and Safety Promotion for Parents and Caregivers of Infants
- Health Education And Current Challenges For Family-Centered Health Promotion
- Cultural Competence And Nutrition In Health Promotion
- Why is the concept of family health important? Consider the various strategies for health promotion.
- levels of health promotion
- Integrate evidence from research and theory into discussions of practice competencies, health promotion and disease prevention strategies, quality improvement, and safety standards.
- Discuss various theories of health promotion, including Pender’s Health Promotion Model, the Health Belief Model, the Transtheoretical Theory, and the Theory of Reasoned Action.
- What strategies, besides the use of learning styles, can a nurse educator consider when developing tailored individual care plans, or for educational programs in health promotion?
- Describe health promotion for Pregnant women
- Identify a health problem or need for health promotion for a particular stage in the life span of a population from a specific culture in your area. Choose one of the Leading Health Indicators (LHI) priorities from Healthy People 2020: https://www.healthypeople.gov/2020/Leading-Health-Indicators
- A description of a borrowed theory (expectancy-value theory and social cognitive theory) that could be applied to improve health promotion patient education in primary care clinic. Is this borrowed theory appropriate?
- How has health promotion changed over time
- Primary Prevention/Health Promotion
- Health Risk Assessment and Health Promotion Contract
Nursing Leadership Case Studies
Nursing leadership is essential for driving positive change and ensuring high-quality patient care. Our nursing leadership case studies examine effective leadership strategies, change management initiatives, and interprofessional collaboration in healthcare settings. Gain insights into the qualities of successful nurse leaders, explore innovative approaches to leadership, and learn how to inspire and motivate your team to achieve excellence in nursing practice.
- Part 3: Nursing Leadership – Childbearing after menopause – Assignment Solution
- Capstone Project Ideas for Nursing Leadership
- The purpose of this assignment is to examine the impact of contemporary challenges in care delivery facing nursing leadership. Select and research a major issue in the delivery of care facing nurse leaders today and write a 1,250-1,500 word paper addressing the following:
- One nursing theory will be presented as a framework to resolve a problem occurring within one of the professional areas of leadership, education, informatics, healthcare policy or advance clinical practice. The same nursing theory selected in Assignment One may be used to resolve the identified problem.
- Module 6: Change and Leadership in Nursing Education – Professional Development
- Module 6: Change and Leadership in Nursing Education – Critical Thinking
- Module 6: Change and Leadership in Nursing Education – Discussion
- Analyze one of the following concepts: “Advanced Practice Nursing,” “Leadership in Nursing Practice” or “Holistic Nursing Practice”
- Nursing Administration Function: A Comprehensive Guide for Nursing Students
- Theory and Leadership
- NUR-514: Organizational Leadership and Informatics
- Leadership: Workplace Environment Assessment
- Professional Development in Nursing – Topic 3 Assignment Solution
- Leadership Change Framework – Week 8 Assignment Solution
At NursingStudy.org, we strive to provide you with a comprehensive collection of nursing case study examples and solutions that align with the best practices recommended by YOAST and RankMath. By exploring these diverse case studies, you’ll enhance your clinical knowledge, critical thinking abilities, and overall understanding of nursing practice. Take advantage of this valuable resource and elevate your nursing skills to new heights.
Remember, success in nursing begins with knowledge and continues with lifelong learning. Explore our nursing case study examples and solutions today and embark on a journey of professional growth and excellence.
Working On an Assignment With Similar Concepts Or Instructions?
A Page will cost you $12, however, this varies with your deadline.
We have a team of expert nursing writers ready to help with your nursing assignments. They will save you time, and improve your grades.
Whatever your goals are, expect plagiarism-free works, on-time delivery, and 24/7 support from us.
Here is your 15% off to get started. Simply:
- Place your order ( Place Order )
- Click on Enter Promo Code after adding your instructions
- Insert your code – Get20
All the Best,
Have a subject expert Write for You Now
Have a subject expert finish your paper for you, edit my paper for me, have an expert write your dissertation's chapter, what you'll learn.
- Nursing Paper Examples
Related Posts
- Personal Philosophy Statement Example for a PMHNP
- Leadership Strategies for Success-Nursing Paper Examples
- Applying the Scientific Method-Nursing Paper Examples
Important Links
Knowledge base, paper examples, nursing writing services.
Nursingstudy.org helps students cope with college assignments and write papers on various topics. We deal with academic writing, creative writing, and non-word assignments.
All the materials from our website should be used with proper references. All the work should be used per the appropriate policies and applicable laws.
Our samples and other types of content are meant for research and reference purposes only. We are strongly against plagiarism and academic dishonesty.
Phone: +1 628 261 0844
Mail: [email protected]

We Accept:

@2015-2024, Nursingstudy.org
- More On the 6 Components of the Ongoing Case Study

Nursing Career Guide
A Deep Dive into the Six Components of the NCLEX-NGN Ongoing Case Studies
Need help understanding the six components of the Ongoing Case Studies that are part of NCLEX-NGN? We’re here to walk you through each of them so you can feel confident when you sit for your examination.
The Ongoing Case Studies are designed to simulate an actual case that you might encounter in a clinical setting. Rather than simply test the knowledge that you acquired in nursing school—which is also important—the case study progresses from your first interaction with a client through your evaluation of the outcomes.
We told you about the reasoning behind NCLEX-NGN and the implementation of the Clinical Judgment Measurement Model . And we provided a brief description of the six components that you’ll be asked to analyze, using your cognitive skills—not just the “perfect world” situations that textbooks provide.
Recognize cues
The nurse reviews all client findings and determines which data are relevant and important, focusing on cues (findings or assessments) that are of IMMEDIATE CONCERN.
You consider every bit of information in the initial scenario, including things like medical-social history, mental status, developmental stage, diagnosis, and current symptoms. No two clients are the same, so what is abnormal for one client may be acceptable for another. For example, an O2 saturation of 90% means hypoxia for most people but is in the normal range for a client with COPD.
The question: What matters most?
Tips for recognizing cues:.
- This is only the first step—do not interpret or analyze yet. Don’t try to figure out what the findings could mean or what you, as the nurse, will do. Simply sort through all the data and look for items that are normal/usual, abnormal but expected (not relevant), or abnormal but unexpected (relevant).
- When you decide that a finding is abnormal or unexpected, look at the client and the scenario. If it’s expected (as with the O2 saturation of 90% for a client with COPD) then it’s probably not relevant.
- Are MOST important
- Of IMMEDIATE concern
- REQUIRE follow-up.
- Even if a client finding is relevant, it may not be a priority. Example: A client presents to the ED with crushing chest pain; the client also has diabetes. Diabetes is an abnormal finding, so it’s relevant, but NOT the priority in this scenario.
Analyze Cues
With relevant cues sorted out, now the nurse can begin to interpret what the cues can mean. By analyzing the factors in the clinical scenario, you can start to fit them into the case. Now you will think about what is happening and possible complications for the client.
Now you analyze the cues that you have recognized; this will be the basis for the rest of the Ongoing Case Study as you begin to plan and prioritize the client’s needs and how you will meet them. To do this, you’ll require knowledge of health conditions and how they relate to the client’s current situation. You will also have to know about diagnostic tests and what the results can indicate.
The question: What does it mean?
Tips for analyzing cues:.
- Go back to the relevant cues you found in Recognize Cues.
- Link the cues to possible client conditions that match with your findings and cues.
- All client findings are important but concentrate on those that are not normal or not expected. These are the findings to analyze.
- Determine if the findings tell what is happening to the client: Do they support or oppose any conditions?
- Decide if you need more information to make an accurate analysis or understand the clinical situation.
Prioritize Hypotheses
Now the nurse is ready to make predictions (hypotheses) in order to prioritize client needs. You’ve looked at all the data and considered all the possibilities for what the client is experiencing. It’s time to rank the hypotheses according to their urgency, as well as the risks that the client faces.
You look for all explanations and decide which ones are most likely, as well as those that are least likely. As you prioritize, you will use your cognitive skills to decide which problems or issues require IMMEDIATE attention and which ones can be postponed for the moment.
The question: Where do I start?
Tips for prioritizing hypotheses:.
- This is the time to use your nursing education knowledge! You already have the information you need to think critically and prioritize.
- Prioritizing includes considering all factors, not just the client’s condition. Your plan will change depending on where it occurs (A physician’s office is different from an Emergency Department, which is different from an outpatient facility), as well as what resources are available. (Is your unit fully staffed? Do you have services such as Radiology and Respiratory Therapy? Are the client’s Medical Records available?)
- Look at your own level of knowledge and skills. A nurse with 5, 10, or 20 years of experience can handle more complex situations than a new graduate. Consider your expertise in performing tasks. You can’t plan for something you don’t yet know how to do.
- High/Top Priority: Life-threatening or can result in harm to the client
- Intermediate/Middle: Not an emergency/not life-threatening, but important. It may be serious but can wait while High Priorities are met.
- Low/Last Priority: Not directly related to the client’s current situation, is not urgent and can wait until High and Intermediate needs are met.
- ABCs: Always, always include Airway, Breathing, and Circulation in your prioritization. The exception: Cardiopulmonary resuscitation uses CAB: Circulation (compressions), Airway, and Breathing.
- Focus on the information you’re provided in the scenario. Everything you need to answer the test item is included. Don’t wish you had more data.
Generate Solutions
It’s time for the nurse to generate the plan of care and identify appropriate interventions that will lead to positive client outcomes. You’re now using your nursing knowledge and evidence-based practice to generate solutions based on the priorities you’ve established.
As you provide care for your clients, look at the plan of care that was created from the hypotheses and compare it to the client’s status. Determine if the interventions are still appropriate or if they need to be revised. Ask yourself if they will achieve the best outcomes for the client.
Question: What can I do?
Tips for generating solutions:.
- Identify the expected outcomes and determine if the established priorities will achieve those outcomes.
- Be prepared to see test items that ask about interventions based on your assessments, and any interventions that are nursing actions.
- Consider actions that are indications or contraindications.
- Think about the case study scenario and what potential risks and complications for the client.
- Identify contributing factors such as medications, sleep, infection, hydration, surroundings, and ability to communicate.
Take Action
Taking action means performing appropriate activities that benefit the client and lead to desired outcomes. Actions can include things like maintaining stability, improving a situation, preventing a complication, or recognizing and managing an emergency.
Choosing a nursing action is the equivalent of implementing nursing care. You’re meeting the client’s needs based on the priorities that you’ve established. You’re also demonstrating that you know what actions to take in the situation to keep the client safe and comfortable.
Question: What will I do?
Tips for taking action:.
- Expect to see many test items on nursing actions. Questions may be about nursing interventions or performing nursing skills.
- Pay attention to the information provided in the scenario. Every test item has everything you need to determine the correct (key) response.
- Always focus on the needs of your clients and what actions you will take to meet those needs.
- Before taking an action, pause to consider the scenario: What is happening with a client and what the priorities of care are.
- Decide if an action is appropriate and relevant for the client, based on their medical condition and the clinical setting.
Evaluate Outcomes
The nurse is constantly evaluating outcomes and modifying care to meet those goals. The nurse also communicates to the health care team, the client, and the client’s family regarding the plan of care.
Based on the evaluations, the nurse can continue the current plan of care or make revisions if it’s not effective or the goals have only been partially met. A plan of care doesn’t always proceed in a linear fashion and can require multiple adjustments to reach the desired outcomes.
Question: Did it help?
Tips for evaluating outcomes:.
- Focus on the expected outcomes and think if they were met or not. If not, try to decide what needs to be done in order to meet them.
- If outcomes were not met, or partially met, return to the first five steps and see if something was forgotten or misidentified. Examine if the expected outcomes were consistent with earlier assessments findings.
- You can be asked about specific findings, such as lab values, vital signs, or body systems. Remember that normal findings may not be relevant to the case study scenario.
- Look at client education to see if the client has understood your teaching or if more education is needed. If there is a lack of understanding, further follow-up is indicated.
Once you’re able to understand how the Unfolding Case Study progresses from noticing cues about the client’s situation, all the way to evaluating the interventions, the process will become familiar. The steps are logical and align with your knowledge from nursing school. Don’t be intimidated by the case studies. Practice taking them so you’re confident when you sit for your NCLEX.

About the Author
Winona Suzanne Ball
Nursing Adviser, RN | MHS, Governors State University, IL Full member of the American Nurses Association. Learn more
More help for you
How much nurses make
How to become a Registered Nurse
NCLEX terminology
NCLEX Exam Simulator
Preparing for your NCLEX RN or PN? Sure you can study the dusty textbooks, but they don’t give you a pass guarantee. We do. Pass using our fast and efficient method, or your Premium membership is free.

What’s Your Time and Sanity Worth?
Sure you can study the dusty textbooks, but they don’t give you a pass guarantee. We do. Pass your NCLEX exam using our fast and efficient method, or it’s free.


Nursing Case Study
Ai generator.
ScienceDirect posted a nursing ethics case study where an end-stage prostate cancer patient, Mr. Green, confided to nursing staff about his plan to commit suicide. The patient asked the nurse to keep it a secret. The ethical problem is whether the nurse should tell the health care team members about the patient’s thought without his permission. The best ethical decision for this nursing case study was to share this critical information with other health care professionals, which was the action the nurse took. The team adhered to the proper self-harm and suicide protocol. The appropriate team performed a palliative therapy. As a result, the patient didn’t harm himself and died peacefully a few months after he was discharged.
What Is a Nursing Case Study? A nursing case study is a detailed study of an individual patient. Through this type of research, you can gain more information about the symptoms and the medical history of a patient. It will also allow you to provide the proper diagnoses of the patient’s illness based on the symptoms he or she experienced and other affecting factors. Nursing students usually perform this study as part of their practicum, making it an essential experience because, through this research methodology , they can apply the lessons they have learned from school. The situation mentioned above was an excellent example of a nursing case study.
Nursing Case Study Format
1. introduction.
Purpose: Briefly introduces the case study, including the main health issue or condition being explored. Background: Provides context for the patient scenario, outlining the significance of the case in nursing practice. Objectives: Lists the learning objectives or goals that the case study aims to achieve.
2. Patient Information
Demographics: Age, gender, ethnicity, and relevant personal information. Medical History: Past medical history, including any chronic conditions, surgeries, or significant health events. Current Health Assessment: Presents the patient’s current health status, including symptoms, vital signs, and results from initial examinations.
3. Case Description
Clinical Presentation: Detailed description of the patient’s presentation, including physical examination findings and patient-reported symptoms. Diagnostic Findings: Summarizes diagnostic tests that were performed, including lab tests, imaging studies, and other diagnostic procedures, along with their results. Treatment Plan: Outlines the initial treatment provided to the patient, including medications, therapies, surgeries, or other interventions.
4. Nursing Care Plan
Nursing Diagnoses: Identifies the nursing diagnoses based on the assessment data. Goals and Outcomes: Establishes short-term and long-term goals for the patient’s care, including expected outcomes. Interventions: Describes specific nursing interventions planned or implemented to address each nursing diagnosis and achieve the stated goals. Evaluation: Discusses the effectiveness of the nursing interventions, including patient progress and any adjustments made to the care plan.
5. Analysis
Critical Analysis: Analyzes the case in depth, considering different aspects of patient care, decision-making processes, and the application of nursing theories and principles. Reflection: Reflects on the nursing practice, lessons learned, and how the case study has impacted the understanding and application of nursing knowledge.
6. Conclusion
Summary: Provides a concise summary of the key points from the case study, including the patient outcome and the nursing care impact. Implications for Practice: Discusses the implications of the case for nursing practice, including any changes to practice or policy that could improve patient care. Recommendations: Offers recommendations for future care or areas for further study based on the case study findings.
Examples of Nursing Case Study
Management of Acute Myocardial Infarction (AMI) Introduction: A 58-year-old male with a history of hypertension and smoking presents to the emergency department with chest pain. This case study explores the nursing management for patients with AMI. Patient Information: Demographics: 58-year-old male, smoker. Medical History: Hypertension, no previous diagnosis of heart disease. Current Health Assessment: Reports severe chest pain radiating to his left arm, sweating, and nausea. Case Description: Clinical Presentation: Patient appeared in distress, clutching his chest. Diagnostic Findings: ECG showed ST-elevation in anterior leads. Troponin levels were elevated. Treatment Plan: Immediate administration of aspirin, nitroglycerin, and morphine for pain. Referred for emergency coronary angiography. Nursing Care Plan: Nursing Diagnoses: Acute pain related to myocardial ischemia. Goals: Relieve pain and prevent further myocardial damage. Interventions: Monitoring vital signs, administering prescribed medications, and providing emotional support. Evaluation: Pain was managed effectively, and the patient was stabilized for angiography. Analysis: The timely nursing interventions contributed to stabilizing the patient’s condition, showcasing the critical role nurses play in acute care settings. Conclusion: This case highlights the importance of quick assessment and intervention in patients with AMI, emphasizing the nurse’s role in pain management and support.
Managing Type 1 Diabetes in a Pediatric Patient Introduction: A 10-year-old female diagnosed with type 1 diabetes presents for a routine check-up. This case study focuses on the nursing care plan for managing diabetes in pediatric patients. Patient Information: Demographics: 10-year-old female. Medical History: Diagnosed with type 1 diabetes six months ago. Current Health Assessment: Well-controlled blood glucose levels, but expresses difficulty with frequent insulin injections. Case Description: Clinical Presentation: Patient is active, engaging in school activities but struggles with diabetes management. Diagnostic Findings: HbA1c is 7.2%, indicating good control. Treatment Plan: Insulin therapy, carbohydrate counting, and regular blood glucose monitoring. Nursing Care Plan: Nursing Diagnoses: Risk for unstable blood glucose levels. Goals: Maintain blood glucose within target range and increase patient comfort with diabetes management. Interventions: Education on insulin pump use, dietary advice, and coping strategies. Evaluation: Patient showed interest in using an insulin pump and understood dietary recommendations. Analysis: This case emphasizes the importance of education and emotional support in managing chronic conditions in pediatric patients. Conclusion: Effective management of type 1 diabetes in children requires a comprehensive approach that includes education, technological aids, and psychological support.
Elderly Care for Alzheimer’s Disease Introduction: An 82-year-old female with Alzheimer’s disease presents with increased confusion and agitation. This case study examines the complexities of caring for elderly patients with Alzheimer’s. Patient Information: Demographics: 82-year-old female. Medical History: Alzheimer’s disease, osteoarthritis. Current Health Assessment: Increased confusion, agitation, and occasional aggression. Case Description: Clinical Presentation: Patient exhibits signs of advanced Alzheimer’s with memory loss and disorientation. Diagnostic Findings: Cognitive tests confirm the progression of Alzheimer’s. Treatment Plan: Non-pharmacological interventions for agitation, memory aids, and safety measures in the home. Nursing Care Plan: Nursing Diagnoses: Impaired memory related to Alzheimer’s disease. Goals: Reduce agitation and prevent harm. Interventions: Use of calming techniques, establishing a routine, and environmental modifications. Evaluation: Agitation was reduced, and the patient’s safety was improved through environmental adjustments. Analysis: The case underscores the need for tailored interventions to manage Alzheimer’s symptoms and improve the quality of life for the elderly. Conclusion: Nursing care for Alzheimer’s patients requires a multifaceted approach focusing on safety, symptom management, and patient dignity.
Nursing Case Study Topics with Samples to Edit & Download
- Telehealth Nursing
- Mental Health and Psychiatric Nursing
- Geriatric Nursing Care
- Palliative and End-of-Life Care
- Pediatric Nursing
- Emergency and Critical Care Nursing
- Chronic Disease Management
- Nursing Ethics and Patient Rights
- Infection Control and Prevention
- Oncology Nursing
- Nursing Leadership and Management
- Cultural Competence in Nursing
- Substance Abuse and Addiction Nursing
- Technological Innovations in Nursing
- Nursing Education and Training
Nursing Case Study Examples & Templates
1. nursing case study template.
2. Free Nursing Student Care Plan Template
3. Nursing Action Case Study Example
4. Hospital Nursing Care Case Study Example
5. Printable Nursing Health Case Study Example
professays.com
6. Fundamentals of Nursing Case Study Example
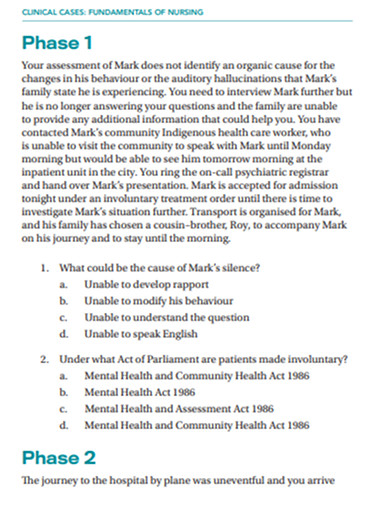
secure-ecsd.elsevier.com
7. Sample Nursing Case Study Example
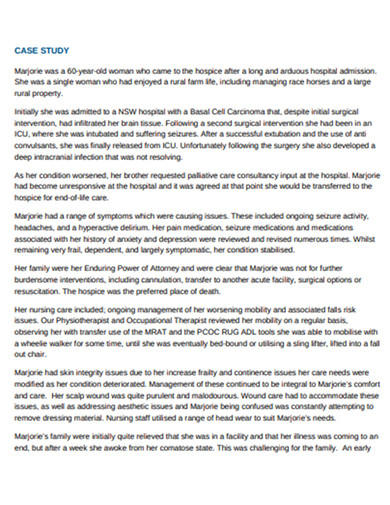
caresearch.com.au
8. Nursing Research Case Study Example
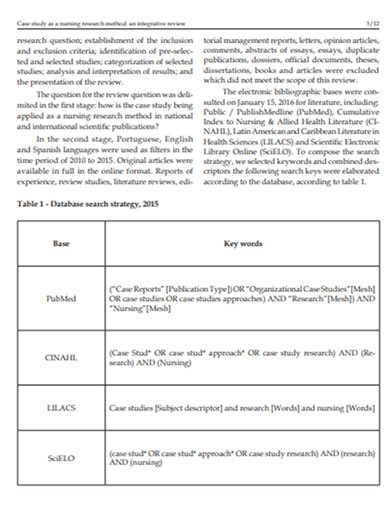
9. Standard Nursing Case Study Example
resourcecenter.ovid.com
10. Nursing Disability Case Study Example
careerswales.com
11. Nursing care Patients Case Study Example

12. School of Nursing Case Study Example

ebn.bmj.com
13. Evaluation of Nursing Care Case Study Example
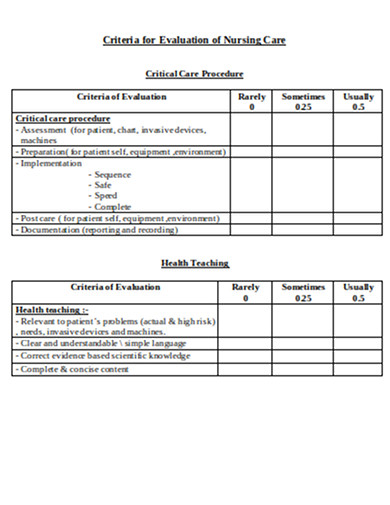
philadelphia.edu
Nursing Case Study Segments
Typically, a nursing case study contains three main categories, such as the items below.
1. The Status of a Patient
In this section, you will provide the patient’s information, such as medical history, and give the current patient’s diagnosis, condition, and treatment. Always remember to write down all the relevant information about the patient. Other items that you can collect in this stage are the reasons for the patient to seek medical care and the initial symptoms that he or she is experiencing. After that, based on the gathered information, you will explain the nature and cause of the illness of the patient.
2. The Nursing Assessment of the Patient
In this stage, you will need to prepare your evaluation of the patient’s condition. You should explain each observation that you have collected based on the vital signs and test results. You will also explain each nursing diagnosis that you have identified and determine the proper nursing care plan for the patient.
3. The Current Care Plan and Recommendations
Describe the appropriate care plan that you can recommend to the patient based on the diagnosis, current status, and prognosis in detail, including how the care plan will affect his or her life quality. If needed, you can also evaluate the patient’s existing care plan and give recommendations to enhance it. It is also crucial to cite relevant authoritative sources that will support your recommendations .
Objectives of Nursing Case Study
Nursing case studies are integral educational tools that bridge theoretical knowledge with practical application in patient care. They serve several key objectives essential for the development of nursing students and professionals. Here are the primary objectives of nursing case studies:
1. Enhance Critical Thinking and Clinical Reasoning
Case studies encourage nurses to analyze complex patient scenarios, make informed decisions, and apply critical thinking skills to solve problems. They simulate real-life situations, requiring nurses to evaluate data, consider multiple outcomes, and choose the best course of action.
2. Improve Diagnostic Skills
Through the detailed analysis of patient information, symptoms, and diagnostic results, nursing case studies help improve diagnostic skills. They allow nurses to practice interpreting clinical data to identify patient conditions and understand the underlying causes of symptoms.
3. Facilitate Application of Theoretical Knowledge
Nursing case studies provide a direct bridge between classroom learning and clinical practice. They offer a practical venue for applying theoretical knowledge about anatomy, physiology, pharmacology, and nursing theories to real-world patient care situations.
4. Promote Understanding of Comprehensive Patient Care
These studies emphasize the importance of holistic care, considering the physical, emotional, social, and psychological aspects of patient well-being. Nurses learn to develop comprehensive care plans that address all facets of a patient’s health.
5. Encourage Reflective Practice and Self-Assessment
Reflecting on case study outcomes enables nurses to evaluate their own decision-making processes, clinical judgments, and actions. This self-assessment promotes continuous learning and professional growth by identifying areas for improvement.
6. Foster Interdisciplinary Collaboration
Case studies often involve scenarios that require collaboration among healthcare professionals from various disciplines. They teach nurses the value of teamwork, communication, and the integration of different expertise to achieve optimal patient outcomes.
7. Enhance Patient Education and Advocacy Skills
By working through case studies, nurses improve their ability to educate patients and families about health conditions, treatment plans, and preventive measures. They also learn to advocate for their patients’ needs and preferences within the healthcare system.
8. Prepare for Real-Life Challenges
Nursing case studies prepare students and new nurses for the unpredictability and challenges of real-life clinical settings. They provide safe, controlled environments to practice responses to emergencies, ethical dilemmas, and complex patient needs without the risk of actual harm.
Steps in Nursing Process
Whether you are handling a patient with schizophrenia, pneumonia, diabetes, appendicitis, hypertension, COPD, etc, you will need to follow specific steps to ensure that you are executing the critical nursing process.
1. Assess the Patient
The first step of the nursing process requires critical thinking skills as it involves gathering both subjective and objective data. Subjective data includes verbal statements that you can collect from the patient or caregiver. In contrast, objective information refers to measurable and tangible data, such as vital signs, height, weight, etc. You can also use other sources of information, such as electronic health records, and friends that are in direct contact with the patient.
2. Diagnose the Patient
This critical step will help you in the next steps, such as planning and implementation of patient care. In this step, you will formulate a nursing diagnosis by applying clinical judgment. As a nurse, the North American Nursing Diagnosis Association (NANDA) will give you an up-to-date nursing diagnosis list, which will allow you to form a diagnosis based on the actual health problem.
3. Plan for a Proper Patient Care Plan
This part is where you will plan out the appropriate care plan for the patient. You will set this goal following the evidence-based practice (EDP) guidelines. The goal you will set should be specific, measurable, attainable, realistic, and timely ( SMART ).
4. Implement the Plan
In this stage, you can execute the plan that you have developed in the previous step. The implementation may need interventions such as a cardiac monitor, medication administration, etc.
5. Evaluate the Results
It is crucial to remember that every time the team does an intervention, you must do a reassessment to ensure that the process will lead to a positive result. You may need to reassess the patient depending on his progress, and the care plan may be modified based on the reassessment result.
Where to find nursing case studies?
Nursing case studies can be found in a variety of academic, professional, and medical resources. Here are some key places to look for nursing case studies:
- Academic Journals : Many academic journals focus on nursing and healthcare and publish case studies regularly. Examples include the “Journal of Clinical Nursing,” “Nursing Case Studies,” and “American Journal of Nursing.”
- University and College Libraries : Many academic institutions provide access to databases and journals that contain nursing case studies. Libraries often have subscriptions to these resources.
- Online Medical Libraries : Websites like PubMed, ScienceDirect, and Wiley Online Library offer a vast collection of nursing and medical case studies.
- Professional Nursing Organizations : Organizations such as the American Nurses Association (ANA) and the National League for Nursing (NLN) often provide resources, including case studies, for their members.
- Nursing Education Websites : Websites dedicated to nursing education, such as Lippincott NursingCenter and Nurse.com, often feature case studies for educational purposes.
- Government Health Websites : The Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) sometimes publish case studies related to public health nursing and disease outbreaks.
- Nursing Textbooks and eBooks : Many nursing textbooks and eBooks include case studies to illustrate key concepts and scenarios encountered in practice.
- Online Nursing Forums and Communities : Forums and online communities for nursing professionals may share or discuss case studies as part of their content.
- Conference Proceedings : Nursing and healthcare conferences often include presentations of case studies. Many of these are published in the conference proceedings, which may be accessible online.
Carrying out a nursing case study can be a delicate task since it puts the life of a person at stake. Thus, it requires a thorough investigation. With that said, it is essential to gain intensive knowledge about this type of study. Today, we have discussed an overview of how to conduct a nursing case study. However, if you think that you are having problems with your writing skills , we recommend you to consider looking for an essay writing service from the experts in the nursing department to ensure that the output follows the appropriate writing style and terminology.
Text prompt
- Instructive
- Professional
10 Examples of Public speaking
20 Examples of Gas lighting
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- Write for Us
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 21, Issue 1
- What is a case study?
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Roberta Heale 1 ,
- Alison Twycross 2
- 1 School of Nursing , Laurentian University , Sudbury , Ontario , Canada
- 2 School of Health and Social Care , London South Bank University , London , UK
- Correspondence to Dr Roberta Heale, School of Nursing, Laurentian University, Sudbury, ON P3E2C6, Canada; rheale{at}laurentian.ca
https://doi.org/10.1136/eb-2017-102845
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
What is it?
Case study is a research methodology, typically seen in social and life sciences. There is no one definition of case study research. 1 However, very simply… ‘a case study can be defined as an intensive study about a person, a group of people or a unit, which is aimed to generalize over several units’. 1 A case study has also been described as an intensive, systematic investigation of a single individual, group, community or some other unit in which the researcher examines in-depth data relating to several variables. 2
Often there are several similar cases to consider such as educational or social service programmes that are delivered from a number of locations. Although similar, they are complex and have unique features. In these circumstances, the evaluation of several, similar cases will provide a better answer to a research question than if only one case is examined, hence the multiple-case study. Stake asserts that the cases are grouped and viewed as one entity, called the quintain . 6 ‘We study what is similar and different about the cases to understand the quintain better’. 6
The steps when using case study methodology are the same as for other types of research. 6 The first step is defining the single case or identifying a group of similar cases that can then be incorporated into a multiple-case study. A search to determine what is known about the case(s) is typically conducted. This may include a review of the literature, grey literature, media, reports and more, which serves to establish a basic understanding of the cases and informs the development of research questions. Data in case studies are often, but not exclusively, qualitative in nature. In multiple-case studies, analysis within cases and across cases is conducted. Themes arise from the analyses and assertions about the cases as a whole, or the quintain, emerge. 6
Benefits and limitations of case studies
If a researcher wants to study a specific phenomenon arising from a particular entity, then a single-case study is warranted and will allow for a in-depth understanding of the single phenomenon and, as discussed above, would involve collecting several different types of data. This is illustrated in example 1 below.
Using a multiple-case research study allows for a more in-depth understanding of the cases as a unit, through comparison of similarities and differences of the individual cases embedded within the quintain. Evidence arising from multiple-case studies is often stronger and more reliable than from single-case research. Multiple-case studies allow for more comprehensive exploration of research questions and theory development. 6
Despite the advantages of case studies, there are limitations. The sheer volume of data is difficult to organise and data analysis and integration strategies need to be carefully thought through. There is also sometimes a temptation to veer away from the research focus. 2 Reporting of findings from multiple-case research studies is also challenging at times, 1 particularly in relation to the word limits for some journal papers.
Examples of case studies
Example 1: nurses’ paediatric pain management practices.
One of the authors of this paper (AT) has used a case study approach to explore nurses’ paediatric pain management practices. This involved collecting several datasets:
Observational data to gain a picture about actual pain management practices.
Questionnaire data about nurses’ knowledge about paediatric pain management practices and how well they felt they managed pain in children.
Questionnaire data about how critical nurses perceived pain management tasks to be.
These datasets were analysed separately and then compared 7–9 and demonstrated that nurses’ level of theoretical did not impact on the quality of their pain management practices. 7 Nor did individual nurse’s perceptions of how critical a task was effect the likelihood of them carrying out this task in practice. 8 There was also a difference in self-reported and observed practices 9 ; actual (observed) practices did not confirm to best practice guidelines, whereas self-reported practices tended to.
Example 2: quality of care for complex patients at Nurse Practitioner-Led Clinics (NPLCs)
The other author of this paper (RH) has conducted a multiple-case study to determine the quality of care for patients with complex clinical presentations in NPLCs in Ontario, Canada. 10 Five NPLCs served as individual cases that, together, represented the quatrain. Three types of data were collected including:
Review of documentation related to the NPLC model (media, annual reports, research articles, grey literature and regulatory legislation).
Interviews with nurse practitioners (NPs) practising at the five NPLCs to determine their perceptions of the impact of the NPLC model on the quality of care provided to patients with multimorbidity.
Chart audits conducted at the five NPLCs to determine the extent to which evidence-based guidelines were followed for patients with diabetes and at least one other chronic condition.
The three sources of data collected from the five NPLCs were analysed and themes arose related to the quality of care for complex patients at NPLCs. The multiple-case study confirmed that nurse practitioners are the primary care providers at the NPLCs, and this positively impacts the quality of care for patients with multimorbidity. Healthcare policy, such as lack of an increase in salary for NPs for 10 years, has resulted in issues in recruitment and retention of NPs at NPLCs. This, along with insufficient resources in the communities where NPLCs are located and high patient vulnerability at NPLCs, have a negative impact on the quality of care. 10
These examples illustrate how collecting data about a single case or multiple cases helps us to better understand the phenomenon in question. Case study methodology serves to provide a framework for evaluation and analysis of complex issues. It shines a light on the holistic nature of nursing practice and offers a perspective that informs improved patient care.
- Gustafsson J
- Calanzaro M
- Sandelowski M
Competing interests None declared.
Provenance and peer review Commissioned; internally peer reviewed.
Read the full text or download the PDF:
This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Akhtar N, Lee L Utilization and complications of central venous access devices in oncology patients. Current Oncology.. 2021; 28:(1)367-377 https://doi.org/10.3390/curroncol28010039
BD ChloraPrep: summary of product characteristics.. 2021; https://www.bd.com/en-uk/products/infection-prevention/chloraprep-patient-preoperative-skin-preparation/chloraprep-smpc-pil-msds
Chloraprep 10.5ml applicator.. 2022a; https://www.bd.com/en-uk/products/infection-prevention/chloraprep-patient-preoperative-skin-preparation/chloraprep-patient-preoperative-skin-preparation-product-line/chloraprep-105-ml-applicator
Chloraprep 3ml applicator.. 2022b; https://www.bd.com/en-uk/products/infection-prevention/chloraprep-patient-preoperative-skin-preparation/chloraprep-patient-preoperative-skin-preparation-product-line/chloraprep-3-ml-applicator
Website.. 2021; https://www.cdc.gov/cancer/preventinfections/providers.htm
Ceylan G, Topal S, Turgut N, Ozdamar N, Oruc Y, Agin H, Devrim I Assessment of potential differences between pre-filled and manually prepared syringe use during vascular access device management in a pediatric intensive care unit. https://doi.org/10.1177/11297298211015500
Clare S, Rowley S Best practice skin antisepsis for insertion of peripheral catheters. Br J Nurs.. 2021; 30:(1)8-14 https://doi.org/10.12968/bjon.2021.30.1.8
Caguioa J, Pilpil F, Greensitt C, Carnan D HANDS: standardised intravascular practice based on evidence. Br J Nurs.. 2012; 21:(14)S4-S11 https://doi.org/10.12968/bjon.2012.21.Sup14.S4
Easterlow D, Hoddinott P, Harrison S Implementing and standardising the use of peripheral vascular access devices. J Clin Nurs.. 2010; 19:(5-6)721-727 https://doi.org/10.1111/j.1365-2702.2009.03098.x
Florman S, Nichols RL Current approaches for the prevention of surgical site infections. Am J Infect Dis.. 2007; 3:(1)51-61 https://doi.org/10.3844/ajidsp.2007.51.61
Gorski LA, Hadaway L, Hagle M Infusion therapy standards of practice. J Infus Nurs.. 2021; 44:(S1)S1-S224 https://doi.org/10.1097/NAN.0000000000000396
Guenezan J, Marjanovic N, Drugeon B Chlorhexidine plus alcohol versus povidone iodine plus alcohol, combined or not with innovative devices, for prevention of short-term peripheral venous catheter infection and failure (CLEAN 3 study): an investigator-initiated, openlabel, single centre, randomised-controlled, two-by-two factorial trial [published correction appears in Lancet Infect Dis. 2021 Apr 6]. Lancet Infect Dis.. 2021; 21:(7)1038-1048 https://doi.org/10.1016/S1473-3099(20)30738-6
Gunka V, Soltani P, Astrakianakis G, Martinez M, Albert A, Taylor J, Kavanagh T Determination of ChloraPrep® drying time before neuraxial anesthesia in elective cesarean delivery: a prospective observational study. Int J Obstet Anesth.. 2019; 38:19-24 https://doi.org/10.1016/j.ijoa.2018.10.012
Ishikawa K, Furukawa K Staphylococcus aureus bacteraemia due to central venous catheter infection: a clinical comparison of infections caused by methicillin-resistant and methicillin-susceptible strains. Cureus.. 2021; 13:(7) https://doi.org/10.7759/cureus.16607
Loveday HP, Wilson JA, Pratt RJ Epic3: national evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. J Hosp Infect.. 2014; 86:(S1)S1-70 https://doi.org/10.1016/S0195-6701(13)60012-2
Promoting safer use of injectable medicines.. 2007; https://healthcareea.vctms.co.uk/assets/content/9652/4759/content/injectable.pdf
Standards for infusion therapy. 4th edn.. 2016; https://www.rcn.org.uk/clinical-topics/Infection-prevention-and-control/Standards-for-infusion-therapy
Taxbro K, Chopra V Appropriate vascular access for patients with cancer. Lancet.. 2021; 398:(10298)367-368 https://doi.org/10.1016/S0140-6736(21)00920-X
Case Studies
Gema munoz-mozas.
Vascular Access Advanced Nurse Practitioner—Lead Vascular Access Nurse, The Royal Marsden NHS Foundation Trust
View articles · Email Gema
Colin Fairhurst
Vascular Access Advanced Clinical Practitioner, University Hospitals Plymouth NHS Trust
View articles
Simon Clare
Research and Practice Development Director, The Association for Safe Aseptic Practice
View articles · Email Simon
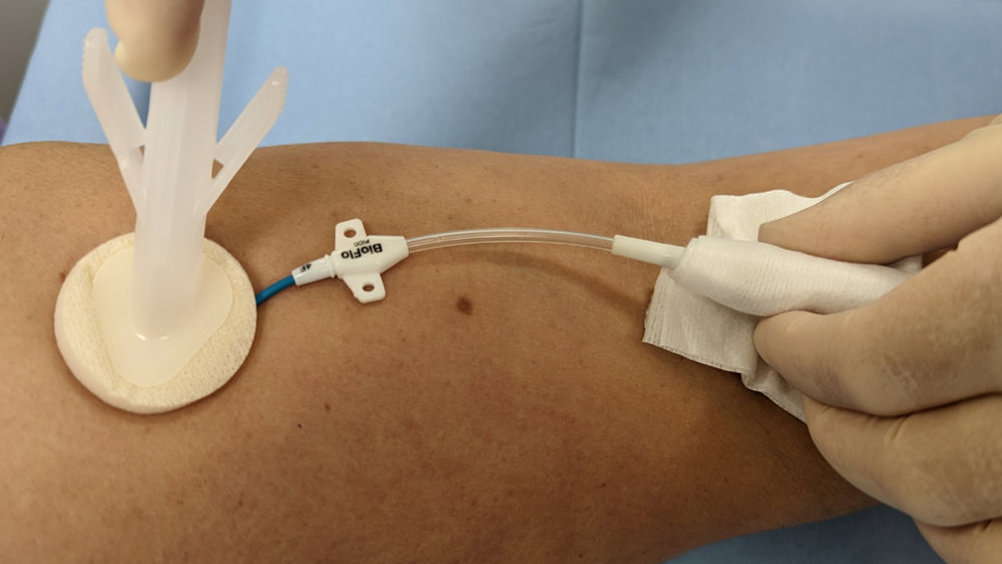
Intravenous (IV) access, both peripheral and central, is an integral part of the patient care pathways for diagnosing and treating cancer. Patients receiving systemic anticancer treatment (SACT) are at risk for developing infections, which may lead to hospitalisation, disruptions in treatment schedules and even death ( Centers for Disease Control and Prevention, 2021 ). However, infection rates can be reduced and general patient outcomes improved with the evidence-based standardisation of IV practice, and the adoption of the appropriate equipment, such as peripheral IV cannulas, flushing solutions and sterile IV dressings ( Easterlow et al, 2010 ).
Cancer treatment frequently involves the use of central venous catheters (CVCs)-also referred to as central venous access devices (CVADs)—which can represent a lifeline for patients when used to administer all kinds of IV medications, including chemotherapy, blood products and parenteral nutrition. They can also be used to obtain blood samples, which can improve the patient’s quality of life by reducing the need for peripheral stabs from regular venepunctures ( Taxbro and Chopra, 2021 ). CVCs are relatively easy to insert and care for; however, they are associated with potential complications throughout their insertion and maintenance.
One serious complication of CVC use is catheter-related bloodstream infections (CRBSIs), which can increase morbidity, leading to prolonged hospitalisation and critical use of hospital resources ( Akhtar and Lee, 2021 ). Early-onset CRBSIs are commonly caused by skin pathogens, and so a cornerstone of a CRBSI prevention is skin antisepsis at the time of CVC insertion. Appropriate antisepsis (decontamination/preparation) of the site for CVC insertion can prevent the transmission of such skin pathogens during insertion, while reducing the burden of bacteria on the CVC exit site ( Loveday et al, 2014 ).
Evidence-based practice for the prevention of a CRBSIs and other healthcare-associated infections recommends skin antisepsis prior to insertion of a vascular-access device (VAD) using a 2% chlorhexidine gluconate and 70% isopropyl alcohol solution. This is recommended in guidelines such as epic3 ( Loveday et al, 2014 ), the Standards for Infusion Therapy ( Royal College of Nursing, 2016 ) and the Infusion Therapy Standards of Practice ( Gorski et al, 2021 ). A strong evidenced-backed product such as BD ChloraPrep™ ( Figure 1 ) has a combination of 2% chlorhexidine gluconate in 70% isopropyl alcohol that provides broad-spectrum rapid-action antisepsis, while the applicators facilitate a sterile, single-use application that eliminates direct hand-to-patient contact, helping to reduce cross-contamination and maintaining sterile conditions ( BD, 2021 ). The BD ChloraPrep™ applicator’s circular head allows precise antisepsis of the required area, and the sponge head helps to apply gentle friction in back-and-forth motion to penetrate the skin layers ( BD, 2021 ). BD ChloraPrep’s rapidacting, persistent and broad-spectrum characteristics and proven applicator system ( Florman and Nichols, 2007 ) make it a vital part of the policy and protocol for insertion, care and maintenance of CVCs in specialist cancer centres such as the Royal Marsden. Meanwhile, the use of BD PosiFlush™ Prefilled Saline Syringe ( Figure 2 ), a prefilled normal saline (0.9% sodium choride) syringe, is established practice for the flushing regime of VADs in many NHS Trusts.
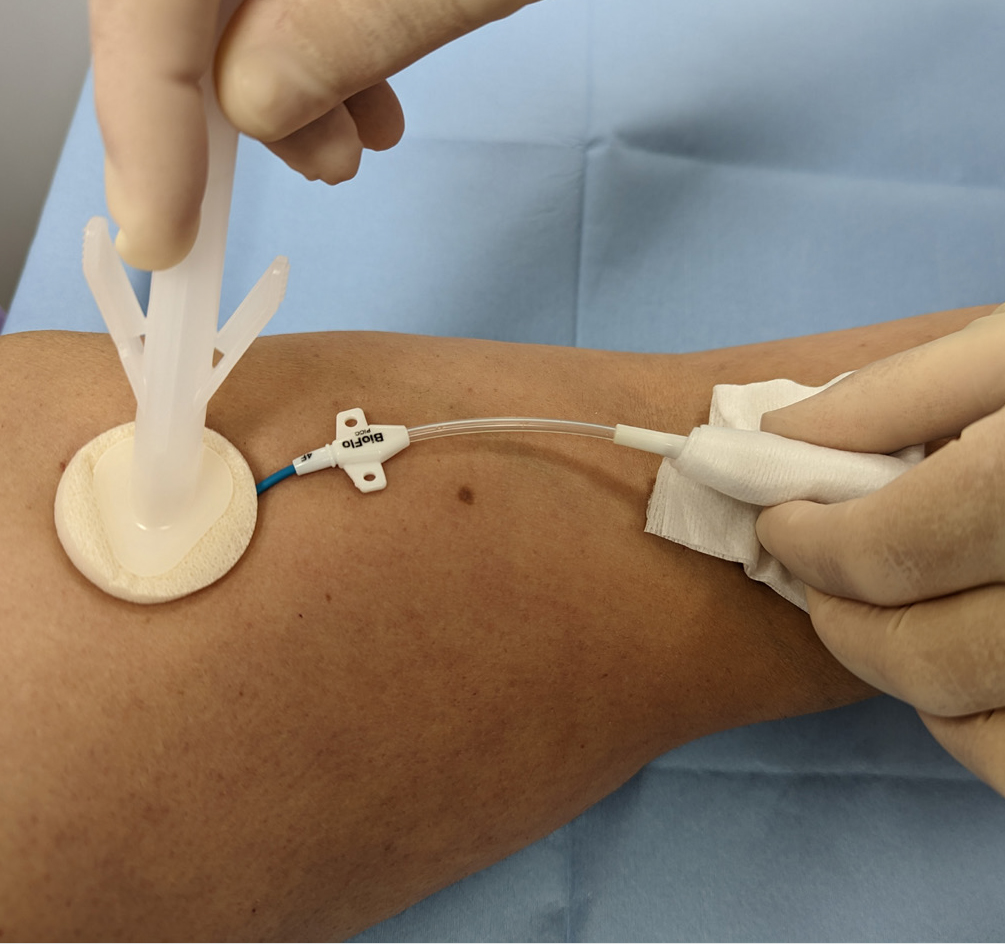
The following five case studies present examples from personal experience of clinical practice that illustrate how and why clinicians in oncology and other disciplines use BD ChloraPrep ™ and BD PosiFlush ™ Prefilled Saline Syringe in both adult and paediatric patients.
Case study 1 (Andy)
Andy was a 65-year-old man being treated for metastatic colorectal cancer at the Royal Marsden NHS Foundation Trust specialist cancer service, which provides state-of-the-art treatment to over 60 000 patients each year.
Andy had a peripherally inserted central catheter (PICC) placed at the onset of his chemotherapy treatment to facilitate IV treatment. While in situ, PICCs require regular maintenance to minimise associated risks. This consists of a weekly dressing change to minimise infection and a weekly flush to maintain patency, if not in constant use. For ambulatory patients, weekly PICC maintenance can be carried out either in the hospital outpatient department or at home by a district nurse or family member trained to do so. Patients, relatives, carers and less-experienced nurses involved in PICC care (flushing and dressing) can watch a video on the Royal Marsden website as an aide memoir.
Initially, Andy decided to have his weekly PICC maintenance at the hospital’s nurse-led clinic for the maintenance of CVCs. At the clinic, Andy’s PICC dressing change and catheter flushing procedures were performed by a nursing associate (NA), who, having completed the relevant competences and undergone supervised practise, could carry out weekly catheter maintenance and access PICC for blood sampling.
In line with hospital policy, the PICC dressing change was performed under aseptic non-touch technique (ANTT) using a dressing pack and sterile gloves. After removal of the old dressing, the skin around the entry site and the PICC was cleaned with a 3 ml BD ChloraPrep™ applicator, using back-andforth strokes for 30 seconds and allowing the area to air dry completely before applying the new dressing. As clarified in a recent article on skin antisepsis (Clare and Rowley, 2020), BD ChloraPrep™ applicator facilitated a sterile, single-use application that eliminates direct hand-to-patient contact, which help reduce cross-contamination and maintaining ANTT. Its circular head allowed precise antisepsis around the catheter, and the sponge head helped to apply gentle friction in back-and-forth strokes to penetrate the skin layers.
Once the new dressing was applied, the NA continued to clean the catheter hub and change the needle-free connector. Finally, the catheter lumen was flushed with 10 ml of normal saline (0.9% sodium chloride) with a pre-filled saline syringe (BD PosiFlush™ Prefilled Saline Syringe). This involved flushing 1 ml at a time, following a push-pause technique, with positive pressure disconnection to ensure catheter patency. The classification of these syringes as medical devices enables NAs and other nonregistered members of the clinical team to support nursing staff with the care and maintenance of PICCs and other CVCs, within local policies and procedures. Using pre-filled syringes can save time and minimise the risk of contamination of the solution ( Ceylan et al, 2021 ).
The use of pre-filled 0.9% sodium chloride syringes facilitates home maintenance of PICCs for patients. When Andy did not need to attend hospital, his PICC maintenance could be performed by a family member. Patients and relatives could access the necessary equipment and training from the day-case unit or outpatient department. Home PICC maintenance is extremely beneficial, not just to providers, but also to patients, who may avoid unnecessary hospital attendance and so benefit from more quality time at home and a reduced risk of hospital-acquired infections. Many patients and relatives have commented on the convenience of having their PICC maintenance at home and how easy they found using the ChloraPrep™ and BD PosiFlush™ Prefilled Saline Syringe ‘sticks’.
Case study 2 (Gail)
Gail was as a 48-year-old woman being treated for bladder cancer with folinic acid, fluorouracil and oxaliplatin (FOLOX). She was admitted for a replacement PICC, primarily for continuous cytotoxic intravenous medication via infusion pump in the homecare setting. Her first PICC developed a reaction thought to be related to a sutureless securement device (SSD) anchoring the PICC. The device was removed, but this resulted in displacement of the PICC and incorrect positioning in the vessel (superior vena cava). Now unsafe, the PICC was removed, awaiting replacement, which resulted in a delayed start for the chemotherapy.
A second PICC placement was attempted by a nurse-led CVC placement team, and a line attempt was made in Gail’s left arm. Skin antisepsis was undertaken using a 2% chlorhexidine gluconate and 70% isopropyl alcohol solution (ChloraPrep™). A BD ChloraPrep ™ 10 ml applicator was selected, using manufacturer’s recommendations, as per best practice guidance for CVC placement ( Loveday et al, 2014 ) and to comply with local policy for the use of ANTT. The BD ChloraPrep™ applicator allowed improved non-touch technique and helped facilitate good key-part and key-site protection, in line with ANTT ( Clare and Rowley, 2021 ).
The inserting clinician failed to successfully position the PICC in Gail’s left arm and moved to try on the right. On the second attempt, Gail noted the use of BD ChloraPrep™ and stated that she was allergic to the product, reporting a severe skin rash and local discomfort. The line placer informed the Gail that she had used BD ChloraPrep™ on the failed first attempt without issue, and she gave her consent to continue the procedure. No skin reaction was noted during or after insertion of the PICC.
BD ChloraPrep™ has a rapid-acting broad-spectrum antiseptic range and ability to keep fighting bacteria for at least 48 hours ( BD, 2021 ). These were tangible benefits during maintenance of the CVC insertion site, in the protection of key sites following dressing change and until subsequent dressing changes. There are reported observations of clinicians not allowing the skin to fully dry and applying a new dressing onto wet skin after removing old dressings and disinfecting the exit site with BD ChloraPrep™. This has been reported to cause skin irritation, which can be mistaken for an allergic reaction and lead the patient to think that they have an allergy to chlorhexidine. In our centre’s general experience, very few true allergic reactions have ever been reported by the insertion team. Improved surveillance might better differentiate between later reported reactions, possibly associated with a delayed response to exposure to BD ChloraPrep ™ at insertion, and local skin irritation caused by incorrect management at some later point during hospitalisation.
Staff training is an important consideration in the safe and correct use of BD ChloraPrep™ products and the correct use of adhesive dressings to avoid irritant contact dermatitis (ICD). It is worth noting that it can be difficult to differentiate between ICD and allergic contact dermatitis (ACD). Education and training should be multifaceted (such as with training videos and study days), allowing for different ways of learning, and monitored with audit. Local training in the benefits of using BD ChloraPrep™ correctly have been reinforced by adding simple instructions to ANTT procedure guidelines for CVC insertion and maintenance. Education on its own is often limited to a single episode of training, the benefit of using ANTT procedure guidelines is that they are embedded in a programme of audits and periodic competency reassessment. This makes sure that, as an integral part of good practice, skin antisepsis with BD ChloraPrep ™ is consistently and accurately retrained and assessed.
Gail’s case illustrates the importance of correct application of BD ChloraPrep ™ and how good documentation and surveillance are vital in monitoring skin health during the repeated use skindisinfection products. Care should be taken when recording ICD and ACD reactions, and staff should take steps to confirm true allergy versus temporary skin irritation.
Case study 3 (Beata)
Beata was a 13-year-old teenage girl being treated for acute myeloid leukaemia. Although Beata had a dual-lumen skin-tunnelled catheter in situ, a peripheral intravenous cannula (PIVC) was required for the administration of contrast media for computed tomography (CT) scanning. However, Beata had needlephobia, and so the lead vascular access nurse was contacted to insert the cannula, following ultrasound guidance and the ANTT. After Beata and her mother gave their consent to the procedure, the nurse gathered and prepared all the equipment, including a cannulation pack, single-use tourniquet, skin-antisepsis product, appropriate cannula, PIVC dressing, 0.9% sodium chloride BD PosiFlush ™ Prefilled Saline Syringe, sterile gel, sterile dressing to cover ultrasound probe and personal protective equipment.
Prior to PIVC insertion, a 4x5 cm area of skin underwent antisepsis with a 1.5 ml BD ChloraPrep ™ Frepp applicator, with back-and-forth strokes for 30 seconds, and was allowed to air-dry. The vascular access team prefer to use BD ChloraPrep ™ Frepp over single-use wipes, as the former is faster acting and provides the right volume to decontaminate the indicated area using ANTT ( Clare and Rowley, 2021 ).
Following insertion, the PIVC was flushed with a 10 ml BD PosiFlush ™ Prefilled Saline Syringe syringe, using a pushpause pulsatile technique, with positive pressure disconnection. Local policy recommends the use of pre-filled saline syringes, as they save time and minimise infection risk compared with manually drawn saline flushes ( Ceylan et al, 2021 ). The Trust also permits competent non-registered members of staff to perform PIVC insertion, which is more cost-effective than depending on registered nurses.
In Beata’s case, the team considered the use of BD ChloraPrep™ and BD PosiFlush™ Prefilled Saline Syringe to be essential for the prevention of VAD-associated infections, as well as increasing the quality of nursing care by saving time in the day-case and inpatient settings alike.
Case study 4 (Emma)
Emma, a 43-year-old woman diagnosed with acute lymphoblastic leukaemia, was scheduled for an allogenic stem-cell transplant and associated chemotherapy. To facilitate this, she attended the vascular access service at University Hospitals Plymouth NHS Trust for the insertion of a triple-lumen skin-tunnelled catheter. This was identified as the best VAD for her needs, because of its longevity, multiple points of access and decreased infection risk compared with other devices, such as PICCs.
This was Emma’s second advanced VAD insertion, having previously received an apheresis line due to poor peripheral venous access, to facilitate the prior stem-cell harvest. She was yet to receive any treatment, and, therefore, no immunodeficiency had been identified prior to the insertion procedure.
Trust policy for skin disinfection prior to the insertion or removal of PICC lines is a 2% chlorhexidine gluconate and 70% isopropyl alcohol solution, BD ChloraPrep™. There is an exception for patient history of allergy or sensitivity to BD ChloraPrep™, where 10% povidone iodine is used instead. Emma had received BD ChloraPrep™ before, with no sign allergy or sensitivity, and so the vascular access team decided to use this product again for insertion. BD Chloraprep™ was used, in preference of other skin antisepsis options, due to the applicator’s ability to effectively penetrate the layers of the epidermis, as well as the ability to eliminate direct hand-to-skin contact between the operator and patient ( Clare and Rowley, 2021 ).
Insertion of a skin-tunnelled catheter first requires disinfection of a large area, including the neck and upper chest. Following the manufacturer’s coverage recommendations, a 10.5 ml BD ChloraPrep™ applicator was selected as most suitable to cover an area of 25x30 cm ( BD, 2022 a).
The applicator was activated by pinching the wings to allow the antiseptic solution to properly load onto the sponge. To ensure proper release of the solution, the applicator was held on the skin against the anticipated site of insertion until the sponge pad became saturated. Then, a back-and-forth rubbing motion was undertaken for a minimum of 30 seconds, ensuring that the full area to be used was covered. The solution was then left to dry completely, prior to full-body draping, leaving the procedural area exposed for the procedure. Generally, drying time takes from 30 to 60 seconds, but local policy is not restrictive, as allowing the solution to fully dry is of paramount importance ( Gunka et al, 2019 ). BD Chloraprep™ is effective against a wide variety of microorganisms and has a rapid onset of action ( Florman and Nichols, 2007 ). Therefore, it was felt to be the best option for procedural and ongoing care skin asepsis in a patient anticipated to be immunocompromised during treatment.
It is the normal policy of the Trust’s vascular access service to flush VADs using BD PosiFlush™ Prefilled Saline Syringes with 0.9% sodium chloride. Likewise, BD PosiFlush™ Prefilled Saline Syringes Sterile Pathway (SP) are used to prime all VADs prior to insertion and to check for correct patency once inserted. BD PosiFlush ™ Prefilled Saline Syringe were used in preference of other options, such as vials or bags, due to the absence of requirement for a prescription in the local organisation. They are treated as a medical device and, therefore, can be used without prescription. The advantage of this is that flushes can be administered in a nurse-led clinic, where prescribers are not always available. Aside from the logistical advantages, the use of pre-filled syringes reduces the risk of microbial contamination through preparation error and administration error through correct labelling ( National Patient Safety Agency, 2007 ) In Emma’s case, three BD PosiFlush™ SP Prefilled Saline Syringes were used to check patency and/or ascertain venous location following the insertion of the skin-tunnelled catheter.
In this case, both BD ChloraPrep ™ and BD PosiFlush ™ Prefilled Saline Syringe proved simple to use and helped achieve a successful procedural outcome for the patient.
Case study 5 (Frank)
Frank was a 47-year-old man who had been diagnosed with infective endocarditis following a trans-oesophageal echo. A few days later, to facilitate his planned treatment of 6 weeks of intravenous antibiotics to be administered 4-hourly every day, he was referred to the vascular access service for insertion of longterm IV access. To facilitate this administration, the decision was made to place a PICC.
Frank’s referral included a history of illegal intravenous drug use and details of the consequent difficulty the ward-based team had in finding suitable veins to obtain vascular access. His medical history also included infected abscesses in the left groin and methicillin-resistant Staphylococcus aureus (MRSA) colonisation.
First, Frank was administered suppression therapy for MRSA decolonisation. Following this and prior to PICC insertion, the skin antisepsis procedure was undertaken using a 2% chlorhexidine gluconate and 70% isopropyl alcohol solution, BD ChloraPrep™, in adherence to Trust policy ( Loveday et al, 2014 ). Specifically, BD ChloraPrep™ applicators are selected for their single-use application. They have been demonstrated to reduce the risk of infectious complications (catheter colonisation and local infection) by 92% compared with 5% povidone iodine (PVI) 69% ethanol ( Guenezan et al, 2021 ). A 3 ml BD ChloraPrep™ applicator was considered suitable to decontaminate an area sufficient for the intended PICC insertion procedure, as recommended by the manufacturer ( BD, 2022 b). It was applied using a back-and-forth motion for a minimum of 30 seconds and left to fully dry ( Loveday et al, 2014 ). Staphylococcus aureus bacteraemia’s have a mortality rate of 20-40% and are predominantly caused by VAD insertion ( Ishikawa and Furukawa, 2021 ), and, therefore, the need to reduce this risk was of particular importance for this patient due to the history of MRSA colonisation.
In Frank’s case, the use of BD ChloraPrep™ during the insertion procedure and for each subsequent dressing change episode participated in an uneventful period of treatment. The clinical challenges posed by the patients’ presentation of MRSA colonisation meant the risk of infection was increased but, through correct antisepsis, no adverse events were noted, and the full course of treatment was successfully administered through the PICC.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Integr Care
- v.22(1); Jan-Mar 2022

The Evolving Roles of Nurses Providing Care at Home: A Qualitative Case Study Research of a Transitional Care Team
Wei ting chen.
1 Advanced Practice Nurse, Division for Central Health, Tan Tock Seng Hospital, SG
2 Alice Lee Centre for Nursing Studies, Yong Loo Lin School of Medicine, National University of Singapore, Singapore
3 National University Health System, SG
Yeow Leng Chow
To examine the roles of transitional care nurses in an integrated healthcare system and how the integrated healthcare system influences their evolving roles.
Background:
Transitional care teams have been introduced to enable the seamless transfer of patients from acute-care to the home settings. A qualitative case study of the transitional care team was conducted to understand the changing roles of these nurses in an integrated Regional Health System (RHS) in Singapore.
A hospital transitional team of an integrated RHS was studied. Purposive sampling was used. Non-participant observations and follow-up interviews were conducted with four nurses. Data were triangulated with the interviews of two managers and three healthcare professionals, and the analysis of documents. Within-case thematic analysis was carried out.
Three themes were identified: ‘Coming together to meet the needs of all’; ‘Standing strong amidst the stormy waves’; and ‘Searching for the right formula in handling complexity’. These themes have explained on the atypical roles taken on by nurses in their attempts to close the gaps and meet the patients’ needs. Various factors influencing the evolving roles were revealed.
Conclusion:
The roles of nurses have ‘emerged differently’ from their traditional counterparts. Various nursing roles have been undertaken to facilitate care integration. The findings emphasised the important balance between formal structural practices and informal processes in facilitating and supporting the nurses in their role development.
Introduction
Health systems are facing challenges as the ageing population increases. From 2014 to 2017, the proportion of the Singaporean population aged 65 and above rose from 11.2% to 13.0% [ 1 , 2 ]. It has been projected that about 18.7% of its population would be aged 65 and above in 2030 [ 3 ]. The elderly were found to have more chronic conditions, with 80.6% of the age-group more than 65 years reporting one or more chronic diseases compared to 54.8% for that between 45 and 64 years [ 4 ]. With the increased health and social care needs of the elderly in Singapore, the healthcare system and policies have been evolving to embrace the principles of integrated care [ 5 ]. Singapore’s reforms started in 2000 when the government reorganised all polyclinics and restructured hospitals under two healthcare clusters–the National Healthcare Group (NHG) and Singapore Health Services (SingHealth)–to provide integrated care for patients [ 6 ]. From 2008 to 2009, six integrated regional health systems (RHSs) have been formed ( Figure 1 ). Each RHS aimed to promote the integration of care services received by patients in public hospitals, primary care providers or intermediate and long-term care providers within a designated geographical area [ 6 , 7 ]. Further restructuring of the RHSs occurred in 2017, where three large RHSs were formed ( Figure 1 ). While such re-clustering efforts aimed to promote greater integration of care, evidence on its benefits is still lacking [ 5 ].

Re-clustering of six integrated regional health systems (RHSs) to three larger integrated RHSs in 2017 [ 8 , 9 ].
With the need to provide holistic and coordinated care, nursing teams have evolved from a traditional flattened structure of nurses to multi-skilled and multi-professional teams [ 10 ]. The elderly often require coordination of care among multiple healthcare and social-care providers [ 11 ] and transitional care from the hospital to home [ 12 ]. This has also accentuated the role of nurses in care coordination and management [ 13 , 14 ]. Similar nursing developments have taken place in Singapore ( Figure 2 ). The introduction of Hospital-to-Home (H2H) programme has driven the development of transitional care or RHS community nurses. These registered nurses (RN) were based in acute care hospitals and promote the safe and timely transfer of patients between care settings by taking on activities at hospital discharge and post-discharge care. This decreases preventable adverse events during care transition, such as medication errors and falls [ 12 ].

Development of Singapore’s healthcare system and home and community nursing [ 15 ].
A literature review has been conducted to understand the changing roles of transitional care and community nurses in integrated healthcare systems. Common activities and practices performed by home and community nurses have been identified in previous studies [ 16 , 17 , 18 ]. They are direct patient care, patients’ monitoring, educational actions, psychosocial care and administrative work. There is also a shift away from the reactive nursing delivery system to models of care that focus on preventive home visits for older people, nurse-led post-discharge services and the specialisation of nursing work [ 19 , 20 , 21 ].
Transitional care programmes have been studied to identify the main interventions involved, duration of care and their effectiveness. In a recent scoping review, key professionals involved in transitional care teams were often nurses, with some of them receiving additional training in transitional care or speciality training [ 22 ]. Common interventions were discharge planning, medication management, structured needs assessment, patient education, chronic disease self-management, post-discharge guidance, caregiver support, care coordination and case management [ 12 , 23 , 24 , 25 , 26 , 27 ]. Delivery of transitional care varied in duration and frequencies of telephonic and/or home visitation mode [ 22 , 28 ].
Despite the programmes have demonstrated their usefulness and cost-effectiveness [ 23 , 29 ], the changing roles assumed by nurses were little explored. The programmes often focused on specific disease conditions or patient profiles [ 29 , 30 ] such that roles of the nurses could be seen as an extension of work settings from hospital to community. A recent study has demonstrated the interrelated influence of moderating factors on the implementation fidelity of the transitional care program [ 25 ]. Gaps in the literature could be seen in the overall change in the roles of nurses in the hospital-to-home interface and as an overall integrated system approach. Such understanding will be crucial in determining whether certain roles were assumed considering the changing contextual system factors and developments of other professional roles in this care system.
As integrated healthcare systems are increasingly formed, studies have shown their impact on the roles of nurses [ 31 , 32 , 33 , 34 ]. Coordination and partnership across settings and delegation and supervision of unlicensed personnel were reported [ 33 ]. There were also a high number of non-patient-related activities such as meetings, referrals and administrative tasks [ 31 ]. Although all of these studies have afforded some evidence on the influences of the integrated care system on the evolution of the nursing roles, the actual changes and development of these roles have not been well elucidated. A study to understand the changing roles of nurses is warranted. In particular, the drivers for the development of community and home nursing have remained less explored. This study aimed to examine the roles of transitional care nurses in an integrated RHS and the influence of the development of RHS on their evolving roles. The research questions were the following:
- What are the transitional care nursing roles in an integrated RHS?
- What are the various influencing factors in the integrated RHS on their roles?
- How does the development of the integrated RHS affect the change in the roles of transitional care nurses?
Study design
A qualitative case study research design was used to examine the influence of different contexts and social interactions on the nursing roles, offering insights into the complex interrelationships between the components [ 35 , 36 ].
Theoretical framework
The role theory and complex adaptive system (CAS) theory were used to guide the study [ 37 , 38 ]. A role can be defined as ‘the set of prescriptions defining what the behaviour of a position member should be’ [ 39 ] (p29). Three aspects of role can be defined, with reference to the person segment (role of a nurse), behaviour segment (nursing roles) and person–behaviour segment (patterns of behaviour characteristics of transitional care nurses). This role theory emphasised the importance of observation as the optimal method to gather the behaviours of the transitional care nurses. The construct of the observation charts and interview schedules have aimed to uncover the various roles taken on by these nurses. Previous researchers have also emphasised the dynamic properties of roles and various influences on the roles of nurses within a social system [ 37 , 40 , 41 ]. Drawing reference from two existing CAS conceptual frameworks in healthcare [ 42 , 43 ] and findings from a separate study in the first author’s thesis [ 15 ], the conceptual framework for this study is proposed. This framework ( Figure 3 ) was based on the understanding that although nursing services are governed by systems of working within individual organisations, relationships were maintained between the organisations in the overarching integrated healthcare system. Besides emphasising the use of a qualitative case study research using multiple cases, this CAS framework guided the data analyses such that the within-case analysis preceded cross-case comparisons. The findings of the other three cases and the final analysis were reported separately in the first author’s thesis [ 15 ].

A refined conceptual framework that recognises the importance of relationships and interactions between different staff within each organisation and between different organisations [ 42 , 43 ].
Setting and sample
There were six integrated RHSs in Singapore before the mergers into three larger RHSs in January 2017. Despite the mergers, the operations in the six sub-systems have not changed drastically compared with their pre-merger times during data collection from April to September 2017. The sub-system of one of the three large RHSs in central Singapore was selected as the main research setting, hereafter referred to as ‘central RHS’. An instrumental case study was used to achieve the research objectives [ 35 ]. The transitional care team from the central RHS was the case of interest, named herein as ‘Case D’. This team formed a diverse case, offering a different insight to the roles of nurses providing care in a home environment [ 44 ]. Nurses in specially developed programmes to serve certain unique patient profiles, such as mental health and home ventilation, were excluded in this case.
Case D was managed under the main 1,500-bed tertiary hospital that anchored the central RHS. The hospital’s home-based care services had started with three silo programmes to serve post-discharge patients of different profiles: Aged Care Transition (ACTION), Virtual Hospital and Post-Acute Care at Home. The first programme aimed to provide case management service for patients with health and social care needs; the second programme targeted patients who were frequently admitted for chronic health conditions; and the third served to provide intensive medical and nursing care for clients with complex health care needs. The data collection was conducted after the merger of these three programmes into one transitional care team, allowing rich information to be collected. This team was led by nurses and supported by a multi-disciplinary team of doctors, pharmacists and allied health therapists in service provision. This service has also been financed by the H2H funding under the Ministry of Health since 2017. These RNs received in-house orientation and induction programme before they were merged into one department. They reviewed patients at their homes independently and work within escalation protocols for medical support through joint home visits and case discussions.
Purposive sampling was used to select participants. The inclusion criteria for the nurses were the following: (1) age of 21 years and above, (2) experience working as a nurse in transitional care services for more than 2 years and (3) provision of patient care for at least 24 hours a week to patients within the central RHS. The nurses were recruited for observations and follow-up interviews. Managers and other healthcare professionals (e.g. doctors, therapists and/or ancillary staff) were invited for interviews to elicit their perspectives on nurses’ work. Managers were included if they held key administrative positions in overseeing the department that governs nurses. The inclusion criteria for other healthcare professionals were the following: (1) age of 21 years and above, (2) working with a nurse participant and (3) provision of professional services under the organisation. Relevant documents, such as policies and forms that described the roles and practices of nurses in the last five years, were also examined.
Ethical consideration
Ethical approval for the study was obtained from the Institutional Review Board of the RHS (Ref. No.: 2016/01418). The potential participants had first been identified by the nursing manager based on the inclusion and exclusion criteria. The study was explained to the prospective participants, and written informed consent was obtained by the first author. Anonymity and confidentiality were assured through the use of codes to identify the participants. Verbal consent to observe the nurses’ work was obtained from patients or caregivers prior entry to their homes.
Data collection
Three data collection methods were used: non-participant observations of nurses by the first author, a registered nurse working in a tertiary hospital and doing her PhD project; individual interviews of nurses, managers and healthcare professionals; and a documentary analysis. Data collection continued to the point of data saturation, which was when the data set was completed and the research questions were answered [ 45 ]. The participants’ demographics were collected using self-completed demographic sheets.
Non-participant observations of the nurses during their regular working hours were undertaken for at least 24 hours a week. The first author asked them to provide care to patients as usual so that the data collected could genuinely reflect their practices. The first author followed each participant and observed their practices consecutively in a week. Two observation charts to document nurse-patient encounters during home visits and the nurses’ daily schedules were used to elicit the direct or non-direct care interventions and nursing work. Following the observations, the same nurses were interviewed individually based on a semi-structured interview guide to understand the ‘how’ and ‘why’ of the roles performed. Separate semi-structured interview guides were used for managers and healthcare professionals. All interviews were audio-recorded. Each interview lasted approximately 30–120 min. The interview guides were developed from the research questions and had been pilot-tested on a separate home hospice team, of which the findings were not used in this study. Lastly, documentary data were transcribed onto the data extraction form, which was constructed to capture relevant information on the work and roles of nurses [ 46 ].
Data analysis
A simple descriptive analysis using Microsoft Excel 2013 was conducted on the quantitative data from the participants’ demographic sheets and daily observational information. Audio recordings of the interviews were transcribed verbatim, and handwritten observation notes were typed into electronic text. A thematic analysis was then undertaken for the qualitative data using the six-phase data analytical method [ 47 ], incorporated with techniques of data condensation, data display and conclusion drawing [ 48 ]. QSR Nvivo 10 was used to organise the data.
First, data were collected by the first author to allow familiarity of the data [ 47 ]. Next, the first and third authors independently generated the initial codes before checking for agreement [ 48 ]. During the third step in searching for themes, different codes were sorted into potential units of analysis to discern pattern codes [ 47 , 48 ]. In the fourth step, three authors refined the themes by examining the levels of the coded data extracts to ensure coherence in its patterns and consider individual themes in relation to the data set as a whole [ 47 ]. The themes were defined in step five before concluding with a written report in step six. Pattern matching and explanation building were employed in the within-case analysis [ 49 ].
Methodological rigour
The four criteria of credibility, transferability, dependability and conformability were used to ensure the trustworthiness of the study [ 50 ]. Triangulation of the data collection methods and data sources was undertaken to enhance the credibility of the study [ 51 , 52 ]. Prolonged engagement was crucial to reduce the observer effect on the participants’ behaviours [ 53 ]. The authors undertook independent data analyses before coming together to ensure consistency in the coding and identification of themes [ 51 ]. The first author kept a research diary to enable the comprehension of the thoughts that led to the findings [ 51 ]. The study research design and findings are described in detail in the first author’s thesis [ 15 ] to allow for the transferability of the findings [ 54 ].
Demographic data of the participants and observation information
A total of four nurses were selected based on the inclusion and exclusion criteria, and they covered different geographical regions served by the central RHS. Two managers and three healthcare professionals who worked closely with these four nurses were interviewed. Table 1 presents the demographics of the participants. The nurse participants were observed over a total of 147 h ours over 17 days. Eleven home visits were made, with a mean duration of 54.55 min utes per home visit. A total of 11 relevant internal documents were reviewed here. These documents were mainly workflows, service manuals and induction materials.
Demographics of the participants.
Note : ‡ , range is not reported as the small numbers may reveal the identity of the participants; *, data not presented to ensure anonymity of the small number of participants.
Themes and sub-themes of Case D: RHS hospital transitional care team
The themes and sub-themes are presented in Table 2 . The nurses’ roles arose because of the need to come together in the integrated healthcare system ‘to meet the needs of all’. Case D was at the centre of all change forces, and the nurses’ roles were developing to be ‘strong amidst the stormy waves’. The nurses’ roles were still evolving and ‘searching for the right formula to handle the complexity’ in the integrated healthcare system.
Themes and sub-themes of Case D.
Theme 1: coming together to meet the needs of all
This theme describes the atypical roles undertaken by nurses in Case D (Sub-theme 1) and their attempts to close gaps and meet patients’ needs (Sub-theme 2).
Sub-theme 1: rising out of the norm
The observation of Case D nurses has demonstrated that the care delivered was beyond the traditional home visits, displaying the sub-theme of ‘out of the norm’. The nurses typically made only one visit for each patient as the first visit was considered free of charge for them. Therefore, during one single home visit, the nurses were observed to make a comprehensive health assessment, which included physical aspects, cognition, environmental safety, emotional well-being and social support system. As part of their role in care management, the nurses would promote adherence to chronic disease care plans by educating the patients and their caregivers. Ensuring medication adherence and reminding them of their appointments were significant components of their work. Coordination of care then followed to ensure that various health or social services were in place. Patients’ care management was executed mainly through telephone consultations.
Delivery of nursing care was not limited to direct contact with patients or caregivers at home visits or over the phone. The nurses were instrumental in discussing the patients with the multi-disciplinary team. A formal daily case discussion and weekly multi-disciplinary rounds (MDR) were held for each of the four sub-teams. Observations of the nurses also revealed that informal discussions with their multi-disciplinary team were common in the office.
‘The nurse went to speak to the occupational therapist in the office regarding a home visit for the patient. The nurse arranged the timing for the visit and updated her about the case. The nurse also updated her regarding another case.’ [Observation–Nurse03]
Proactive preventive care was observed as one of the nursing roles undertaken. The nurses received a national risk stratification list of hospitalised patients who might need services post-discharge. Each sub-team had a lead nurse to screen through the list and enrol patients with complex medical and social needs. As the service was developing, the nurses also participated in strategic development projects within the department as well as with other community providers.
Sub-theme 2: closing the gaps
There were unique features of the roles of the nurses, of which ‘closing the gaps’ was the most prominent observation. They made sure that the patients transited smoothly through various settings. Forming a safety net included addressing any new health concerns, providing health information and caregiver teaching and escalating rapidly to the medical team when these patients turned unstable. Although closing the gaps was the primary reason for the development of Case D, the nurses’ roles also addressed the current fragmentation of the integrated RHS.
‘Because if we cannot cross that bridge right, then we try other bridge that can support. If there aren’t any bridge that can support. Then it will be due to a limitation in the service, which is something geographically or politically or service limitation wise, we cannot do anything about it. We should just try our best to help the patients.’ [Interview–Manager02]
Closing the gaps has also meant that the nurses have moved away from the traditional manner of care delivery. Instead of solely functioning within a certain care setting, these nurses have worked in different settings such as inpatient wards, community settings and homes or via teleconsultation. The care network was expanded by their attendance at regular networking sessions and case discussions with the community providers and polyclinics (primary care). Although it was observed that the nurses spent much time on the telephone, these increased contacts have attempted to plug the gaps in the integrated RHS in which some patients had fallen through.
Theme 2: standing strong amidst the stormy waves
This theme has described how the nurses established their new roles in the face of various challenges, including the intense push for changes at the system and policy levels (Sub-theme 1), shaken foundation of the organisation (Sub-theme 2), remote influences of families (Sub-theme 3) and need to provide care to the most vulnerable patients (Sub-theme 4).
Sub-theme 1: moving along with the storm of change
The merger from the three programmes into one service was the most significant turning point for the nurses. This change was fuelled by the changing healthcare needs of the population. The participants echoed this, who explained that the patients were older and sicker and thus needed more care after hospitalisation. National programmes were introduced to expand the existing community healthcare services. Although the shift was welcomed, the nurses verbalised that the change in the funding structure has changed the care delivery. Programmes were nurse-led as the doctors’ visits were expensive. The free-of-charge nurse’s first visit was very intense to identify and address the patients’ biopsychosocial needs. One nurse also discussed her discomfort that her role was much determined by the cost of visits.
The governmental policies and funding on other primary and community services have exerted strong impacts on the nurses’ role. As the community services were run by non-for-profit organisations, different organisational sizes also meant different standards and capacities of the services. The disparate service capacities have resulted in some nurses holding on longer to their patients before handing them over to a suitable provider. Understanding the strengths and weaknesses of social services and working with them to improve their service scope has become part of their roles.
‘The networking is with the community partners most of the time… … that helped us to come to a consensus that this is the part that you will do and this is the part that I will do. We can come together and synergise, and benefit the patients.’ [Interview–Manager01]
Sub-theme 2: shaking a solid foundation
The expansion of the hospital outside of an institution setting has shaken its fundamental operating philosophy. The hospital was constantly setting new workflows, and regular briefing meetings were held. At times, there were uncertainties and confusion over the new and changing workflows by the team. Although the organisation has involved the nurses in the development of new workflows and processes, this also translated into heavier involvement in projects and meetings. The fast-paced changes have left nurses feeling overwhelmed.
‘I think it is not from them [managers], it is from the top management that will sometimes shake the team a little bit. How come it is last minute? How come we are the last team to know? That kind of feel. It will be good that the management can prepare us in advance on what is going to happen.’ [Interview–Manager02]
There was a shift in the model of care towards the nurse-led and team-based approach. One therapist shared that the doctors and therapists became consultative figures rather than directive ones. The shift in care delivery towards a team-based approach was evident. The managers, also known as the team leaders, have stood firm and resolute. They provided stability within the team by being the clinical support and by looking into nursing development to keep pace with rapid and constant changes. Standing firm amidst all of the changes and supporting the nurses in their roles were significant to maintain the cohesion of the team. They guided the nurses despite the lack of clarity.
‘I just have to make the boat works. If not, the whole boat will collapse. I cannot demonstrate that I am shaking. I just have to keep it going.’ [Interview–Manager02]
Sub-theme 3: maintaining a distant relationship
The relationship between the patients’ caregivers or families has exerted a lesser impact than other influences. Their main determining factor in establishing this relationship was often driven by the costs of the service. Even the enrolment and follow-up home visits were much decided by the family or caregivers. Regular updates and advice to family members and caregivers through telephone consults were commonly observed. The participants shared that these family members or caregivers have access to more health information via the internet. Communication via WhatsApp, text messages and emails were common. Because of the distant relationship, the nurses sometimes had little control of how the family members or caregivers managed the patients’ care.
‘The nurse made a phone call to arrange a home visit as the son reported that the patient passed less urine. The nurse was concerned of urinary retention and was planning to do a bladder scan. However the son refused the home visit.’ [Observation–Nurse04]
Sub-theme 4: sustaining a lifeline in the storm
The sub-theme ‘a lifeline in the storm’ describes the complex and challenging patients who depended on the nurses to prevent them from falling through gaps and weaknesses when the system has not integrated sufficiently to provide the care required by these patients. This particular group of patients often had extreme social circumstances or demonstrated non-adherence to lifestyle modifications or medications, leading to frequent disease exacerbations and hospital admissions. The patients’ multiple medical conditions sometimes limited the use of standard care plans. The patients had complex biopsychosocial needs such that several community services had to be in place. The nurses undertook the role as the single point of contact.
‘One point of contact. By doing so, patients… by being one point of contact…… they don’t need to remember so many nurses’ names. And what we are dealing with are elderly, who tends to be more forgetful.’ [Interview–Nurse02]
To meet the needs of these complex patients, the nurses first built a rapport with the patients. The nurses made contact with these patients in the wards before they were discharged and addressed their concerns when they encountered problems at home. One nurse described herself as ‘being a phone call away’. Thereafter, they would empower the patients in managing their own health. In a short transitional care period, they have ensured that patients were stable before handing over to a long-term care provider.
Theme 3: searching for the right formula in handling complexity
Case D has faced a number of complex changes as the RHS developed (Sub-theme 1) and working within a team and with several teams (Sub-theme 2). Their emerging roles in providing care differed from the norm (Sub-theme 3). Their evolving roles were still fraught with uncertainty, thus giving rise to the overarching theme of ‘searching for the right formula in handling complexity’.
Sub-theme 1: facing complexity at its prime
‘Complexity at its prime’ describes the pubescent stage of the changes in healthcare after the re-clustering in January 2017. The lack of awareness of other community services and their service capabilities was common. This was further hampered by the lack of system links between them, such that the nurses sometimes did not know the services received by the patients. The medical information documented by the community providers was not available on the National Electronic Health Records. Thus, the onus fell back on the nurses to communicate with the community providers to gather information. However, the constant and dynamic change was only the beginning as more upcoming changes were announced during the data collection period.
It is evident that the boundaries of work between different organisations and the rules in each organisation within the RHS have begun to change, leading to further complexity. It was observed that it was unclear whether certain nursing services were still within the scope. Protocols and workflows were continuously developed or modified. As the boundaries between the different organisations became blurred within the integrated system, there were duplications and gaps of services at times. The adaptability of the nurses came in useful when rules were unclear. In addition, the nurses were observed to display self-organising abilities and interacting within their own sub-teams and with other community providers. However, during such self-organisation and adaptation, one significant observation was that nurses unable to adapt effectively also departed from the system.
‘Those [Nurses] who have eventually left. I would not say that because they cannot make it. It is because I think that there is something that they think it is not something for them.’ [Interview Nurse02]
Sub-theme 2: teaming with teams
The nurses have formed a team that worked with several teams, thus giving rise to the sub-theme ‘team of teams’. Besides seeing the patients at home, they would assess the patients in the wards or clinics and hold case discussions with hospital teams or primary care teams. The nurses were recognised as the single source of contact and were supported by other healthcare professionals. Their role as a catalyst to other teams was also observed. In the community, they frequently collaborated with other homecare nurses and primary care and community providers. For ways to connect with them, other than the face-to-face physical presence in the wards or clinics, formal methods included holding joint MDR or teleconsultations. For more complex patients, joint home visits were made. The nurses usually followed up by speaking to the staff to discuss the patients after these formal communications. The various ways of communicating with several teams emphasised the role of nurses as good communicators.
‘My efforts might be limited by one self. Let’s say I gather a team of community partners. Together with community partners, working with them, to let them know that there is a shared common patient goal, then they help with whichever means of expertise. [Interview–Nurse03]
Sub-theme 3: emerging differently
As the hospital developed its community services in tandem with the integrated healthcare system, new roles were emerging. Because of the focus on integration and collaboration, the ways through which the nurses conducted their usual assessment have changed. Possible enrolment into the service was no longer only referred but was identified by a national risk stratification tool. These patients had to be assessed proactively to look for any unidentified needs and refer appropriately to the various community services.
‘As the patients’ conditions get more complex, the complex care does not allow the nurses to be so hospital-based, clinic-based. Rather be more proactive. Proactive to go in and be more engaging with the patients……. To elicit the behavioural changes in getting well.’ [Interview–Nurse03]
The drive towards integrated care has meant that the nurses have to coordinate with both the specialists and community partners. Working in such a grey zone has meant that their caseloads were always shared. In this multi-prolonged integrative work, the physical presence and contacts of the nurses could be observed at different parts of the integrated RHS. The observations had shown that their roles were required to cover the current gaps in the integrated RHS when other providers were unable to provide the services on time.
The research aimed to understand the changing roles of transitional care nurses in the integrated healthcare system. Key insights were gained on their roles, the systems in which they worked and the evolution of their roles as the integrated RHS developed.
Diverse nursing roles have been reported in the literature as new community programmes and initiatives were implemented to facilitate the transition of care between settings [ 12 , 19 , 20 , 21 , 23 , 24 , 25 , 26 , 27 , 33 ]. The health assessment, telephonic support, coordination and chronic disease management roles were similarly performed by nurses in Case D. Proactive recruitment was also in place to identify at-risk patients using predictive tools and early institution of preventive measures. The literature has also witnessed this increasing shift of roles from passive and reactive to proactive care [ 20 , 21 , 33 ]. Emphasis was also placed on discharge planning and coordinating with other professionals to prepare patients and caregivers for their post-discharge care [ 12 ]. More studies should be conducted on the importance of this anticipatory and integrative role by transitional care nurses to ensure other care partners to take over patients’ care when they bridge from hospital to community.
The findings have shown that the nurses in Case D have extended from clinically-focused roles and holistic direct patient care activities to other new roles in networking, project planning and representation in workgroup and committees. A ‘rising out of the norm’ may be the new working philosophy to place nurses as key players in developing integrated care. The nurses’ roles in Case D were unique when they were ‘closing the gaps’ through their provision of interim nursing interventions, using different forms of care delivery and working in different care settings. Nurses often bridged the gaps and worked between boundaries of health and social care [ 55 ]. In addition, Case D nurses have taken on the system roles in working with care partners to close the gaps through the development of collaborative partnerships and were beyond the usually described direct patient-nurse care in literature [ 12 , 23 , 24 , 25 , 26 , 27 ].
The findings have highlighted the impact of the restructuring of the healthcare system towards community care on the roles of nurses. Studies have similarly outlined the possible socio-political influences on nurses’ roles [ 56 , 57 ]. Findings have shown that nurses played a role not only in their organisations but also in the integrated RHS by partaking in collaborative meetings and developing services and workflows with other community partners. It was evident that these new and expanded roles of the transitional care nurses have been introduced as a result of the change in the funding system for various programmes. Although such increased funding has been welcomed to drive the rapid shift to community care, Schofield et al. (2011) have cautioned that community programmes were often suspended when competing demands for funds emerged [ 58 ]. Confusion created by the lack of well-developed program direction and protocols was similarly observed in other national transitional care programme [ 25 ]. Such policy and system changes have to be managed carefully so as not to place nurses in an uncertain state of change.
The presence of nursing managers and leaders was significant in fostering the growth and development of the roles of nurses in the integrated care system. A qualitative study has shown that leadership in community nursing was crucial in how policies are delivered and how leaders have translated the policies into action plans for frontline community nurses to deliver care [ 59 ]. In this study, the team leaders concurrently managed the senior management upstream and nurses in their teams downstream. The effect of the patterns of the patients’ family and caregivers on the roles of nurses is noteworthy. Similar to other Asian studies, family members were heavily involved in medical decision-making [ 60 ], and the hired foreign domestic workers and themselves were the direct care providers in home settings [ 61 ]. Although cost was often stated not as a barrier for patients to receive care [ 25 ], negotiations with the family to provide services have fallen on the nurses who have to balance between professional obligations and the family’s financial concerns.
The development of the integrated RHS on nursing roles and possible mechanisms of change were examined through the lens of complexity science and the role theory. The changes in the roles were largely complex, even though some form of structure and order was present. CAS theorists have highlighted that the organisational structures and processes have facilitated informal exchanges and interactions [ 62 , 63 , 64 ]. This research has demonstrated that the nurses have expanded linkages throughout the integrated RHS with a high amount and level of interactions undertaken. Although it may appear chaotic, there were actually ‘order within chaos’ as the nurses self-organised their work towards integrated care [ 65 ].
Adaptable and self-organising attributes of the nurses have been observed to ‘emerge differently’ in this new complex integrated care system. The roles of the nurses in various programmes in Case D were merged as one, and new roles were introduced. It was observed that establishing new nursing roles was also a dynamic process as the integrated healthcare system develops. Although it is tempting to reduce complexity and ensure certainty by managing persons and creating structures [ 66 ], the findings have suggested that broad frameworks and healthcare policies should be provided to allow local adaptability yet prevent wide variations in the roles of nurses [ 43 , 67 ]. In addition, the processes should only be formalised when necessary: this will avoid having several prohibitive workflows and formal guidelines that add to administrative work but serve little clinical purpose.
The strengths of this study were that this research took place when the RHS underwent organisational changes. It is also noteworthy that this study has afforded valuable insights into nurses who provided care at home in an Asian context. The findings have also informed the importance of transitional nursing interventions in integrated care systems, and these roles should be further emphasised in the national community nursing scope of practice and development. This study also revealed the significance of organisational structures and policies in influencing the roles of transitional care nurses. Adequate support in terms of educational preparation and continued expansion of their roles should be undertaken.
Although the limitation of generalisation due to the small number of nurses is present, a longer observation period of over a week per nurse has been undertaken. Although it is recognised that the findings reported here might be limited to a single case study, the first author has conducted three similar case studies to provide the cross-case comparison in her final thesis and further modified the CAS conceptual framework ( Figure 4 ). More studies are recommended using the framework, given the complexity of healthcare services and systems. Lastly, it is recommended that future studies on nursing roles should include observation as a data collection method instead of solely depending on interview methods as this method allows accurate capturing of multiple roles.

Proposed conceptual framework of the changing homecare nursing roles in an integrated regional health system (RHS).
The study has demonstrated the shift in the roles of transitional care nurses as the healthcare system grows increasingly complex and the replacement of linear thinking models with complexity science. The evolvement of the roles of nurses will be continuous and dynamic as different influencing factors come together and interact at varying strengths. The findings have contributed to developing the conceptual framework, which will enhance understanding the shift of nurses roles as the integrated care system develops. Further studies on the evolvement of nursing roles as the integrated RHS develops are strongly recommended to provide insights to future policy designs and nursing profession advancement.
Marlène Karam, inf., Ph.D. Professeure adjointe, Faculté des sciences infirmières, Université de Montréal, Canada.
Elodie Montaigne, Registered Nurse, MSc, PhD student in Community Health, Laval University, VITAM Research Center on Sustainable Health Qc, Canada and Visiting Lecturer, University of Rennes 1, France.
Competing Interests
The authors have no competing interests to declare.

COMMENTS
Ensure your summary has at least the case presentation, the nursing assessment/diagnosis, the intervention, and the key recommendations. At the very end of your conclusion, add a closing statement. The statement should wrap up the whole thing nicely. Try to make it as impressive as possible. 9.
Writing a nursing case study analysis usually takes only a few hours. Reference your case study. After writing your case study, make sure you add all in-text citations if you had not added them already. And when adding them, you should make sure you follow the style/format recommended in the assignment prompt (usually APA or Harvard style).
The title of the case study should be concise, descriptive, and reflective of its main focus. Include your name, academic credentials, and the institution where you are studying. Provide the date of submission. Abstract. Write a brief summary (usually 150-300 words) of the case study.
The nursing case study example on Death and Dying and answers questions on Suffering and the Fallenness of the World, Suffering and the Hope of Resurrection, Value of Life, Euthanasia, and Morally Justified Options, also offers an analysis of the sin of suicide. Explores Ethical end of life decision making.
A few key parts portray these contextual analyses, each assuming a critical part in understanding patient considerations and illuminating clinical navigation. 1. Right off the bat, the patient ...
Case study is a research methodology, typically seen in social and life sciences. There is no one definition of case study research.1 However, very simply... 'a case study can be defined as an intensive study about a person, a group of people or a unit, which is aimed to generalize over several units' .1 A case study has also been described ...
The parts of each case study can also be used independently of each other to facilitate problem solving. ... The way that the scenarios are explained could even be understood by a non-nursing student as well. The case studies are very clear and very thorough. Interface rating: 5 The book is very easy to navigate, prints well on paper, and is ...
Nursing Case Study Your patient is a 48-year-old premenopausal, multiparous female suffering from urinary stress incontinence. She has been doing pelvic floor exercises on her own, following instructions on a patient education handout she got from her doctor, to improve the symptoms, but she is not happy with the results and isn't sure if she is doing the exercises correctly.
Author Affiliation: Senior Nurse Scientist, Department of Nursing Research and Innovation, Cleveland Clinic, Ohio. Dr Siedlecki is a senior nurse scientist at the Cleveland Clinic who maintains her own program of research and serves as a consultant and mentor to clinical nurses who are planning and conducting bedside research.
'Case-study is the study of the particularity and complexity of a single case, coming to understand its activity within important circumstances.' Stake (1995, p.xi) 'Case-study is an 'intensive study of a single unit for the purpose of understanding a larger class of units' Gerring (2004) 'Case-study is an empirical inquiry that:
A nursing case study paper contains several sections that fall into three categories: 1. The status of the patient. Demographic data. Medical History. Current diagnosis and treatment. 2. The nursing assessment of the patient. Vital signs and test results.
HE003: Delivery of Services - Emmanuel is 55-year-old man Case - With Solution The Extent of Evidence-Based Data for Proposed Interventions - Sample Assignment 1 Solution. Planning Model for Population Health Management Veterans Diagnosed with Non cancerous chronic pain - Part 1 & 2 Solutions.
The Ongoing Case Studies are designed to simulate an actual case that you might encounter in a clinical setting. Rather than simply test the knowledge that you acquired in nursing school—which is also important—the case study progresses from your first interaction with a client through your evaluation of the outcomes.
Click on a case study below to view in our Nursing Case Study Examples course which holds all of our 40+ nursing case studies with answers. Acute Kidney Injury Nursing Case Study. Continue Case Study. Cardiogenic Shock Nursing Case Study. Continue Case Study. Breast Cancer Nursing Case Study. Continue Case Study. Respiratory Nursing Case Study.
White Paper Using Case Studies to Develop Clinical Judgment and Ensure Next eneration NCLEX ® NGN) Success 2 Background In 2010, the results of a large study of nursing education in the United States were summarized in Educating Nurses: A Call for Radical Transformation (Benner, et al., 2010).One of the key findings was that nurses entering practice do not
A case report is a detailed report of the symptoms, signs, diagnosis, treatment, and follow-up of an individual patient. Case reports usually describe an unusual or novel occurrence and as such, remain one of the cornerstones of medical progress and provide many new ideas in medicine. Some reports contain an extensive review of the relevant ...
NGN case studies present a realistic patient scenario that you must navigate, step by step, starting with identifying and analyzing relevant client information, then planning and providing treatment, and lastly evaluating client outcomes. The result is a six-question set that requires you to: 1. 1. Recognize Cues.
This video introduces the concept of the case study in a nursing context, but concepts are applicable to other areas. It identifies how case studies differ ...
A nursing case study is a detailed study of an individual patient, which allows you to gain more information about the symptoms and the medical history of a patient and provide the proper diagnoses of the patient's illness based on the symptoms he or she experienced and other affecting factors. Learn more about this type of research by reading the article.
2. BACKGROUND. Case studies have been widely used in nursing theory training because they help students to build on the basic knowledge taught and to collect information and analyse it to make diagnoses and support interventions (O'Rourke & Zerwic, 2016).In addition, there is considerable research on the use of case studies in simulation settings, which are practical environments where ...
Case study is a research methodology, typically seen in social and life sciences. There is no one definition of case study research.1 However, very simply… 'a case study can be defined as an intensive study about a person, a group of people or a unit, which is aimed to generalize over several units'.1 A case study has also been described as an intensive, systematic investigation of a ...
Case Studies. 02 April 2023. Case Studies. Gema Munoz-Mozas. Colin Fairhurst. Simon Clare. References. Intravenous (IV) access, both peripheral and central, is an integral part of the patient care pathways for diagnosing and treating cancer. Patients receiving systemic anticancer treatment (SACT) are at risk for developing infections, which may ...
With the need to provide holistic and coordinated care, nursing teams have evolved from a traditional flattened structure of nurses to multi-skilled and multi-professional teams [].The elderly often require coordination of care among multiple healthcare and social-care providers [] and transitional care from the hospital to home [].This has also accentuated the role of nurses in care ...
Given the importance of ethics and the protection of human rights in nursing practice, the American Nurses Association is urging RNs to join ANA President Pamela F. Cipriano, PhD, RN, NEA-BC, FAAN, and ANA Chief Executive Officer Marla J. Weston, PhD, RN, FAAN, in signing on to the Health Professionals' Pledge Against Torture.
With a bachelor's degree in business or a Master of Business Administration (MBA), you can expect to take courses in finance, marketing, management, accounting, entrepreneurship, and business strategy, and build up expertise in one or more areas.. Beyond subject knowledge, both kinds of degrees are designed for you to strengthen key skills, including critical and creative thinking, problem ...