Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, generate accurate citations for free.
- Knowledge Base
Methodology
- Types of Interviews in Research | Guide & Examples

Types of Interviews in Research | Guide & Examples
Published on March 10, 2022 by Tegan George . Revised on June 22, 2023.
An interview is a qualitative research method that relies on asking questions in order to collect data . Interviews involve two or more people, one of whom is the interviewer asking the questions.
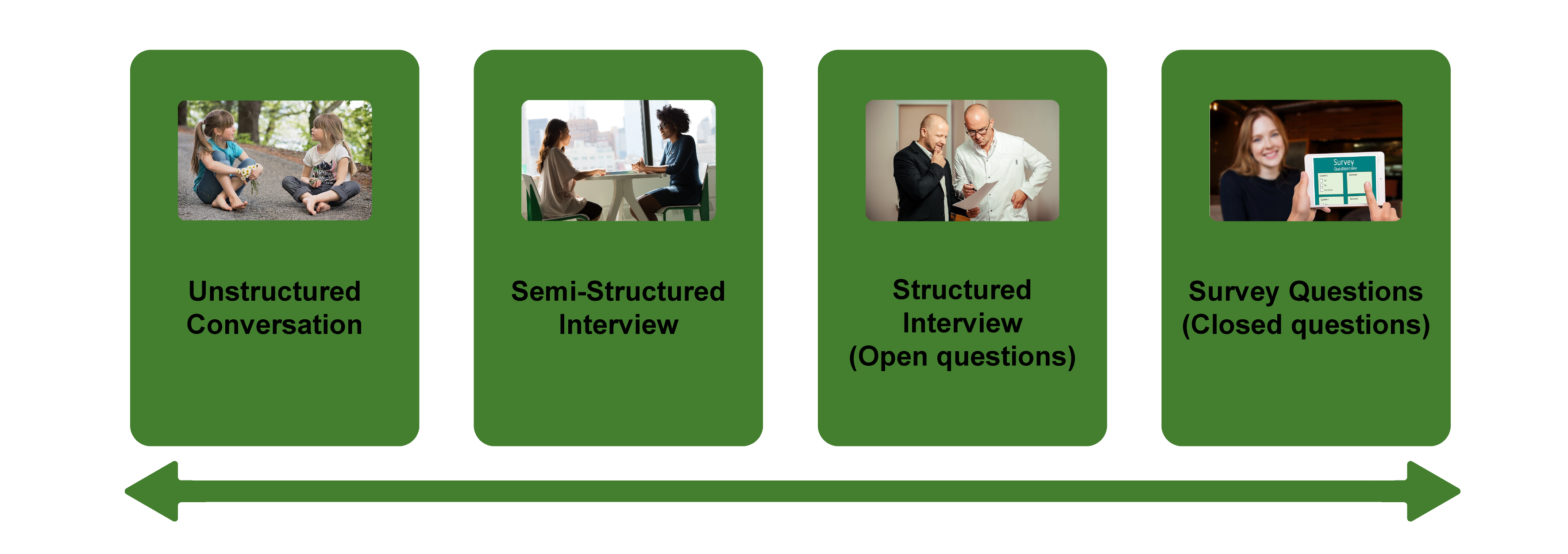
There are several types of interviews, often differentiated by their level of structure.
- Structured interviews have predetermined questions asked in a predetermined order.
- Unstructured interviews are more free-flowing.
- Semi-structured interviews fall in between.
Interviews are commonly used in market research, social science, and ethnographic research .
Table of contents
What is a structured interview, what is a semi-structured interview, what is an unstructured interview, what is a focus group, examples of interview questions, advantages and disadvantages of interviews, other interesting articles, frequently asked questions about types of interviews.
Structured interviews have predetermined questions in a set order. They are often closed-ended, featuring dichotomous (yes/no) or multiple-choice questions. While open-ended structured interviews exist, they are much less common. The types of questions asked make structured interviews a predominantly quantitative tool.
Asking set questions in a set order can help you see patterns among responses, and it allows you to easily compare responses between participants while keeping other factors constant. This can mitigate research biases and lead to higher reliability and validity. However, structured interviews can be overly formal, as well as limited in scope and flexibility.
- You feel very comfortable with your topic. This will help you formulate your questions most effectively.
- You have limited time or resources. Structured interviews are a bit more straightforward to analyze because of their closed-ended nature, and can be a doable undertaking for an individual.
- Your research question depends on holding environmental conditions between participants constant.
Receive feedback on language, structure, and formatting
Professional editors proofread and edit your paper by focusing on:
- Academic style
- Vague sentences
- Style consistency
See an example

Semi-structured interviews are a blend of structured and unstructured interviews. While the interviewer has a general plan for what they want to ask, the questions do not have to follow a particular phrasing or order.
Semi-structured interviews are often open-ended, allowing for flexibility, but follow a predetermined thematic framework, giving a sense of order. For this reason, they are often considered “the best of both worlds.”
However, if the questions differ substantially between participants, it can be challenging to look for patterns, lessening the generalizability and validity of your results.
- You have prior interview experience. It’s easier than you think to accidentally ask a leading question when coming up with questions on the fly. Overall, spontaneous questions are much more difficult than they may seem.
- Your research question is exploratory in nature. The answers you receive can help guide your future research.
An unstructured interview is the most flexible type of interview. The questions and the order in which they are asked are not set. Instead, the interview can proceed more spontaneously, based on the participant’s previous answers.
Unstructured interviews are by definition open-ended. This flexibility can help you gather detailed information on your topic, while still allowing you to observe patterns between participants.
However, so much flexibility means that they can be very challenging to conduct properly. You must be very careful not to ask leading questions, as biased responses can lead to lower reliability or even invalidate your research.
- You have a solid background in your research topic and have conducted interviews before.
- Your research question is exploratory in nature, and you are seeking descriptive data that will deepen and contextualize your initial hypotheses.
- Your research necessitates forming a deeper connection with your participants, encouraging them to feel comfortable revealing their true opinions and emotions.
A focus group brings together a group of participants to answer questions on a topic of interest in a moderated setting. Focus groups are qualitative in nature and often study the group’s dynamic and body language in addition to their answers. Responses can guide future research on consumer products and services, human behavior, or controversial topics.
Focus groups can provide more nuanced and unfiltered feedback than individual interviews and are easier to organize than experiments or large surveys . However, their small size leads to low external validity and the temptation as a researcher to “cherry-pick” responses that fit your hypotheses.
- Your research focuses on the dynamics of group discussion or real-time responses to your topic.
- Your questions are complex and rooted in feelings, opinions, and perceptions that cannot be answered with a “yes” or “no.”
- Your topic is exploratory in nature, and you are seeking information that will help you uncover new questions or future research ideas.
Prevent plagiarism. Run a free check.
Depending on the type of interview you are conducting, your questions will differ in style, phrasing, and intention. Structured interview questions are set and precise, while the other types of interviews allow for more open-endedness and flexibility.
Here are some examples.
- Semi-structured
- Unstructured
- Focus group
- Do you like dogs? Yes/No
- Do you associate dogs with feeling: happy; somewhat happy; neutral; somewhat unhappy; unhappy
- If yes, name one attribute of dogs that you like.
- If no, name one attribute of dogs that you don’t like.
- What feelings do dogs bring out in you?
- When you think more deeply about this, what experiences would you say your feelings are rooted in?
Interviews are a great research tool. They allow you to gather rich information and draw more detailed conclusions than other research methods, taking into consideration nonverbal cues, off-the-cuff reactions, and emotional responses.
However, they can also be time-consuming and deceptively challenging to conduct properly. Smaller sample sizes can cause their validity and reliability to suffer, and there is an inherent risk of interviewer effect arising from accidentally leading questions.
Here are some advantages and disadvantages of each type of interview that can help you decide if you’d like to utilize this research method.
| Type of interview | Advantages | Disadvantages |
|---|---|---|
| Structured interview | ||
| Semi-structured interview | , , , and | |
| Unstructured interview | , , , and | |
| Focus group | , , and , since there are multiple people present |
If you want to know more about statistics , methodology , or research bias , make sure to check out some of our other articles with explanations and examples.
- Student’s t -distribution
- Normal distribution
- Null and Alternative Hypotheses
- Chi square tests
- Confidence interval
- Quartiles & Quantiles
- Cluster sampling
- Stratified sampling
- Data cleansing
- Reproducibility vs Replicability
- Peer review
- Prospective cohort study
Research bias
- Implicit bias
- Cognitive bias
- Placebo effect
- Hawthorne effect
- Hindsight bias
- Affect heuristic
- Social desirability bias
The four most common types of interviews are:
- Structured interviews : The questions are predetermined in both topic and order.
- Semi-structured interviews : A few questions are predetermined, but other questions aren’t planned.
- Unstructured interviews : None of the questions are predetermined.
- Focus group interviews : The questions are presented to a group instead of one individual.
The interviewer effect is a type of bias that emerges when a characteristic of an interviewer (race, age, gender identity, etc.) influences the responses given by the interviewee.
There is a risk of an interviewer effect in all types of interviews , but it can be mitigated by writing really high-quality interview questions.
Social desirability bias is the tendency for interview participants to give responses that will be viewed favorably by the interviewer or other participants. It occurs in all types of interviews and surveys , but is most common in semi-structured interviews , unstructured interviews , and focus groups .
Social desirability bias can be mitigated by ensuring participants feel at ease and comfortable sharing their views. Make sure to pay attention to your own body language and any physical or verbal cues, such as nodding or widening your eyes.
This type of bias can also occur in observations if the participants know they’re being observed. They might alter their behavior accordingly.
A focus group is a research method that brings together a small group of people to answer questions in a moderated setting. The group is chosen due to predefined demographic traits, and the questions are designed to shed light on a topic of interest. It is one of 4 types of interviews .
Quantitative research deals with numbers and statistics, while qualitative research deals with words and meanings.
Quantitative methods allow you to systematically measure variables and test hypotheses . Qualitative methods allow you to explore concepts and experiences in more detail.
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the “Cite this Scribbr article” button to automatically add the citation to our free Citation Generator.
George, T. (2023, June 22). Types of Interviews in Research | Guide & Examples. Scribbr. Retrieved June 9, 2024, from https://www.scribbr.com/methodology/interviews-research/
Is this article helpful?
Tegan George
Other students also liked, unstructured interview | definition, guide & examples, structured interview | definition, guide & examples, semi-structured interview | definition, guide & examples, get unlimited documents corrected.
✔ Free APA citation check included ✔ Unlimited document corrections ✔ Specialized in correcting academic texts

Chapter 11. Interviewing
Introduction.
Interviewing people is at the heart of qualitative research. It is not merely a way to collect data but an intrinsically rewarding activity—an interaction between two people that holds the potential for greater understanding and interpersonal development. Unlike many of our daily interactions with others that are fairly shallow and mundane, sitting down with a person for an hour or two and really listening to what they have to say is a profound and deep enterprise, one that can provide not only “data” for you, the interviewer, but also self-understanding and a feeling of being heard for the interviewee. I always approach interviewing with a deep appreciation for the opportunity it gives me to understand how other people experience the world. That said, there is not one kind of interview but many, and some of these are shallower than others. This chapter will provide you with an overview of interview techniques but with a special focus on the in-depth semistructured interview guide approach, which is the approach most widely used in social science research.
An interview can be variously defined as “a conversation with a purpose” ( Lune and Berg 2018 ) and an attempt to understand the world from the point of view of the person being interviewed: “to unfold the meaning of peoples’ experiences, to uncover their lived world prior to scientific explanations” ( Kvale 2007 ). It is a form of active listening in which the interviewer steers the conversation to subjects and topics of interest to their research but also manages to leave enough space for those interviewed to say surprising things. Achieving that balance is a tricky thing, which is why most practitioners believe interviewing is both an art and a science. In my experience as a teacher, there are some students who are “natural” interviewers (often they are introverts), but anyone can learn to conduct interviews, and everyone, even those of us who have been doing this for years, can improve their interviewing skills. This might be a good time to highlight the fact that the interview is a product between interviewer and interviewee and that this product is only as good as the rapport established between the two participants. Active listening is the key to establishing this necessary rapport.
Patton ( 2002 ) makes the argument that we use interviews because there are certain things that are not observable. In particular, “we cannot observe feelings, thoughts, and intentions. We cannot observe behaviors that took place at some previous point in time. We cannot observe situations that preclude the presence of an observer. We cannot observe how people have organized the world and the meanings they attach to what goes on in the world. We have to ask people questions about those things” ( 341 ).
Types of Interviews
There are several distinct types of interviews. Imagine a continuum (figure 11.1). On one side are unstructured conversations—the kind you have with your friends. No one is in control of those conversations, and what you talk about is often random—whatever pops into your head. There is no secret, underlying purpose to your talking—if anything, the purpose is to talk to and engage with each other, and the words you use and the things you talk about are a little beside the point. An unstructured interview is a little like this informal conversation, except that one of the parties to the conversation (you, the researcher) does have an underlying purpose, and that is to understand the other person. You are not friends speaking for no purpose, but it might feel just as unstructured to the “interviewee” in this scenario. That is one side of the continuum. On the other side are fully structured and standardized survey-type questions asked face-to-face. Here it is very clear who is asking the questions and who is answering them. This doesn’t feel like a conversation at all! A lot of people new to interviewing have this ( erroneously !) in mind when they think about interviews as data collection. Somewhere in the middle of these two extreme cases is the “ semistructured” interview , in which the researcher uses an “interview guide” to gently move the conversation to certain topics and issues. This is the primary form of interviewing for qualitative social scientists and will be what I refer to as interviewing for the rest of this chapter, unless otherwise specified.
Informal (unstructured conversations). This is the most “open-ended” approach to interviewing. It is particularly useful in conjunction with observational methods (see chapters 13 and 14). There are no predetermined questions. Each interview will be different. Imagine you are researching the Oregon Country Fair, an annual event in Veneta, Oregon, that includes live music, artisan craft booths, face painting, and a lot of people walking through forest paths. It’s unlikely that you will be able to get a person to sit down with you and talk intensely about a set of questions for an hour and a half. But you might be able to sidle up to several people and engage with them about their experiences at the fair. You might have a general interest in what attracts people to these events, so you could start a conversation by asking strangers why they are here or why they come back every year. That’s it. Then you have a conversation that may lead you anywhere. Maybe one person tells a long story about how their parents brought them here when they were a kid. A second person talks about how this is better than Burning Man. A third person shares their favorite traveling band. And yet another enthuses about the public library in the woods. During your conversations, you also talk about a lot of other things—the weather, the utilikilts for sale, the fact that a favorite food booth has disappeared. It’s all good. You may not be able to record these conversations. Instead, you might jot down notes on the spot and then, when you have the time, write down as much as you can remember about the conversations in long fieldnotes. Later, you will have to sit down with these fieldnotes and try to make sense of all the information (see chapters 18 and 19).
Interview guide ( semistructured interview ). This is the primary type employed by social science qualitative researchers. The researcher creates an “interview guide” in advance, which she uses in every interview. In theory, every person interviewed is asked the same questions. In practice, every person interviewed is asked mostly the same topics but not always the same questions, as the whole point of a “guide” is that it guides the direction of the conversation but does not command it. The guide is typically between five and ten questions or question areas, sometimes with suggested follow-ups or prompts . For example, one question might be “What was it like growing up in Eastern Oregon?” with prompts such as “Did you live in a rural area? What kind of high school did you attend?” to help the conversation develop. These interviews generally take place in a quiet place (not a busy walkway during a festival) and are recorded. The recordings are transcribed, and those transcriptions then become the “data” that is analyzed (see chapters 18 and 19). The conventional length of one of these types of interviews is between one hour and two hours, optimally ninety minutes. Less than one hour doesn’t allow for much development of questions and thoughts, and two hours (or more) is a lot of time to ask someone to sit still and answer questions. If you have a lot of ground to cover, and the person is willing, I highly recommend two separate interview sessions, with the second session being slightly shorter than the first (e.g., ninety minutes the first day, sixty minutes the second). There are lots of good reasons for this, but the most compelling one is that this allows you to listen to the first day’s recording and catch anything interesting you might have missed in the moment and so develop follow-up questions that can probe further. This also allows the person being interviewed to have some time to think about the issues raised in the interview and go a little deeper with their answers.
Standardized questionnaire with open responses ( structured interview ). This is the type of interview a lot of people have in mind when they hear “interview”: a researcher comes to your door with a clipboard and proceeds to ask you a series of questions. These questions are all the same whoever answers the door; they are “standardized.” Both the wording and the exact order are important, as people’s responses may vary depending on how and when a question is asked. These are qualitative only in that the questions allow for “open-ended responses”: people can say whatever they want rather than select from a predetermined menu of responses. For example, a survey I collaborated on included this open-ended response question: “How does class affect one’s career success in sociology?” Some of the answers were simply one word long (e.g., “debt”), and others were long statements with stories and personal anecdotes. It is possible to be surprised by the responses. Although it’s a stretch to call this kind of questioning a conversation, it does allow the person answering the question some degree of freedom in how they answer.
Survey questionnaire with closed responses (not an interview!). Standardized survey questions with specific answer options (e.g., closed responses) are not really interviews at all, and they do not generate qualitative data. For example, if we included five options for the question “How does class affect one’s career success in sociology?”—(1) debt, (2) social networks, (3) alienation, (4) family doesn’t understand, (5) type of grad program—we leave no room for surprises at all. Instead, we would most likely look at patterns around these responses, thinking quantitatively rather than qualitatively (e.g., using regression analysis techniques, we might find that working-class sociologists were twice as likely to bring up alienation). It can sometimes be confusing for new students because the very same survey can include both closed-ended and open-ended questions. The key is to think about how these will be analyzed and to what level surprises are possible. If your plan is to turn all responses into a number and make predictions about correlations and relationships, you are no longer conducting qualitative research. This is true even if you are conducting this survey face-to-face with a real live human. Closed-response questions are not conversations of any kind, purposeful or not.
In summary, the semistructured interview guide approach is the predominant form of interviewing for social science qualitative researchers because it allows a high degree of freedom of responses from those interviewed (thus allowing for novel discoveries) while still maintaining some connection to a research question area or topic of interest. The rest of the chapter assumes the employment of this form.
Creating an Interview Guide
Your interview guide is the instrument used to bridge your research question(s) and what the people you are interviewing want to tell you. Unlike a standardized questionnaire, the questions actually asked do not need to be exactly what you have written down in your guide. The guide is meant to create space for those you are interviewing to talk about the phenomenon of interest, but sometimes you are not even sure what that phenomenon is until you start asking questions. A priority in creating an interview guide is to ensure it offers space. One of the worst mistakes is to create questions that are so specific that the person answering them will not stray. Relatedly, questions that sound “academic” will shut down a lot of respondents. A good interview guide invites respondents to talk about what is important to them, not feel like they are performing or being evaluated by you.
Good interview questions should not sound like your “research question” at all. For example, let’s say your research question is “How do patriarchal assumptions influence men’s understanding of climate change and responses to climate change?” It would be worse than unhelpful to ask a respondent, “How do your assumptions about the role of men affect your understanding of climate change?” You need to unpack this into manageable nuggets that pull your respondent into the area of interest without leading him anywhere. You could start by asking him what he thinks about climate change in general. Or, even better, whether he has any concerns about heatwaves or increased tornadoes or polar icecaps melting. Once he starts talking about that, you can ask follow-up questions that bring in issues around gendered roles, perhaps asking if he is married (to a woman) and whether his wife shares his thoughts and, if not, how they negotiate that difference. The fact is, you won’t really know the right questions to ask until he starts talking.
There are several distinct types of questions that can be used in your interview guide, either as main questions or as follow-up probes. If you remember that the point is to leave space for the respondent, you will craft a much more effective interview guide! You will also want to think about the place of time in both the questions themselves (past, present, future orientations) and the sequencing of the questions.
Researcher Note
Suggestion : As you read the next three sections (types of questions, temporality, question sequence), have in mind a particular research question, and try to draft questions and sequence them in a way that opens space for a discussion that helps you answer your research question.
Type of Questions
Experience and behavior questions ask about what a respondent does regularly (their behavior) or has done (their experience). These are relatively easy questions for people to answer because they appear more “factual” and less subjective. This makes them good opening questions. For the study on climate change above, you might ask, “Have you ever experienced an unusual weather event? What happened?” Or “You said you work outside? What is a typical summer workday like for you? How do you protect yourself from the heat?”
Opinion and values questions , in contrast, ask questions that get inside the minds of those you are interviewing. “Do you think climate change is real? Who or what is responsible for it?” are two such questions. Note that you don’t have to literally ask, “What is your opinion of X?” but you can find a way to ask the specific question relevant to the conversation you are having. These questions are a bit trickier to ask because the answers you get may depend in part on how your respondent perceives you and whether they want to please you or not. We’ve talked a fair amount about being reflective. Here is another place where this comes into play. You need to be aware of the effect your presence might have on the answers you are receiving and adjust accordingly. If you are a woman who is perceived as liberal asking a man who identifies as conservative about climate change, there is a lot of subtext that can be going on in the interview. There is no one right way to resolve this, but you must at least be aware of it.
Feeling questions are questions that ask respondents to draw on their emotional responses. It’s pretty common for academic researchers to forget that we have bodies and emotions, but people’s understandings of the world often operate at this affective level, sometimes unconsciously or barely consciously. It is a good idea to include questions that leave space for respondents to remember, imagine, or relive emotional responses to particular phenomena. “What was it like when you heard your cousin’s house burned down in that wildfire?” doesn’t explicitly use any emotion words, but it allows your respondent to remember what was probably a pretty emotional day. And if they respond emotionally neutral, that is pretty interesting data too. Note that asking someone “How do you feel about X” is not always going to evoke an emotional response, as they might simply turn around and respond with “I think that…” It is better to craft a question that actually pushes the respondent into the affective category. This might be a specific follow-up to an experience and behavior question —for example, “You just told me about your daily routine during the summer heat. Do you worry it is going to get worse?” or “Have you ever been afraid it will be too hot to get your work accomplished?”
Knowledge questions ask respondents what they actually know about something factual. We have to be careful when we ask these types of questions so that respondents do not feel like we are evaluating them (which would shut them down), but, for example, it is helpful to know when you are having a conversation about climate change that your respondent does in fact know that unusual weather events have increased and that these have been attributed to climate change! Asking these questions can set the stage for deeper questions and can ensure that the conversation makes the same kind of sense to both participants. For example, a conversation about political polarization can be put back on track once you realize that the respondent doesn’t really have a clear understanding that there are two parties in the US. Instead of asking a series of questions about Republicans and Democrats, you might shift your questions to talk more generally about political disagreements (e.g., “people against abortion”). And sometimes what you do want to know is the level of knowledge about a particular program or event (e.g., “Are you aware you can discharge your student loans through the Public Service Loan Forgiveness program?”).
Sensory questions call on all senses of the respondent to capture deeper responses. These are particularly helpful in sparking memory. “Think back to your childhood in Eastern Oregon. Describe the smells, the sounds…” Or you could use these questions to help a person access the full experience of a setting they customarily inhabit: “When you walk through the doors to your office building, what do you see? Hear? Smell?” As with feeling questions , these questions often supplement experience and behavior questions . They are another way of allowing your respondent to report fully and deeply rather than remain on the surface.
Creative questions employ illustrative examples, suggested scenarios, or simulations to get respondents to think more deeply about an issue, topic, or experience. There are many options here. In The Trouble with Passion , Erin Cech ( 2021 ) provides a scenario in which “Joe” is trying to decide whether to stay at his decent but boring computer job or follow his passion by opening a restaurant. She asks respondents, “What should Joe do?” Their answers illuminate the attraction of “passion” in job selection. In my own work, I have used a news story about an upwardly mobile young man who no longer has time to see his mother and sisters to probe respondents’ feelings about the costs of social mobility. Jessi Streib and Betsy Leondar-Wright have used single-page cartoon “scenes” to elicit evaluations of potential racial discrimination, sexual harassment, and classism. Barbara Sutton ( 2010 ) has employed lists of words (“strong,” “mother,” “victim”) on notecards she fans out and asks her female respondents to select and discuss.
Background/Demographic Questions
You most definitely will want to know more about the person you are interviewing in terms of conventional demographic information, such as age, race, gender identity, occupation, and educational attainment. These are not questions that normally open up inquiry. [1] For this reason, my practice has been to include a separate “demographic questionnaire” sheet that I ask each respondent to fill out at the conclusion of the interview. Only include those aspects that are relevant to your study. For example, if you are not exploring religion or religious affiliation, do not include questions about a person’s religion on the demographic sheet. See the example provided at the end of this chapter.
Temporality
Any type of question can have a past, present, or future orientation. For example, if you are asking a behavior question about workplace routine, you might ask the respondent to talk about past work, present work, and ideal (future) work. Similarly, if you want to understand how people cope with natural disasters, you might ask your respondent how they felt then during the wildfire and now in retrospect and whether and to what extent they have concerns for future wildfire disasters. It’s a relatively simple suggestion—don’t forget to ask about past, present, and future—but it can have a big impact on the quality of the responses you receive.
Question Sequence
Having a list of good questions or good question areas is not enough to make a good interview guide. You will want to pay attention to the order in which you ask your questions. Even though any one respondent can derail this order (perhaps by jumping to answer a question you haven’t yet asked), a good advance plan is always helpful. When thinking about sequence, remember that your goal is to get your respondent to open up to you and to say things that might surprise you. To establish rapport, it is best to start with nonthreatening questions. Asking about the present is often the safest place to begin, followed by the past (they have to know you a little bit to get there), and lastly, the future (talking about hopes and fears requires the most rapport). To allow for surprises, it is best to move from very general questions to more particular questions only later in the interview. This ensures that respondents have the freedom to bring up the topics that are relevant to them rather than feel like they are constrained to answer you narrowly. For example, refrain from asking about particular emotions until these have come up previously—don’t lead with them. Often, your more particular questions will emerge only during the course of the interview, tailored to what is emerging in conversation.
Once you have a set of questions, read through them aloud and imagine you are being asked the same questions. Does the set of questions have a natural flow? Would you be willing to answer the very first question to a total stranger? Does your sequence establish facts and experiences before moving on to opinions and values? Did you include prefatory statements, where necessary; transitions; and other announcements? These can be as simple as “Hey, we talked a lot about your experiences as a barista while in college.… Now I am turning to something completely different: how you managed friendships in college.” That is an abrupt transition, but it has been softened by your acknowledgment of that.
Probes and Flexibility
Once you have the interview guide, you will also want to leave room for probes and follow-up questions. As in the sample probe included here, you can write out the obvious probes and follow-up questions in advance. You might not need them, as your respondent might anticipate them and include full responses to the original question. Or you might need to tailor them to how your respondent answered the question. Some common probes and follow-up questions include asking for more details (When did that happen? Who else was there?), asking for elaboration (Could you say more about that?), asking for clarification (Does that mean what I think it means or something else? I understand what you mean, but someone else reading the transcript might not), and asking for contrast or comparison (How did this experience compare with last year’s event?). “Probing is a skill that comes from knowing what to look for in the interview, listening carefully to what is being said and what is not said, and being sensitive to the feedback needs of the person being interviewed” ( Patton 2002:374 ). It takes work! And energy. I and many other interviewers I know report feeling emotionally and even physically drained after conducting an interview. You are tasked with active listening and rearranging your interview guide as needed on the fly. If you only ask the questions written down in your interview guide with no deviations, you are doing it wrong. [2]
The Final Question
Every interview guide should include a very open-ended final question that allows for the respondent to say whatever it is they have been dying to tell you but you’ve forgotten to ask. About half the time they are tired too and will tell you they have nothing else to say. But incredibly, some of the most honest and complete responses take place here, at the end of a long interview. You have to realize that the person being interviewed is often discovering things about themselves as they talk to you and that this process of discovery can lead to new insights for them. Making space at the end is therefore crucial. Be sure you convey that you actually do want them to tell you more, that the offer of “anything else?” is not read as an empty convention where the polite response is no. Here is where you can pull from that active listening and tailor the final question to the particular person. For example, “I’ve asked you a lot of questions about what it was like to live through that wildfire. I’m wondering if there is anything I’ve forgotten to ask, especially because I haven’t had that experience myself” is a much more inviting final question than “Great. Anything you want to add?” It’s also helpful to convey to the person that you have the time to listen to their full answer, even if the allotted time is at the end. After all, there are no more questions to ask, so the respondent knows exactly how much time is left. Do them the courtesy of listening to them!
Conducting the Interview
Once you have your interview guide, you are on your way to conducting your first interview. I always practice my interview guide with a friend or family member. I do this even when the questions don’t make perfect sense for them, as it still helps me realize which questions make no sense, are poorly worded (too academic), or don’t follow sequentially. I also practice the routine I will use for interviewing, which goes something like this:
- Introduce myself and reintroduce the study
- Provide consent form and ask them to sign and retain/return copy
- Ask if they have any questions about the study before we begin
- Ask if I can begin recording
- Ask questions (from interview guide)
- Turn off the recording device
- Ask if they are willing to fill out my demographic questionnaire
- Collect questionnaire and, without looking at the answers, place in same folder as signed consent form
- Thank them and depart
A note on remote interviewing: Interviews have traditionally been conducted face-to-face in a private or quiet public setting. You don’t want a lot of background noise, as this will make transcriptions difficult. During the recent global pandemic, many interviewers, myself included, learned the benefits of interviewing remotely. Although face-to-face is still preferable for many reasons, Zoom interviewing is not a bad alternative, and it does allow more interviews across great distances. Zoom also includes automatic transcription, which significantly cuts down on the time it normally takes to convert our conversations into “data” to be analyzed. These automatic transcriptions are not perfect, however, and you will still need to listen to the recording and clarify and clean up the transcription. Nor do automatic transcriptions include notations of body language or change of tone, which you may want to include. When interviewing remotely, you will want to collect the consent form before you meet: ask them to read, sign, and return it as an email attachment. I think it is better to ask for the demographic questionnaire after the interview, but because some respondents may never return it then, it is probably best to ask for this at the same time as the consent form, in advance of the interview.
What should you bring to the interview? I would recommend bringing two copies of the consent form (one for you and one for the respondent), a demographic questionnaire, a manila folder in which to place the signed consent form and filled-out demographic questionnaire, a printed copy of your interview guide (I print with three-inch right margins so I can jot down notes on the page next to relevant questions), a pen, a recording device, and water.
After the interview, you will want to secure the signed consent form in a locked filing cabinet (if in print) or a password-protected folder on your computer. Using Excel or a similar program that allows tables/spreadsheets, create an identifying number for your interview that links to the consent form without using the name of your respondent. For example, let’s say that I conduct interviews with US politicians, and the first person I meet with is George W. Bush. I will assign the transcription the number “INT#001” and add it to the signed consent form. [3] The signed consent form goes into a locked filing cabinet, and I never use the name “George W. Bush” again. I take the information from the demographic sheet, open my Excel spreadsheet, and add the relevant information in separate columns for the row INT#001: White, male, Republican. When I interview Bill Clinton as my second interview, I include a second row: INT#002: White, male, Democrat. And so on. The only link to the actual name of the respondent and this information is the fact that the consent form (unavailable to anyone but me) has stamped on it the interview number.
Many students get very nervous before their first interview. Actually, many of us are always nervous before the interview! But do not worry—this is normal, and it does pass. Chances are, you will be pleasantly surprised at how comfortable it begins to feel. These “purposeful conversations” are often a delight for both participants. This is not to say that sometimes things go wrong. I often have my students practice several “bad scenarios” (e.g., a respondent that you cannot get to open up; a respondent who is too talkative and dominates the conversation, steering it away from the topics you are interested in; emotions that completely take over; or shocking disclosures you are ill-prepared to handle), but most of the time, things go quite well. Be prepared for the unexpected, but know that the reason interviews are so popular as a technique of data collection is that they are usually richly rewarding for both participants.
One thing that I stress to my methods students and remind myself about is that interviews are still conversations between people. If there’s something you might feel uncomfortable asking someone about in a “normal” conversation, you will likely also feel a bit of discomfort asking it in an interview. Maybe more importantly, your respondent may feel uncomfortable. Social research—especially about inequality—can be uncomfortable. And it’s easy to slip into an abstract, intellectualized, or removed perspective as an interviewer. This is one reason trying out interview questions is important. Another is that sometimes the question sounds good in your head but doesn’t work as well out loud in practice. I learned this the hard way when a respondent asked me how I would answer the question I had just posed, and I realized that not only did I not really know how I would answer it, but I also wasn’t quite as sure I knew what I was asking as I had thought.
—Elizabeth M. Lee, Associate Professor of Sociology at Saint Joseph’s University, author of Class and Campus Life , and co-author of Geographies of Campus Inequality
How Many Interviews?
Your research design has included a targeted number of interviews and a recruitment plan (see chapter 5). Follow your plan, but remember that “ saturation ” is your goal. You interview as many people as you can until you reach a point at which you are no longer surprised by what they tell you. This means not that no one after your first twenty interviews will have surprising, interesting stories to tell you but rather that the picture you are forming about the phenomenon of interest to you from a research perspective has come into focus, and none of the interviews are substantially refocusing that picture. That is when you should stop collecting interviews. Note that to know when you have reached this, you will need to read your transcripts as you go. More about this in chapters 18 and 19.
Your Final Product: The Ideal Interview Transcript
A good interview transcript will demonstrate a subtly controlled conversation by the skillful interviewer. In general, you want to see replies that are about one paragraph long, not short sentences and not running on for several pages. Although it is sometimes necessary to follow respondents down tangents, it is also often necessary to pull them back to the questions that form the basis of your research study. This is not really a free conversation, although it may feel like that to the person you are interviewing.
Final Tips from an Interview Master
Annette Lareau is arguably one of the masters of the trade. In Listening to People , she provides several guidelines for good interviews and then offers a detailed example of an interview gone wrong and how it could be addressed (please see the “Further Readings” at the end of this chapter). Here is an abbreviated version of her set of guidelines: (1) interview respondents who are experts on the subjects of most interest to you (as a corollary, don’t ask people about things they don’t know); (2) listen carefully and talk as little as possible; (3) keep in mind what you want to know and why you want to know it; (4) be a proactive interviewer (subtly guide the conversation); (5) assure respondents that there aren’t any right or wrong answers; (6) use the respondent’s own words to probe further (this both allows you to accurately identify what you heard and pushes the respondent to explain further); (7) reuse effective probes (don’t reinvent the wheel as you go—if repeating the words back works, do it again and again); (8) focus on learning the subjective meanings that events or experiences have for a respondent; (9) don’t be afraid to ask a question that draws on your own knowledge (unlike trial lawyers who are trained never to ask a question for which they don’t already know the answer, sometimes it’s worth it to ask risky questions based on your hypotheses or just plain hunches); (10) keep thinking while you are listening (so difficult…and important); (11) return to a theme raised by a respondent if you want further information; (12) be mindful of power inequalities (and never ever coerce a respondent to continue the interview if they want out); (13) take control with overly talkative respondents; (14) expect overly succinct responses, and develop strategies for probing further; (15) balance digging deep and moving on; (16) develop a plan to deflect questions (e.g., let them know you are happy to answer any questions at the end of the interview, but you don’t want to take time away from them now); and at the end, (17) check to see whether you have asked all your questions. You don’t always have to ask everyone the same set of questions, but if there is a big area you have forgotten to cover, now is the time to recover ( Lareau 2021:93–103 ).
Sample: Demographic Questionnaire
ASA Taskforce on First-Generation and Working-Class Persons in Sociology – Class Effects on Career Success
Supplementary Demographic Questionnaire
Thank you for your participation in this interview project. We would like to collect a few pieces of key demographic information from you to supplement our analyses. Your answers to these questions will be kept confidential and stored by ID number. All of your responses here are entirely voluntary!
What best captures your race/ethnicity? (please check any/all that apply)
- White (Non Hispanic/Latina/o/x)
- Black or African American
- Hispanic, Latino/a/x of Spanish
- Asian or Asian American
- American Indian or Alaska Native
- Middle Eastern or North African
- Native Hawaiian or Pacific Islander
- Other : (Please write in: ________________)
What is your current position?
- Grad Student
- Full Professor
Please check any and all of the following that apply to you:
- I identify as a working-class academic
- I was the first in my family to graduate from college
- I grew up poor
What best reflects your gender?
- Transgender female/Transgender woman
- Transgender male/Transgender man
- Gender queer/ Gender nonconforming
Anything else you would like us to know about you?
Example: Interview Guide
In this example, follow-up prompts are italicized. Note the sequence of questions. That second question often elicits an entire life history , answering several later questions in advance.
Introduction Script/Question
Thank you for participating in our survey of ASA members who identify as first-generation or working-class. As you may have heard, ASA has sponsored a taskforce on first-generation and working-class persons in sociology and we are interested in hearing from those who so identify. Your participation in this interview will help advance our knowledge in this area.
- The first thing we would like to as you is why you have volunteered to be part of this study? What does it mean to you be first-gen or working class? Why were you willing to be interviewed?
- How did you decide to become a sociologist?
- Can you tell me a little bit about where you grew up? ( prompts: what did your parent(s) do for a living? What kind of high school did you attend?)
- Has this identity been salient to your experience? (how? How much?)
- How welcoming was your grad program? Your first academic employer?
- Why did you decide to pursue sociology at the graduate level?
- Did you experience culture shock in college? In graduate school?
- Has your FGWC status shaped how you’ve thought about where you went to school? debt? etc?
- Were you mentored? How did this work (not work)? How might it?
- What did you consider when deciding where to go to grad school? Where to apply for your first position?
- What, to you, is a mark of career success? Have you achieved that success? What has helped or hindered your pursuit of success?
- Do you think sociology, as a field, cares about prestige?
- Let’s talk a little bit about intersectionality. How does being first-gen/working class work alongside other identities that are important to you?
- What do your friends and family think about your career? Have you had any difficulty relating to family members or past friends since becoming highly educated?
- Do you have any debt from college/grad school? Are you concerned about this? Could you explain more about how you paid for college/grad school? (here, include assistance from family, fellowships, scholarships, etc.)
- (You’ve mentioned issues or obstacles you had because of your background.) What could have helped? Or, who or what did? Can you think of fortuitous moments in your career?
- Do you have any regrets about the path you took?
- Is there anything else you would like to add? Anything that the Taskforce should take note of, that we did not ask you about here?
Further Readings
Britten, Nicky. 1995. “Qualitative Interviews in Medical Research.” BMJ: British Medical Journal 31(6999):251–253. A good basic overview of interviewing particularly useful for students of public health and medical research generally.
Corbin, Juliet, and Janice M. Morse. 2003. “The Unstructured Interactive Interview: Issues of Reciprocity and Risks When Dealing with Sensitive Topics.” Qualitative Inquiry 9(3):335–354. Weighs the potential benefits and harms of conducting interviews on topics that may cause emotional distress. Argues that the researcher’s skills and code of ethics should ensure that the interviewing process provides more of a benefit to both participant and researcher than a harm to the former.
Gerson, Kathleen, and Sarah Damaske. 2020. The Science and Art of Interviewing . New York: Oxford University Press. A useful guidebook/textbook for both undergraduates and graduate students, written by sociologists.
Kvale, Steiner. 2007. Doing Interviews . London: SAGE. An easy-to-follow guide to conducting and analyzing interviews by psychologists.
Lamont, Michèle, and Ann Swidler. 2014. “Methodological Pluralism and the Possibilities and Limits of Interviewing.” Qualitative Sociology 37(2):153–171. Written as a response to various debates surrounding the relative value of interview-based studies and ethnographic studies defending the particular strengths of interviewing. This is a must-read article for anyone seriously engaging in qualitative research!
Pugh, Allison J. 2013. “What Good Are Interviews for Thinking about Culture? Demystifying Interpretive Analysis.” American Journal of Cultural Sociology 1(1):42–68. Another defense of interviewing written against those who champion ethnographic methods as superior, particularly in the area of studying culture. A classic.
Rapley, Timothy John. 2001. “The ‘Artfulness’ of Open-Ended Interviewing: Some considerations in analyzing interviews.” Qualitative Research 1(3):303–323. Argues for the importance of “local context” of data production (the relationship built between interviewer and interviewee, for example) in properly analyzing interview data.
Weiss, Robert S. 1995. Learning from Strangers: The Art and Method of Qualitative Interview Studies . New York: Simon and Schuster. A classic and well-regarded textbook on interviewing. Because Weiss has extensive experience conducting surveys, he contrasts the qualitative interview with the survey questionnaire well; particularly useful for those trained in the latter.
- I say “normally” because how people understand their various identities can itself be an expansive topic of inquiry. Here, I am merely talking about collecting otherwise unexamined demographic data, similar to how we ask people to check boxes on surveys. ↵
- Again, this applies to “semistructured in-depth interviewing.” When conducting standardized questionnaires, you will want to ask each question exactly as written, without deviations! ↵
- I always include “INT” in the number because I sometimes have other kinds of data with their own numbering: FG#001 would mean the first focus group, for example. I also always include three-digit spaces, as this allows for up to 999 interviews (or, more realistically, allows for me to interview up to one hundred persons without having to reset my numbering system). ↵
A method of data collection in which the researcher asks the participant questions; the answers to these questions are often recorded and transcribed verbatim. There are many different kinds of interviews - see also semistructured interview , structured interview , and unstructured interview .
A document listing key questions and question areas for use during an interview. It is used most often for semi-structured interviews. A good interview guide may have no more than ten primary questions for two hours of interviewing, but these ten questions will be supplemented by probes and relevant follow-ups throughout the interview. Most IRBs require the inclusion of the interview guide in applications for review. See also interview and semi-structured interview .
A data-collection method that relies on casual, conversational, and informal interviewing. Despite its apparent conversational nature, the researcher usually has a set of particular questions or question areas in mind but allows the interview to unfold spontaneously. This is a common data-collection technique among ethnographers. Compare to the semi-structured or in-depth interview .
A form of interview that follows a standard guide of questions asked, although the order of the questions may change to match the particular needs of each individual interview subject, and probing “follow-up” questions are often added during the course of the interview. The semi-structured interview is the primary form of interviewing used by qualitative researchers in the social sciences. It is sometimes referred to as an “in-depth” interview. See also interview and interview guide .
The cluster of data-collection tools and techniques that involve observing interactions between people, the behaviors, and practices of individuals (sometimes in contrast to what they say about how they act and behave), and cultures in context. Observational methods are the key tools employed by ethnographers and Grounded Theory .
Follow-up questions used in a semi-structured interview to elicit further elaboration. Suggested prompts can be included in the interview guide to be used/deployed depending on how the initial question was answered or if the topic of the prompt does not emerge spontaneously.
A form of interview that follows a strict set of questions, asked in a particular order, for all interview subjects. The questions are also the kind that elicits short answers, and the data is more “informative” than probing. This is often used in mixed-methods studies, accompanying a survey instrument. Because there is no room for nuance or the exploration of meaning in structured interviews, qualitative researchers tend to employ semi-structured interviews instead. See also interview.
The point at which you can conclude data collection because every person you are interviewing, the interaction you are observing, or content you are analyzing merely confirms what you have already noted. Achieving saturation is often used as the justification for the final sample size.
An interview variant in which a person’s life story is elicited in a narrative form. Turning points and key themes are established by the researcher and used as data points for further analysis.
Introduction to Qualitative Research Methods Copyright © 2023 by Allison Hurst is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License , except where otherwise noted.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Neurol Res Pract

How to use and assess qualitative research methods
Loraine busetto.
1 Department of Neurology, Heidelberg University Hospital, Im Neuenheimer Feld 400, 69120 Heidelberg, Germany
Wolfgang Wick
2 Clinical Cooperation Unit Neuro-Oncology, German Cancer Research Center, Heidelberg, Germany
Christoph Gumbinger
Associated data.
Not applicable.
This paper aims to provide an overview of the use and assessment of qualitative research methods in the health sciences. Qualitative research can be defined as the study of the nature of phenomena and is especially appropriate for answering questions of why something is (not) observed, assessing complex multi-component interventions, and focussing on intervention improvement. The most common methods of data collection are document study, (non-) participant observations, semi-structured interviews and focus groups. For data analysis, field-notes and audio-recordings are transcribed into protocols and transcripts, and coded using qualitative data management software. Criteria such as checklists, reflexivity, sampling strategies, piloting, co-coding, member-checking and stakeholder involvement can be used to enhance and assess the quality of the research conducted. Using qualitative in addition to quantitative designs will equip us with better tools to address a greater range of research problems, and to fill in blind spots in current neurological research and practice.
The aim of this paper is to provide an overview of qualitative research methods, including hands-on information on how they can be used, reported and assessed. This article is intended for beginning qualitative researchers in the health sciences as well as experienced quantitative researchers who wish to broaden their understanding of qualitative research.
What is qualitative research?
Qualitative research is defined as “the study of the nature of phenomena”, including “their quality, different manifestations, the context in which they appear or the perspectives from which they can be perceived” , but excluding “their range, frequency and place in an objectively determined chain of cause and effect” [ 1 ]. This formal definition can be complemented with a more pragmatic rule of thumb: qualitative research generally includes data in form of words rather than numbers [ 2 ].
Why conduct qualitative research?
Because some research questions cannot be answered using (only) quantitative methods. For example, one Australian study addressed the issue of why patients from Aboriginal communities often present late or not at all to specialist services offered by tertiary care hospitals. Using qualitative interviews with patients and staff, it found one of the most significant access barriers to be transportation problems, including some towns and communities simply not having a bus service to the hospital [ 3 ]. A quantitative study could have measured the number of patients over time or even looked at possible explanatory factors – but only those previously known or suspected to be of relevance. To discover reasons for observed patterns, especially the invisible or surprising ones, qualitative designs are needed.
While qualitative research is common in other fields, it is still relatively underrepresented in health services research. The latter field is more traditionally rooted in the evidence-based-medicine paradigm, as seen in " research that involves testing the effectiveness of various strategies to achieve changes in clinical practice, preferably applying randomised controlled trial study designs (...) " [ 4 ]. This focus on quantitative research and specifically randomised controlled trials (RCT) is visible in the idea of a hierarchy of research evidence which assumes that some research designs are objectively better than others, and that choosing a "lesser" design is only acceptable when the better ones are not practically or ethically feasible [ 5 , 6 ]. Others, however, argue that an objective hierarchy does not exist, and that, instead, the research design and methods should be chosen to fit the specific research question at hand – "questions before methods" [ 2 , 7 – 9 ]. This means that even when an RCT is possible, some research problems require a different design that is better suited to addressing them. Arguing in JAMA, Berwick uses the example of rapid response teams in hospitals, which he describes as " a complex, multicomponent intervention – essentially a process of social change" susceptible to a range of different context factors including leadership or organisation history. According to him, "[in] such complex terrain, the RCT is an impoverished way to learn. Critics who use it as a truth standard in this context are incorrect" [ 8 ] . Instead of limiting oneself to RCTs, Berwick recommends embracing a wider range of methods , including qualitative ones, which for "these specific applications, (...) are not compromises in learning how to improve; they are superior" [ 8 ].
Research problems that can be approached particularly well using qualitative methods include assessing complex multi-component interventions or systems (of change), addressing questions beyond “what works”, towards “what works for whom when, how and why”, and focussing on intervention improvement rather than accreditation [ 7 , 9 – 12 ]. Using qualitative methods can also help shed light on the “softer” side of medical treatment. For example, while quantitative trials can measure the costs and benefits of neuro-oncological treatment in terms of survival rates or adverse effects, qualitative research can help provide a better understanding of patient or caregiver stress, visibility of illness or out-of-pocket expenses.
How to conduct qualitative research?
Given that qualitative research is characterised by flexibility, openness and responsivity to context, the steps of data collection and analysis are not as separate and consecutive as they tend to be in quantitative research [ 13 , 14 ]. As Fossey puts it : “sampling, data collection, analysis and interpretation are related to each other in a cyclical (iterative) manner, rather than following one after another in a stepwise approach” [ 15 ]. The researcher can make educated decisions with regard to the choice of method, how they are implemented, and to which and how many units they are applied [ 13 ]. As shown in Fig. 1 , this can involve several back-and-forth steps between data collection and analysis where new insights and experiences can lead to adaption and expansion of the original plan. Some insights may also necessitate a revision of the research question and/or the research design as a whole. The process ends when saturation is achieved, i.e. when no relevant new information can be found (see also below: sampling and saturation). For reasons of transparency, it is essential for all decisions as well as the underlying reasoning to be well-documented.

Iterative research process
While it is not always explicitly addressed, qualitative methods reflect a different underlying research paradigm than quantitative research (e.g. constructivism or interpretivism as opposed to positivism). The choice of methods can be based on the respective underlying substantive theory or theoretical framework used by the researcher [ 2 ].
Data collection
The methods of qualitative data collection most commonly used in health research are document study, observations, semi-structured interviews and focus groups [ 1 , 14 , 16 , 17 ].
Document study
Document study (also called document analysis) refers to the review by the researcher of written materials [ 14 ]. These can include personal and non-personal documents such as archives, annual reports, guidelines, policy documents, diaries or letters.
Observations
Observations are particularly useful to gain insights into a certain setting and actual behaviour – as opposed to reported behaviour or opinions [ 13 ]. Qualitative observations can be either participant or non-participant in nature. In participant observations, the observer is part of the observed setting, for example a nurse working in an intensive care unit [ 18 ]. In non-participant observations, the observer is “on the outside looking in”, i.e. present in but not part of the situation, trying not to influence the setting by their presence. Observations can be planned (e.g. for 3 h during the day or night shift) or ad hoc (e.g. as soon as a stroke patient arrives at the emergency room). During the observation, the observer takes notes on everything or certain pre-determined parts of what is happening around them, for example focusing on physician-patient interactions or communication between different professional groups. Written notes can be taken during or after the observations, depending on feasibility (which is usually lower during participant observations) and acceptability (e.g. when the observer is perceived to be judging the observed). Afterwards, these field notes are transcribed into observation protocols. If more than one observer was involved, field notes are taken independently, but notes can be consolidated into one protocol after discussions. Advantages of conducting observations include minimising the distance between the researcher and the researched, the potential discovery of topics that the researcher did not realise were relevant and gaining deeper insights into the real-world dimensions of the research problem at hand [ 18 ].
Semi-structured interviews
Hijmans & Kuyper describe qualitative interviews as “an exchange with an informal character, a conversation with a goal” [ 19 ]. Interviews are used to gain insights into a person’s subjective experiences, opinions and motivations – as opposed to facts or behaviours [ 13 ]. Interviews can be distinguished by the degree to which they are structured (i.e. a questionnaire), open (e.g. free conversation or autobiographical interviews) or semi-structured [ 2 , 13 ]. Semi-structured interviews are characterized by open-ended questions and the use of an interview guide (or topic guide/list) in which the broad areas of interest, sometimes including sub-questions, are defined [ 19 ]. The pre-defined topics in the interview guide can be derived from the literature, previous research or a preliminary method of data collection, e.g. document study or observations. The topic list is usually adapted and improved at the start of the data collection process as the interviewer learns more about the field [ 20 ]. Across interviews the focus on the different (blocks of) questions may differ and some questions may be skipped altogether (e.g. if the interviewee is not able or willing to answer the questions or for concerns about the total length of the interview) [ 20 ]. Qualitative interviews are usually not conducted in written format as it impedes on the interactive component of the method [ 20 ]. In comparison to written surveys, qualitative interviews have the advantage of being interactive and allowing for unexpected topics to emerge and to be taken up by the researcher. This can also help overcome a provider or researcher-centred bias often found in written surveys, which by nature, can only measure what is already known or expected to be of relevance to the researcher. Interviews can be audio- or video-taped; but sometimes it is only feasible or acceptable for the interviewer to take written notes [ 14 , 16 , 20 ].
Focus groups
Focus groups are group interviews to explore participants’ expertise and experiences, including explorations of how and why people behave in certain ways [ 1 ]. Focus groups usually consist of 6–8 people and are led by an experienced moderator following a topic guide or “script” [ 21 ]. They can involve an observer who takes note of the non-verbal aspects of the situation, possibly using an observation guide [ 21 ]. Depending on researchers’ and participants’ preferences, the discussions can be audio- or video-taped and transcribed afterwards [ 21 ]. Focus groups are useful for bringing together homogeneous (to a lesser extent heterogeneous) groups of participants with relevant expertise and experience on a given topic on which they can share detailed information [ 21 ]. Focus groups are a relatively easy, fast and inexpensive method to gain access to information on interactions in a given group, i.e. “the sharing and comparing” among participants [ 21 ]. Disadvantages include less control over the process and a lesser extent to which each individual may participate. Moreover, focus group moderators need experience, as do those tasked with the analysis of the resulting data. Focus groups can be less appropriate for discussing sensitive topics that participants might be reluctant to disclose in a group setting [ 13 ]. Moreover, attention must be paid to the emergence of “groupthink” as well as possible power dynamics within the group, e.g. when patients are awed or intimidated by health professionals.
Choosing the “right” method
As explained above, the school of thought underlying qualitative research assumes no objective hierarchy of evidence and methods. This means that each choice of single or combined methods has to be based on the research question that needs to be answered and a critical assessment with regard to whether or to what extent the chosen method can accomplish this – i.e. the “fit” between question and method [ 14 ]. It is necessary for these decisions to be documented when they are being made, and to be critically discussed when reporting methods and results.
Let us assume that our research aim is to examine the (clinical) processes around acute endovascular treatment (EVT), from the patient’s arrival at the emergency room to recanalization, with the aim to identify possible causes for delay and/or other causes for sub-optimal treatment outcome. As a first step, we could conduct a document study of the relevant standard operating procedures (SOPs) for this phase of care – are they up-to-date and in line with current guidelines? Do they contain any mistakes, irregularities or uncertainties that could cause delays or other problems? Regardless of the answers to these questions, the results have to be interpreted based on what they are: a written outline of what care processes in this hospital should look like. If we want to know what they actually look like in practice, we can conduct observations of the processes described in the SOPs. These results can (and should) be analysed in themselves, but also in comparison to the results of the document analysis, especially as regards relevant discrepancies. Do the SOPs outline specific tests for which no equipment can be observed or tasks to be performed by specialized nurses who are not present during the observation? It might also be possible that the written SOP is outdated, but the actual care provided is in line with current best practice. In order to find out why these discrepancies exist, it can be useful to conduct interviews. Are the physicians simply not aware of the SOPs (because their existence is limited to the hospital’s intranet) or do they actively disagree with them or does the infrastructure make it impossible to provide the care as described? Another rationale for adding interviews is that some situations (or all of their possible variations for different patient groups or the day, night or weekend shift) cannot practically or ethically be observed. In this case, it is possible to ask those involved to report on their actions – being aware that this is not the same as the actual observation. A senior physician’s or hospital manager’s description of certain situations might differ from a nurse’s or junior physician’s one, maybe because they intentionally misrepresent facts or maybe because different aspects of the process are visible or important to them. In some cases, it can also be relevant to consider to whom the interviewee is disclosing this information – someone they trust, someone they are otherwise not connected to, or someone they suspect or are aware of being in a potentially “dangerous” power relationship to them. Lastly, a focus group could be conducted with representatives of the relevant professional groups to explore how and why exactly they provide care around EVT. The discussion might reveal discrepancies (between SOPs and actual care or between different physicians) and motivations to the researchers as well as to the focus group members that they might not have been aware of themselves. For the focus group to deliver relevant information, attention has to be paid to its composition and conduct, for example, to make sure that all participants feel safe to disclose sensitive or potentially problematic information or that the discussion is not dominated by (senior) physicians only. The resulting combination of data collection methods is shown in Fig. 2 .

Possible combination of data collection methods
Attributions for icons: “Book” by Serhii Smirnov, “Interview” by Adrien Coquet, FR, “Magnifying Glass” by anggun, ID, “Business communication” by Vectors Market; all from the Noun Project
The combination of multiple data source as described for this example can be referred to as “triangulation”, in which multiple measurements are carried out from different angles to achieve a more comprehensive understanding of the phenomenon under study [ 22 , 23 ].
Data analysis
To analyse the data collected through observations, interviews and focus groups these need to be transcribed into protocols and transcripts (see Fig. 3 ). Interviews and focus groups can be transcribed verbatim , with or without annotations for behaviour (e.g. laughing, crying, pausing) and with or without phonetic transcription of dialects and filler words, depending on what is expected or known to be relevant for the analysis. In the next step, the protocols and transcripts are coded , that is, marked (or tagged, labelled) with one or more short descriptors of the content of a sentence or paragraph [ 2 , 15 , 23 ]. Jansen describes coding as “connecting the raw data with “theoretical” terms” [ 20 ]. In a more practical sense, coding makes raw data sortable. This makes it possible to extract and examine all segments describing, say, a tele-neurology consultation from multiple data sources (e.g. SOPs, emergency room observations, staff and patient interview). In a process of synthesis and abstraction, the codes are then grouped, summarised and/or categorised [ 15 , 20 ]. The end product of the coding or analysis process is a descriptive theory of the behavioural pattern under investigation [ 20 ]. The coding process is performed using qualitative data management software, the most common ones being InVivo, MaxQDA and Atlas.ti. It should be noted that these are data management tools which support the analysis performed by the researcher(s) [ 14 ].

From data collection to data analysis
Attributions for icons: see Fig. Fig.2, 2 , also “Speech to text” by Trevor Dsouza, “Field Notes” by Mike O’Brien, US, “Voice Record” by ProSymbols, US, “Inspection” by Made, AU, and “Cloud” by Graphic Tigers; all from the Noun Project
How to report qualitative research?
Protocols of qualitative research can be published separately and in advance of the study results. However, the aim is not the same as in RCT protocols, i.e. to pre-define and set in stone the research questions and primary or secondary endpoints. Rather, it is a way to describe the research methods in detail, which might not be possible in the results paper given journals’ word limits. Qualitative research papers are usually longer than their quantitative counterparts to allow for deep understanding and so-called “thick description”. In the methods section, the focus is on transparency of the methods used, including why, how and by whom they were implemented in the specific study setting, so as to enable a discussion of whether and how this may have influenced data collection, analysis and interpretation. The results section usually starts with a paragraph outlining the main findings, followed by more detailed descriptions of, for example, the commonalities, discrepancies or exceptions per category [ 20 ]. Here it is important to support main findings by relevant quotations, which may add information, context, emphasis or real-life examples [ 20 , 23 ]. It is subject to debate in the field whether it is relevant to state the exact number or percentage of respondents supporting a certain statement (e.g. “Five interviewees expressed negative feelings towards XYZ”) [ 21 ].
How to combine qualitative with quantitative research?
Qualitative methods can be combined with other methods in multi- or mixed methods designs, which “[employ] two or more different methods [ …] within the same study or research program rather than confining the research to one single method” [ 24 ]. Reasons for combining methods can be diverse, including triangulation for corroboration of findings, complementarity for illustration and clarification of results, expansion to extend the breadth and range of the study, explanation of (unexpected) results generated with one method with the help of another, or offsetting the weakness of one method with the strength of another [ 1 , 17 , 24 – 26 ]. The resulting designs can be classified according to when, why and how the different quantitative and/or qualitative data strands are combined. The three most common types of mixed method designs are the convergent parallel design , the explanatory sequential design and the exploratory sequential design. The designs with examples are shown in Fig. 4 .

Three common mixed methods designs
In the convergent parallel design, a qualitative study is conducted in parallel to and independently of a quantitative study, and the results of both studies are compared and combined at the stage of interpretation of results. Using the above example of EVT provision, this could entail setting up a quantitative EVT registry to measure process times and patient outcomes in parallel to conducting the qualitative research outlined above, and then comparing results. Amongst other things, this would make it possible to assess whether interview respondents’ subjective impressions of patients receiving good care match modified Rankin Scores at follow-up, or whether observed delays in care provision are exceptions or the rule when compared to door-to-needle times as documented in the registry. In the explanatory sequential design, a quantitative study is carried out first, followed by a qualitative study to help explain the results from the quantitative study. This would be an appropriate design if the registry alone had revealed relevant delays in door-to-needle times and the qualitative study would be used to understand where and why these occurred, and how they could be improved. In the exploratory design, the qualitative study is carried out first and its results help informing and building the quantitative study in the next step [ 26 ]. If the qualitative study around EVT provision had shown a high level of dissatisfaction among the staff members involved, a quantitative questionnaire investigating staff satisfaction could be set up in the next step, informed by the qualitative study on which topics dissatisfaction had been expressed. Amongst other things, the questionnaire design would make it possible to widen the reach of the research to more respondents from different (types of) hospitals, regions, countries or settings, and to conduct sub-group analyses for different professional groups.
How to assess qualitative research?
A variety of assessment criteria and lists have been developed for qualitative research, ranging in their focus and comprehensiveness [ 14 , 17 , 27 ]. However, none of these has been elevated to the “gold standard” in the field. In the following, we therefore focus on a set of commonly used assessment criteria that, from a practical standpoint, a researcher can look for when assessing a qualitative research report or paper.
Assessors should check the authors’ use of and adherence to the relevant reporting checklists (e.g. Standards for Reporting Qualitative Research (SRQR)) to make sure all items that are relevant for this type of research are addressed [ 23 , 28 ]. Discussions of quantitative measures in addition to or instead of these qualitative measures can be a sign of lower quality of the research (paper). Providing and adhering to a checklist for qualitative research contributes to an important quality criterion for qualitative research, namely transparency [ 15 , 17 , 23 ].
Reflexivity
While methodological transparency and complete reporting is relevant for all types of research, some additional criteria must be taken into account for qualitative research. This includes what is called reflexivity, i.e. sensitivity to the relationship between the researcher and the researched, including how contact was established and maintained, or the background and experience of the researcher(s) involved in data collection and analysis. Depending on the research question and population to be researched this can be limited to professional experience, but it may also include gender, age or ethnicity [ 17 , 27 ]. These details are relevant because in qualitative research, as opposed to quantitative research, the researcher as a person cannot be isolated from the research process [ 23 ]. It may influence the conversation when an interviewed patient speaks to an interviewer who is a physician, or when an interviewee is asked to discuss a gynaecological procedure with a male interviewer, and therefore the reader must be made aware of these details [ 19 ].
Sampling and saturation
The aim of qualitative sampling is for all variants of the objects of observation that are deemed relevant for the study to be present in the sample “ to see the issue and its meanings from as many angles as possible” [ 1 , 16 , 19 , 20 , 27 ] , and to ensure “information-richness [ 15 ]. An iterative sampling approach is advised, in which data collection (e.g. five interviews) is followed by data analysis, followed by more data collection to find variants that are lacking in the current sample. This process continues until no new (relevant) information can be found and further sampling becomes redundant – which is called saturation [ 1 , 15 ] . In other words: qualitative data collection finds its end point not a priori , but when the research team determines that saturation has been reached [ 29 , 30 ].
This is also the reason why most qualitative studies use deliberate instead of random sampling strategies. This is generally referred to as “ purposive sampling” , in which researchers pre-define which types of participants or cases they need to include so as to cover all variations that are expected to be of relevance, based on the literature, previous experience or theory (i.e. theoretical sampling) [ 14 , 20 ]. Other types of purposive sampling include (but are not limited to) maximum variation sampling, critical case sampling or extreme or deviant case sampling [ 2 ]. In the above EVT example, a purposive sample could include all relevant professional groups and/or all relevant stakeholders (patients, relatives) and/or all relevant times of observation (day, night and weekend shift).
Assessors of qualitative research should check whether the considerations underlying the sampling strategy were sound and whether or how researchers tried to adapt and improve their strategies in stepwise or cyclical approaches between data collection and analysis to achieve saturation [ 14 ].
Good qualitative research is iterative in nature, i.e. it goes back and forth between data collection and analysis, revising and improving the approach where necessary. One example of this are pilot interviews, where different aspects of the interview (especially the interview guide, but also, for example, the site of the interview or whether the interview can be audio-recorded) are tested with a small number of respondents, evaluated and revised [ 19 ]. In doing so, the interviewer learns which wording or types of questions work best, or which is the best length of an interview with patients who have trouble concentrating for an extended time. Of course, the same reasoning applies to observations or focus groups which can also be piloted.
Ideally, coding should be performed by at least two researchers, especially at the beginning of the coding process when a common approach must be defined, including the establishment of a useful coding list (or tree), and when a common meaning of individual codes must be established [ 23 ]. An initial sub-set or all transcripts can be coded independently by the coders and then compared and consolidated after regular discussions in the research team. This is to make sure that codes are applied consistently to the research data.
Member checking
Member checking, also called respondent validation , refers to the practice of checking back with study respondents to see if the research is in line with their views [ 14 , 27 ]. This can happen after data collection or analysis or when first results are available [ 23 ]. For example, interviewees can be provided with (summaries of) their transcripts and asked whether they believe this to be a complete representation of their views or whether they would like to clarify or elaborate on their responses [ 17 ]. Respondents’ feedback on these issues then becomes part of the data collection and analysis [ 27 ].
Stakeholder involvement
In those niches where qualitative approaches have been able to evolve and grow, a new trend has seen the inclusion of patients and their representatives not only as study participants (i.e. “members”, see above) but as consultants to and active participants in the broader research process [ 31 – 33 ]. The underlying assumption is that patients and other stakeholders hold unique perspectives and experiences that add value beyond their own single story, making the research more relevant and beneficial to researchers, study participants and (future) patients alike [ 34 , 35 ]. Using the example of patients on or nearing dialysis, a recent scoping review found that 80% of clinical research did not address the top 10 research priorities identified by patients and caregivers [ 32 , 36 ]. In this sense, the involvement of the relevant stakeholders, especially patients and relatives, is increasingly being seen as a quality indicator in and of itself.
How not to assess qualitative research
The above overview does not include certain items that are routine in assessments of quantitative research. What follows is a non-exhaustive, non-representative, experience-based list of the quantitative criteria often applied to the assessment of qualitative research, as well as an explanation of the limited usefulness of these endeavours.
Protocol adherence
Given the openness and flexibility of qualitative research, it should not be assessed by how well it adheres to pre-determined and fixed strategies – in other words: its rigidity. Instead, the assessor should look for signs of adaptation and refinement based on lessons learned from earlier steps in the research process.
Sample size
For the reasons explained above, qualitative research does not require specific sample sizes, nor does it require that the sample size be determined a priori [ 1 , 14 , 27 , 37 – 39 ]. Sample size can only be a useful quality indicator when related to the research purpose, the chosen methodology and the composition of the sample, i.e. who was included and why.
Randomisation
While some authors argue that randomisation can be used in qualitative research, this is not commonly the case, as neither its feasibility nor its necessity or usefulness has been convincingly established for qualitative research [ 13 , 27 ]. Relevant disadvantages include the negative impact of a too large sample size as well as the possibility (or probability) of selecting “ quiet, uncooperative or inarticulate individuals ” [ 17 ]. Qualitative studies do not use control groups, either.
Interrater reliability, variability and other “objectivity checks”
The concept of “interrater reliability” is sometimes used in qualitative research to assess to which extent the coding approach overlaps between the two co-coders. However, it is not clear what this measure tells us about the quality of the analysis [ 23 ]. This means that these scores can be included in qualitative research reports, preferably with some additional information on what the score means for the analysis, but it is not a requirement. Relatedly, it is not relevant for the quality or “objectivity” of qualitative research to separate those who recruited the study participants and collected and analysed the data. Experiences even show that it might be better to have the same person or team perform all of these tasks [ 20 ]. First, when researchers introduce themselves during recruitment this can enhance trust when the interview takes place days or weeks later with the same researcher. Second, when the audio-recording is transcribed for analysis, the researcher conducting the interviews will usually remember the interviewee and the specific interview situation during data analysis. This might be helpful in providing additional context information for interpretation of data, e.g. on whether something might have been meant as a joke [ 18 ].
Not being quantitative research
Being qualitative research instead of quantitative research should not be used as an assessment criterion if it is used irrespectively of the research problem at hand. Similarly, qualitative research should not be required to be combined with quantitative research per se – unless mixed methods research is judged as inherently better than single-method research. In this case, the same criterion should be applied for quantitative studies without a qualitative component.
The main take-away points of this paper are summarised in Table Table1. 1 . We aimed to show that, if conducted well, qualitative research can answer specific research questions that cannot to be adequately answered using (only) quantitative designs. Seeing qualitative and quantitative methods as equal will help us become more aware and critical of the “fit” between the research problem and our chosen methods: I can conduct an RCT to determine the reasons for transportation delays of acute stroke patients – but should I? It also provides us with a greater range of tools to tackle a greater range of research problems more appropriately and successfully, filling in the blind spots on one half of the methodological spectrum to better address the whole complexity of neurological research and practice.
Take-away-points
• Assessing complex multi-component interventions or systems (of change) • What works for whom when, how and why? • Focussing on intervention improvement | • Document study • Observations (participant or non-participant) • Interviews (especially semi-structured) • Focus groups | • Transcription of audio-recordings and field notes into transcripts and protocols • Coding of protocols • Using qualitative data management software |
• Combinations of quantitative and/or qualitative methods, e.g.: • : quali and quanti in parallel • : quanti followed by quali • : quali followed by quanti | • Checklists • Reflexivity • Sampling strategies • Piloting • Co-coding • Member checking • Stakeholder involvement | • Protocol adherence • Sample size • Randomization • Interrater reliability, variability and other “objectivity checks” • Not being quantitative research |
Acknowledgements
Abbreviations.
| EVT | Endovascular treatment |
| RCT | Randomised Controlled Trial |
| SOP | Standard Operating Procedure |
| SRQR | Standards for Reporting Qualitative Research |
Authors’ contributions
LB drafted the manuscript; WW and CG revised the manuscript; all authors approved the final versions.
no external funding.
Availability of data and materials
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
- Harvard Library
- Research Guides
- Faculty of Arts & Sciences Libraries
Library Support for Qualitative Research
- Interview Research
- Resources for Methodology
- Remote Research & Virtual Fieldwork
Resources for Research Interviewing
Nih-funded qualitative research.
- Oral History
- Data Management & Repositories
- Campus Access
Types of Interviews
- Engaging Participants
Interview Questions
- Conducting Interviews
- Transcription
- Coding and Analysis
- Managing & Finding Interview Data
- UX & Market Research Interviews
Textbooks, Guidebooks, and Handbooks
- The Ethnographic Interview by James P. Spradley “Spradley wrote this book for the professional and student who have never done ethnographic fieldwork (p. 231) and for the professional ethnographer who is interested in adapting the author’s procedures (p. iv). Part 1 outlines in 3 chapters Spradley’s version of ethnographic research, and it provides the background for Part 2 which consists of 12 guided steps (chapters) ranging from locating and interviewing an informant to writing an ethnography. Most of the examples come from the author’s own fieldwork among U.S. subcultures . . . Steps 6 and 8 explain lucidly how to construct a domain and a taxonomic analysis” (excerpted from book review by James D. Sexton, 1980).
- Fundamentals of Qualitative Research by Johnny Saldana (Series edited by Patricia Leavy) Provides a soup-to-nuts overview of the qualitative data collection process, including interviewing, participant observation, and other methods.
- InterViews by Steinar Kvale Interviewing is an essential tool in qualitative research and this introduction to interviewing outlines both the theoretical underpinnings and the practical aspects of the process. After examining the role of the interview in the research process, Steinar Kvale considers some of the key philosophical issues relating to interviewing: the interview as conversation, hermeneutics, phenomenology, concerns about ethics as well as validity, and postmodernism. Having established this framework, the author then analyzes the seven stages of the interview process - from designing a study to writing it up.
- Practical Evaluation by Michael Quinn Patton Surveys different interviewing strategies, from, a) informal/conversational, to b) interview guide approach, to c) standardized and open-ended, to d) closed/quantitative. Also discusses strategies for wording questions that are open-ended, clear, sensitive, and neutral, while supporting the speaker. Provides suggestions for probing and maintaining control of the interview process, as well as suggestions for recording and transcription.
- The SAGE Handbook of Interview Research by Amir B. Marvasti (Editor); James A. Holstein (Editor); Jaber F. Gubrium (Editor); Karyn D. McKinney (Editor) The new edition of this landmark volume emphasizes the dynamic, interactional, and reflexive dimensions of the research interview. Contributors highlight the myriad dimensions of complexity that are emerging as researchers increasingly frame the interview as a communicative opportunity as much as a data-gathering format. The book begins with the history and conceptual transformations of the interview, which is followed by chapters that discuss the main components of interview practice. Taken together, the contributions to The SAGE Handbook of Interview Research: The Complexity of the Craft encourage readers simultaneously to learn the frameworks and technologies of interviewing and to reflect on the epistemological foundations of the interview craft.
- The SAGE Handbook of Online Research Methods by Nigel G. Fielding, Raymond M. Lee and Grant Blank (Editors) Bringing together the leading names in both qualitative and quantitative online research, this new edition is organised into nine sections: 1. Online Research Methods 2. Designing Online Research 3. Online Data Capture and Data Collection 4. The Online Survey 5. Digital Quantitative Analysis 6. Digital Text Analysis 7. Virtual Ethnography 8. Online Secondary Analysis: Resources and Methods 9. The Future of Online Social Research
ONLINE RESOURCES, COMMUNITIES, AND DATABASES
- Interviews as a Method for Qualitative Research (video) This short video summarizes why interviews can serve as useful data in qualitative research.
- Companion website to Bloomberg and Volpe's Completing Your Qualitative Dissertation: A Road Map from Beginning to End, 4th ed Provides helpful templates and appendices featured in the book, as well as links to other useful dissertation resources.
- International Congress of Qualitative Inquiry Annual conference hosted by the International Center for Qualitative Inquiry at the University of Illinois at Urbana-Champaign, which aims to facilitate the development of qualitative research methods across a wide variety of academic disciplines, among other initiatives.
- METHODSPACE An online home of the research methods community, where practicing researchers share how to make research easier.
- SAGE researchmethods Researchers can explore methods concepts to help them design research projects, understand particular methods or identify a new method, conduct their research, and write up their findings. A "methods map" facilitates finding content on methods.
The decision to conduct interviews, and the type of interviewing to use, should flow from, or align with, the methodological paradigm chosen for your study, whether that paradigm is interpretivist, critical, positivist, or participative in nature (or a combination of these).
Structured:
- Structured Interview. Entry in The SAGE Encyclopedia of Social Science Research Methodsby Floyd J. Fowler Jr., Editors: Michael S. Lewis-Beck; Alan E. Bryman; Tim Futing Liao (Editor) A concise article noting standards, procedures, and recommendations for developing and testing structured interviews. For an example of structured interview questions, you may view the Current Population Survey, May 2008: Public Participation in the Arts Supplement (ICPSR 29641), Apr 15, 2011 at https://doi.org/10.3886/ICPSR29641.v1 (To see the survey questions, preview the user guide, which can be found under the "Data and Documentation" tab. Then, look for page 177 (attachment 8).
Semi-Structured:
- Semi-Structured Interview. Entry in The SAGE Encyclopedia of Qualitative Research Methodsby Lioness Ayres; Editor: Lisa M. Given The semi-structured interview is a qualitative data collection strategy in which the researcher asks informants a series of predetermined but open-ended questions. The researcher has more control over the topics of the interview than in unstructured interviews, but in contrast to structured interviews or questionnaires that use closed questions, there is no fixed range of responses to each question.
Unstructured:
- Unstructured Interview. Entry in The SAGE Encyclopedia of Qualitative Research Methodsby Michael W. Firmin; Editor: Lisa M. Given Unstructured interviews in qualitative research involve asking relatively open-ended questions of research participants in order to discover their percepts on the topic of interest. Interviews, in general, are a foundational means of collecting data when using qualitative research methods. They are designed to draw from the interviewee constructs embedded in his or her thinking and rationale for decision making. The researcher uses an inductive method in data gathering, regardless of whether the interview method is open, structured, or semi-structured. That is, the researcher does not wish to superimpose his or her own viewpoints onto the person being interviewed. Rather, inductively, the researcher wishes to understand the participant's perceptions, helping him or her to articulate percepts such that they will be understood clearly by the journal reader.
Genres and Uses
Focus groups:.
- "Focus Groups." Annual Review of Sociology 22 (1996): 129-1524.by David L. Morgan Discusses the use of focus groups and group interviews as methods for gathering qualitative data used by sociologists and other academic and applied researchers. Focus groups are recommended for giving voice to marginalized groups and revealing the group effect on opinion formation.
- Qualitative Research Methods: A Data Collector's Field Guide (See Module 4: "Focus Groups")by Mack, N., et al. This field guide is based on an approach to doing team-based, collaborative qualitative research that has repeatedly proven successful in research projects sponsored by Family Health International (FHI) throughout the developing world. With its straightforward delivery of information on the main qualitative methods being used in public health research today, the guide speaks to the need for simple yet effective instruction on how to do systematic and ethically sound qualitative research. The aim of the guide is thus practical. In bypassing extensive discussion on the theoretical underpinnings of qualitative research, it distinguishes itself as a how-to guide to be used in the field.
In-Depth (typically One-on-One):
- A Practical Introduction to in-Depth Interviewingby Alan Morris Are you new to qualitative research or a bit rusty and in need of some inspiration? Are you doing a research project involving in-depth interviews? Are you nervous about carrying out your interviews? This book will help you complete your qualitative research project by providing a nuts and bolts introduction to interviewing. With coverage of ethics, preparation strategies and advice for handling the unexpected in the field, this handy guide will help you get to grips with the basics of interviewing before embarking on your research. While recognising that your research question and the context of your research will drive your approach to interviewing, this book provides practical advice often skipped in traditional methods textbooks.
- Qualitative Research Methods: A Data Collector's Field Guide (See Module 3: "In-Depth Interviews")by Mack, N., et al. This field guide is based on an approach to doing team-based, collaborative qualitative research that has repeatedly proven successful in research projects sponsored by Family Health International (FHI) throughout the developing world. With its straightforward delivery of information on the main qualitative methods being used in public health research today, the guide speaks to the need for simple yet effective instruction on how to do systematic and ethically sound qualitative research. The aim of the guide is thus practical. In bypassing extensive discussion on the theoretical underpinnings of qualitative research, it distinguishes itself as a how-to guide to be used in the field.
Folklore Research and Oral Histories:
In addition to the following resource, see the Oral History page of this guide for helpful resources on Oral History interviewing.
American Folklife Center at the Library of Congress. Folklife and Fieldwork: A Layman’s Introduction to Field Techniques Interviews gathered for purposes of folklore research are similar to standard social science interviews in some ways, but also have a good deal in common with oral history approaches to interviewing. The focus in a folklore research interview is on documenting and trying to understand the interviewee's way of life relative to a culture or subculture you are studying. This guide includes helpful advice and tips for conducting fieldwork in folklore, such as tips for planning, conducting, recording, and archiving interviews.
An interdisciplinary scientific program within the Institute for Quantitative Social Science which encourages and facilitates research and instruction in the theory and practice of survey research. The primary mission of PSR is to provide survey research resources to enhance the quality of teaching and research at Harvard.
- Internet, Phone, Mail, and Mixed-Mode Surveysby Don A. Dillman; Jolene D. Smyth; Leah Melani Christian The classic survey design reference, updated for the digital age. The new edition is thoroughly updated and revised, and covers all aspects of survey research. It features expanded coverage of mobile phones, tablets, and the use of do-it-yourself surveys, and Dillman's unique Tailored Design Method is also thoroughly explained. This new edition is complemented by copious examples within the text and accompanying website. It includes: Strategies and tactics for determining the needs of a given survey, how to design it, and how to effectively administer it. How and when to use mail, telephone, and Internet surveys to maximum advantage. Proven techniques to increase response rates. Guidance on how to obtain high-quality feedback from mail, electronic, and other self-administered surveys. Direction on how to construct effective questionnaires, including considerations of layout. The effects of sponsorship on the response rates of surveys. Use of capabilities provided by newly mass-used media: interactivity, presentation of aural and visual stimuli. The Fourth Edition reintroduces the telephone--including coordinating land and mobile.
User Experience (UX) and Marketing:
- See the "UX & Market Research Interviews" tab on this guide, above. May include Focus Groups, above.
Screening for Research Site Selection:
- Research interviews are used not only to furnish research data for theoretical analysis in the social sciences, but also to plan other kinds of studies. For example, interviews may allow researchers to screen appropriate research sites to conduct empirical studies (such as randomized controlled trials) in a variety of fields, from medicine to law. In contrast to interviews conducted in the course of social research, such interviews do not typically serve as the data for final analysis and publication.
ENGAGING PARTICIPANTS
Research ethics .
- Human Subjects (IRB) The Committee on the Use of Human Subjects (CUHS) serves as the Institutional Review Board for the University area which includes the Cambridge and Allston campuses at Harvard. Find your IRB contact person , or learn about required ethics training. You may also find the IRB Lifecycle Guide helpful. This is the preferred IRB portal for Harvard graduate students and other researchers. IRB forms can be downloaded via the ESTR Library (click on the "Templates and Forms" tab, then navigate to pages 2 and 3 to find the documents labelled with “HUA” for the Harvard University Area IRB. Nota bene: You may use these forms only if you submit your study to the Harvard University IRB). The IRB office can be reached through email at [email protected] or by telephone at (617) 496-2847.
- Undergraduate Research Training Program (URTP) Portal The URTP at Harvard University is a comprehensive platform to create better prepared undergraduate researchers. The URTP is comprised of research ethics training sessions, a student-focused curriculum, and an online decision form that will assist students in determining whether their project requires IRB review. Students should examine the URTP's guide for student researchers: Introduction to Human Subjects Research Protection.
- Ethics reports From the Association of Internet Researchers (AoIR)
- Respect, Beneficence, and Justice: QDR General Guidance for Human Participants If you are hoping to share your qualitative interview data in a repository after it has been collected, you will need to plan accordingly via informed consent, careful de-identification procedures, and data access controls. Consider consulting with the Qualitative Research Support Group at Harvard Library and consulting with Harvard's Dataverse contacts to help you think through all of the contingencies and processes.
- "Conducting a Qualitative Child Interview: Methodological Considerations." Journal of Advanced Nursing 42/5 (2003): 434-441 by Kortesluoma, R., et al. The purpose of this article is to illustrate the theoretical premises of child interviewing, as well as to describe some practical methodological solutions used during interviews. Factors that influence data gathered from children and strategies for taking these factors into consideration during the interview are also described.
- "Crossing Cultural Barriers in Research Interviewing." Qualitative Social Work 63/3 (2007): 353-372 by Sands, R., et al. This article critically examines a qualitative research interview in which cultural barriers between a white non-Muslim female interviewer and an African American Muslim interviewee, both from the USA, became evident and were overcome within the same interview.
- Decolonizing Methodologies: Research and Indigenous Peoples by Linda Tuhiwai Smith This essential volume explores intersections of imperialism and research - specifically, the ways in which imperialism is embedded in disciplines of knowledge and tradition as 'regimes of truth.' Concepts such as 'discovery' and 'claiming' are discussed and an argument presented that the decolonization of research methods will help to reclaim control over indigenous ways of knowing and being. The text includes case-studies and examples, and sections on new indigenous literature and the role of research in indigenous struggles for social justice.
This resource, sponsored by University of Oregon Libraries, exemplifies the use of interviewing methodologies in research that foregrounds traditional knowledge. The methodology page summarizes the approach.
- Ethics: The Need to Tread Carefully. Chapter in A Practical Introduction to in-Depth Interviewing by Alan Morris Pay special attention to the sections in chapter 2 on "How to prevent and respond to ethical issues arising in the course of the interview," "Ethics in the writing up of your interviews," and "The Ethics of Care."
- Handbook on Ethical Issues in Anthropology by Joan Cassell (Editor); Sue-Ellen Jacobs (Editor) This publication of the American Anthropological Association presents and discusses issues and sources on ethics in anthropology, as well as realistic case studies of ethical dilemmas. It is meant to help social science faculty introduce discussions of ethics in their courses. Some of the topics are relevant to interviews, or at least to studies of which interviews are a part. See chapters 3 and 4 for cases, with solutions and commentary, respectively.
- Research Ethics from the Chanie Wenjack School for Indigenous Studies, Trent University (Open Access) An overview of Indigenous research ethics and protocols from the across the globe.
- Resources for Equity in Research Consult these resources for guidance on creating and incorporating equitable materials into public health research studies that entail community engagement.
The SAGE Handbook of Qualitative Research Ethics by Ron Iphofen (Editor); Martin Tolich (Editor) This handbook is a much-needed and in-depth review of the distinctive set of ethical considerations which accompanies qualitative research. This is particularly crucial given the emergent, dynamic and interactional nature of most qualitative research, which too often allows little time for reflection on the important ethical responsibilities and obligations. Contributions from leading international researchers have been carefully organized into six key thematic sections: Part One: Thick Descriptions Of Qualitative Research Ethics; Part Two: Qualitative Research Ethics By Technique; Part Three: Ethics As Politics; Part Four: Qualitative Research Ethics With Vulnerable Groups; Part Five: Relational Research Ethics; Part Six: Researching Digitally. This Handbook is a one-stop resource on qualitative research ethics across the social sciences that draws on the lessons learned and the successful methods for surmounting problems - the tried and true, and the new.
RESEARCH COMPLIANCE AND PRIVACY LAWS
Research Compliance Program for FAS/SEAS at Harvard : The Faculty of Arts and Sciences (FAS), including the School of Engineering and Applied Sciences (SEAS), and the Office of the Vice Provost for Research (OVPR) have established a shared Research Compliance Program (RCP). An area of common concern for interview studies is international projects and collaboration . RCP is a resource to provide guidance on which international activities may be impacted by US sanctions on countries, individuals, or entities and whether licenses or other disclosure are required to ship or otherwise share items, technology, or data with foreign collaborators.
- Harvard Global Support Services (GSS) is for students, faculty, staff, and researchers who are studying, researching, or working abroad. Their services span safety and security, health, culture, outbound immigration, employment, financial and legal matters, and research center operations. These include travel briefings and registration, emergency response, guidance on international projects, and managing in-country operations.
Generative AI: Harvard-affiliated researchers should not enter data classified as confidential ( Level 2 and above ), including non-public research data, into publicly-available generative AI tools, in accordance with the University’s Information Security Policy. Information shared with generative AI tools using default settings is not private and could expose proprietary or sensitive information to unauthorized parties.
Privacy Laws: Be mindful of any potential privacy laws that may apply wherever you conduct your interviews. The General Data Protection Regulation is a high-profile example (see below):
- General Data Protection Regulation (GDPR) This Regulation lays down rules relating to the protection of natural persons with regard to the processing of personal data and rules relating to the free movement of personal data. It protects fundamental rights and freedoms of natural persons and in particular their right to the protection of personal data. The free movement of personal data within the Union shall be neither restricted nor prohibited for reasons connected with the protection of natural persons with regard to the processing of personal data. For a nice summary of what the GDPR requires, check out the GDPR "crash course" here .
SEEKING CONSENT
If you would like to see examples of consent forms, ask your local IRB, or take a look at these resources:
- Model consent forms for oral history, suggested by the Centre for Oral History and Digital Storytelling at Concordia University
- For NIH-funded research, see this resource for developing informed consent language in research studies where data and/or biospecimens will be stored and shared for future use.
POPULATION SAMPLING
If you wish to assemble resources to aid in sampling, such as the USPS Delivery Sequence File, telephone books, or directories of organizations and listservs, please contact our data librarian or write to [email protected] .
- Research Randomizer A free web-based service that permits instant random sampling and random assignment. It also contains an interactive tutorial perfect for students taking courses in research methods.
- Practical Tools for Designing and Weighting Survey Samples by Richard Valliant; Jill A. Dever; Frauke Kreuter Survey sampling is fundamentally an applied field. The goal in this book is to put an array of tools at the fingertips of practitioners by explaining approaches long used by survey statisticians, illustrating how existing software can be used to solve survey problems, and developing some specialized software where needed. This book serves at least three audiences: (1) Students seeking a more in-depth understanding of applied sampling either through a second semester-long course or by way of a supplementary reference; (2) Survey statisticians searching for practical guidance on how to apply concepts learned in theoretical or applied sampling courses; and (3) Social scientists and other survey practitioners who desire insight into the statistical thinking and steps taken to design, select, and weight random survey samples. Several survey data sets are used to illustrate how to design samples, to make estimates from complex surveys for use in optimizing the sample allocation, and to calculate weights. Realistic survey projects are used to demonstrate the challenges and provide a context for the solutions. The book covers several topics that either are not included or are dealt with in a limited way in other texts. These areas include: sample size computations for multistage designs; power calculations related to surveys; mathematical programming for sample allocation in a multi-criteria optimization setting; nuts and bolts of area probability sampling; multiphase designs; quality control of survey operations; and statistical software for survey sampling and estimation. An associated R package, PracTools, contains a number of specialized functions for sample size and other calculations. The data sets used in the book are also available in PracTools, so that the reader may replicate the examples or perform further analyses.
- Sampling: Design and Analysis by Sharon L. Lohr Provides a modern introduction to the field of sampling. With a multitude of applications from a variety of disciplines, the book concentrates on the statistical aspects of taking and analyzing a sample. Overall, the book gives guidance on how to tell when a sample is valid or not, and how to design and analyze many different forms of sample surveys.
- Sampling Techniques by William G. Cochran Clearly demonstrates a wide range of sampling methods now in use by governments, in business, market and operations research, social science, medicine, public health, agriculture, and accounting. Gives proofs of all the theoretical results used in modern sampling practice. New topics in this edition include the approximate methods developed for the problem of attaching standard errors or confidence limits to nonlinear estimates made from the results of surveys with complex plans.
- "Understanding the Process of Qualitative Data Collection" in Chapter 13 (pp. 103–1162) of 30 Essential Skills for the Qualitative Researcher by John W. Creswell Provides practical "how-to" information for beginning researchers in the social, behavioral, and health sciences with many applied examples from research design, qualitative inquiry, and mixed methods.The skills presented in this book are crucial for a new qualitative researcher starting a qualitative project.
- Survey Methodology by Robert M. Groves; Floyd J. Fowler; Mick P. Couper; James M. Lepkowski; Eleanor Singer; Roger Tourangeau; Floyd J. Fowler coverage includes sampling frame evaluation, sample design, development of questionnaires, evaluation of questions, alternative modes of data collection, interviewing, nonresponse, post-collection processing of survey data, and practices for maintaining scientific integrity.
The way a qualitative researcher constructs and approaches interview questions should flow from, or align with, the methodological paradigm chosen for the study, whether that paradigm is interpretivist, critical, positivist, or participative in nature (or a combination of these).
Constructing Your Questions
Helpful texts:.
- "Developing Questions" in Chapter 4 (pp. 98–108) of Becoming Qualitative Researchers by Corrine Glesne Ideal for introducing the novice researcher to the theory and practice of qualitative research, this text opens students to the diverse possibilities within this inquiry approach, while helping them understand how to design and implement specific research methods.
- "Learning to Interview in the Social Sciences" Qualitative Inquiry, 9(4) 2003, 643–668 by Roulston, K., deMarrais, K., & Lewis, J. B. See especially the section on "Phrasing and Negotiating Questions" on pages 653-655 and common problems with framing questions noted on pages 659 - 660.
- Qualitative Research Interviewing: Biographic Narrative and Semi-Structured Methods (See sections on “Lightly and Heavily Structured Depth Interviewing: Theory-Questions and Interviewer-Questions” and “Preparing for any Interviewing Sequence") by Tom Wengraf Unique in its conceptual coherence and the level of practical detail, this book provides a comprehensive resource for those concerned with the practice of semi-structured interviewing, the most commonly used interview approach in social research, and in particular for in-depth, biographic narrative interviewing. It covers the full range of practices from the identification of topics through to strategies for writing up research findings in diverse ways.
- "Scripting a Qualitative Purpose Statement and Research Questions" in Chapter 12 (pp. 93–102) of 30 Essential Skills for the Qualitative Researcher by John W. Creswell Provides practical "how-to" information for beginning researchers in the social, behavioral, and health sciences with many applied examples from research design, qualitative inquiry, and mixed methods.The skills presented in this book are crucial for a new qualitative researcher starting a qualitative project.
- Some Strategies for Developing Interview Guides for Qualitative Interviews by Sociology Department, Harvard University Includes general advice for conducting qualitative interviews, pros and cons of recording and transcription, guidelines for success, and tips for developing and phrasing effective interview questions.
- Tip Sheet on Question Wording by Harvard University Program on Survey Research
Let Theory Guide You:
The quality of your questions depends on how you situate them within a wider body of knowledge. Consider the following advice:
A good literature review has many obvious virtues. It enables the investigator to define problems and assess data. It provides the concepts on which percepts depend. But the literature review has a special importance for the qualitative researcher. This consists of its ability to sharpen his or her capacity for surprise (Lazarsfeld, 1972b). The investigator who is well versed in the literature now has a set of expectations the data can defy. Counterexpectational data are conspicuous, readable, and highly provocative data. They signal the existence of unfulfilled theoretical assumptions, and these are, as Kuhn (1962) has noted, the very origins of intellectual innovation. A thorough review of the literature is, to this extent, a way to manufacture distance. It is a way to let the data of one's research project take issue with the theory of one's field.
McCracken, G. (1988), The Long Interview, Sage: Newbury Park, CA, p. 31
When drafting your interview questions, remember that everything follows from your central research question. Also, on the way to writing your "operationalized" interview questions, it's helpful to draft broader, intermediate questions, couched in theory. Nota bene: While it is important to know the literature well before conducting your interview(s), be careful not to present yourself to your research participant(s) as "the expert," which would be presumptuous and could be intimidating. Rather, the purpose of your knowledge is to make you a better, keener listener.
If you'd like to supplement what you learned about relevant theories through your coursework and literature review, try these sources:
- Annual Reviews Review articles sum up the latest research in many fields, including social sciences, biomedicine, life sciences, and physical sciences. These are timely collections of critical reviews written by leading scientists.
- HOLLIS - search for resources on theories in your field Modify this example search by entering the name of your field in place of "your discipline," then hit search.
- Oxford Bibliographies Written and reviewed by academic experts, every article in this database is an authoritative guide to the current scholarship in a variety of fields, containing original commentary and annotations.
- ProQuest Dissertations & Theses (PQDT) Indexes dissertations and masters' theses from most North American graduate schools as well as some European universities. Provides full text for most indexed dissertations from 1990-present.
- Very Short Introductions Launched by Oxford University Press in 1995, Very Short Introductions offer concise introductions to a diverse range of subjects from Climate to Consciousness, Game Theory to Ancient Warfare, Privacy to Islamic History, Economics to Literary Theory.
CONDUCTING INTERVIEWS
Equipment and software: .
- Lamont Library loans microphones and podcast starter kits, which will allow you to capture audio (and you may record with software, such as Garage Band).
- Cabot Library loans digital recording devices, as well as USB microphones.
If you prefer to use your own device, you may purchase a small handheld audio recorder, or use your cell phone.
- Audio Capture Basics (PDF) - Helpful instructions, courtesy of the Lamont Library Multimedia Lab.
- Getting Started with Podcasting/Audio: Guidelines from Harvard Library's Virtual Media Lab for preparing your interviewee for a web-based recording (e.g., podcast, interview)
- Camtasia Screen Recorder and Video Editor
- Zoom: Video Conferencing, Web Conferencing
- Visit the Multimedia Production Resources guide! Consult it to find and learn how to use audiovisual production tools, including: cameras, microphones, studio spaces, and other equipment at Cabot Science Library and Lamont Library.
- Try the virtual office hours offered by the Lamont Multimedia Lab!
TIPS FOR CONDUCTING INTERVIEWS
Quick handout: .
- Research Interviewing Tips (Courtesy of Dr. Suzanne Spreadbury)
Remote Interviews:
- For Online or Distant Interviews, See "Remote Research & Virtual Fieldwork" on this guide .
- Deborah Lupton's Bibliography: Doing Fieldwork in a Pandemic
Seeking Consent:
Books and articles: .
- "App-Based Textual Interviews: Interacting With Younger Generations in a Digitalized Social Reallity."International Journal of Social Research Methodology (12 June 2022). Discusses the use of texting platforms as a means to reach young people. Recommends useful question formulations for this medium.
- "Learning to Interview in the Social Sciences." Qualitative Inquiry, 9(4) 2003, 643–668 by Roulston, K., deMarrais, K., & Lewis, J. B. See especially the section on "Phrasing and Negotiating Questions" on pages 653-655 and common problems with framing questions noted on pages 659-660.
- "Slowing Down and Digging Deep: Teaching Students to Examine Interview Interaction in Depth." LEARNing Landscapes, Spring 2021 14(1) 153-169 by Herron, Brigette A. and Kathryn Roulston. Suggests analysis of videorecorded interviews as a precursor to formulating one's own questions. Includes helpful types of probes.
- Using Interviews in a Research Project by Nigel Joseph Mathers; Nicholas J Fox; Amanda Hunn; Trent Focus Group. A work pack to guide researchers in developing interviews in the healthcare field. Describes interview structures, compares face-to-face and telephone interviews. Outlines the ways in which different types of interview data can be analysed.
- “Working through Challenges in Doing Interview Research.” International Journal of Qualitative Methods, (December 2011), 348–66 by Roulston, Kathryn. The article explores (1) how problematic interactions identified in the analysis of focus group data can lead to modifications in research design, (2) an approach to dealing with reported data in representations of findings, and (3) how data analysis can inform question formulation in successive rounds of data generation. Findings from these types of examinations of interview data generation and analysis are valuable for informing both interview practice as well as research design.
Videos:

The way a qualitative researcher transcribes interviews should flow from, or align with, the methodological paradigm chosen for the study, whether that paradigm is interpretivist, critical, positivist, or participative in nature (or a combination of these).
TRANSCRIPTION
Before embarking on a transcription project, it's worthwhile to invest in the time and effort necessary to capture good audio, which will make the transcription process much easier. If you haven't already done so, check out the audio capture guidelines from Harvard Library's Virtual Media Lab , or contact a media staff member for customized recommendations. First and foremost, be mindful of common pitfalls by watching this short video that identifies the most common errors to avoid!
SOFTWARE:
- Adobe Premiere Pro Speech-To-Text automatically generates transcripts and adds captions to your videos. Harvard affiliates can download Adobe Premiere in the Creative Cloud Suite.
- GoTranscript provides cost-effective human-generated transcriptions.
- pyTranscriber is an app for generating automatic transcription and/or subtitles for audio and video files. It uses the Google Cloud Speech-to-Text service, has a friendly graphical user interface, and is purported to work nicely with Chinese.
- Otter provides a new way to capture, store, search and share voice conversations, lectures, presentations, meetings, and interviews. The startup is based in Silicon Valley with a team of experienced Ph.Ds and engineers from Google, Facebook, Yahoo and Nuance (à la Dragon). Free accounts available. This is the software that Zoom uses to generate automated transcripts, so if you have access to a Zoom subscription, you have access to Otter transcriptions with it (applicable in several languages ). As with any automated approach, be prepared to correct any errors after the fact, by hand.
- Panopto is available to Harvard affiliates and generates ASR (automated speech recognition) captions . You may upload compatible audio files into it. As with any automatically generated transcription, you will need to make manual revisions. ASR captioning is available in several languages . Panopto maintains robust security practices, including strong authentication measures and end-to-end encryption, ensuring your content remains private and protected.
- REV.Com allows you to record and transcribe any calls on the iPhone, both outgoing and incoming. It may be useful for recording phone interviews. Rev lets you choose whether you want an AI- or human-generated transcription, with a fast turnaround. Rev has Service Organization Controls Type II (SOC2) certification (a SOC2 cert looks at and verifies an organization’s processing integrity, privacy practices, and security safeguards).
- Scribie Audio/Video Transcription provides automated or manual transcriptions for a small fee. As with any transcription service, some revisions will be necessary after the fact, particularly for its automated transcripts.
- Sonix automatically transcribes, translates, and helps to organize audio and video files in over 40 languages. It's fast and affordable, with good accuracy. The free trial includes 30 minutes of free transcription.
- TranscriptionWing uses a human touch process to clean up machine-generated transcripts so that the content will far more accurately reflect your audio recording.
- Whisper is a tool from OpenAI that facilitates transcription of sensitive audiovisual recordings (e.g., of research interviews) on your own device. Installation and use depends on your operating system and which version you install. Important Note: The Whisper API, where audio is sent to OpenAI to be processed by them and then sent back (usually through a programming language like Python) is NOT appropriate for sensitive data. The model should be downloaded with tools such as those described in this FAQ , so that audio is kept to your local machine. For assistance, contact James Capobianco .
EQUIPMENT:
- Transcription pedals are in circulation and available to borrow from the Circulation desk at Lamont, or use at Lamont Library's Media Lab on level B. For hand-transcribing your interviews, they work in conjunction with software such as Express Scribe , which is loaded on Media Lab computers, or you may download for free on your own machine (Mac or PC versions; scroll down the downloads page for the latter). The pedals are plug-and-play USB, allow a wide range of playback speeds, and have 3 programmable buttons, which are typically set to rewind/play/fast-forward. Instructions are included in the bag that covers installation and set-up of the software, and basic use of the pedals.
NEED HELP?
- Try the virtual office hours offered by the Lamont Multimedia Lab!
- If you're creating podcasts, login to Canvas and check out the Podcasting/Audio guide .
Helpful Texts:
- "Transcription as a Crucial Step of Data Analysis" in Chapter 5 of The SAGE Handbook of Qualitative Data Analysisby Uwe Flick (Editor) Covers basic terminology for transcription, shares caveats for transcribers, and identifies components of vocal behavior. Provides notation systems for transcription, suggestions for transcribing turn-taking, and discusses new technologies and perspectives. Includes a bibliography for further reading.
- "Transcribing the Oral Interview: Part Art, Part Science " on p. 10 of the Centre for Community Knowledge (CCK) newsletter: TIMESTAMPby Mishika Chauhan and Saransh Srivastav
QUALITATIVE DATA ANALYSIS
Software .
- Free download available for Harvard Faculty of Arts and Sciences (FAS) affiliates
- Desktop access at Lamont Library Media Lab, 3rd floor
- Desktop access at Harvard Kennedy School Library (with HKS ID)
- Remote desktop access for Harvard affiliates from IQSS Computer Labs . Email them at [email protected] and ask for a new lab account and remote desktop access to NVivo.
- Virtual Desktop Infrastructure (VDI) access available to Harvard T.H. Chan School of Public Health affiliates
CODING AND THEMEING YOUR DATA
Data analysis methods should flow from, or align with, the methodological paradigm chosen for your study, whether that paradigm is interpretivist, critical, positivist, or participative in nature (or a combination of these). Some established methods include Content Analysis, Critical Analysis, Discourse Analysis, Gestalt Analysis, Grounded Theory Analysis, Interpretive Analysis, Narrative Analysis, Normative Analysis, Phenomenological Analysis, Rhetorical Analysis, and Semiotic Analysis, among others. The following resources should help you navigate your methodological options and put into practice methods for coding, themeing, interpreting, and presenting your data.
- Users can browse content by topic, discipline, or format type (reference works, book chapters, definitions, etc.). SRM offers several research tools as well: a methods map, user-created reading lists, a project planner, and advice on choosing statistical tests.
- Abductive Coding: Theory Building and Qualitative (Re)Analysis by Vila-Henninger, et al. The authors recommend an abductive approach to guide qualitative researchers who are oriented towards theory-building. They outline a set of tactics for abductive analysis, including the generation of an abductive codebook, abductive data reduction through code equations, and in-depth abductive qualitative analysis.
- Analyzing and Interpreting Qualitative Research: After the Interview by Charles F. Vanover, Paul A. Mihas, and Johnny Saldana (Editors) Providing insight into the wide range of approaches available to the qualitative researcher and covering all steps in the research process, the authors utilize a consistent chapter structure that provides novice and seasoned researchers with pragmatic, "how-to" strategies. Each chapter author introduces the method, uses one of their own research projects as a case study of the method described, shows how the specific analytic method can be used in other types of studies, and concludes with three questions/activities to prompt class discussion or personal study.
- "Analyzing Qualitative Data." Theory Into Practice 39, no. 3 (2000): 146-54 by Margaret D. LeCompte This article walks readers though rules for unbiased data analysis and provides guidance for getting organized, finding items, creating stable sets of items, creating patterns, assembling structures, and conducting data validity checks.
- "Coding is Not a Dirty Word" in Chapter 1 (pp. 1–30) of Enhancing Qualitative and Mixed Methods Research with Technology by Shalin Hai-Jew (Editor) Current discourses in qualitative research, especially those situated in postmodernism, represent coding and the technology that assists with coding as reductive, lacking complexity, and detached from theory. In this chapter, the author presents a counter-narrative to this dominant discourse in qualitative research. The author argues that coding is not necessarily devoid of theory, nor does the use of software for data management and analysis automatically render scholarship theoretically lightweight or barren. A lack of deep analytical insight is a consequence not of software but of epistemology. Using examples informed by interpretive and critical approaches, the author demonstrates how NVivo can provide an effective tool for data management and analysis. The author also highlights ideas for critical and deconstructive approaches in qualitative inquiry while using NVivo. By troubling the positivist discourse of coding, the author seeks to create dialogic spaces that integrate theory with technology-driven data management and analysis, while maintaining the depth and rigor of qualitative research.
- The Coding Manual for Qualitative Researchers by Johnny Saldana An in-depth guide to the multiple approaches available for coding qualitative data. Clear, practical and authoritative, the book profiles 32 coding methods that can be applied to a range of research genres from grounded theory to phenomenology to narrative inquiry. For each approach, Saldaña discusses the methods, origins, a description of the method, practical applications, and a clearly illustrated example with analytic follow-up. Essential reading across the social sciences.
- Flexible Coding of In-depth Interviews: A Twenty-first-century Approach by Nicole M. Deterding and Mary C. Waters The authors suggest steps in data organization and analysis to better utilize qualitative data analysis technologies and support rigorous, transparent, and flexible analysis of in-depth interview data.
- From the Editors: What Grounded Theory is Not by Roy Suddaby Walks readers through common misconceptions that hinder grounded theory studies, reinforcing the two key concepts of the grounded theory approach: (1) constant comparison of data gathered throughout the data collection process and (2) the determination of which kinds of data to sample in succession based on emergent themes (i.e., "theoretical sampling").
- “Good enough” methods for life-story analysis, by Wendy Luttrell. In Quinn N. (Ed.), Finding culture in talk (pp. 243–268). Demonstrates for researchers of culture and consciousness who use narrative how to concretely document reflexive processes in terms of where, how and why particular decisions are made at particular stages of the research process.
- The Ethnographic Interview by James P. Spradley “Spradley wrote this book for the professional and student who have never done ethnographic fieldwork (p. 231) and for the professional ethnographer who is interested in adapting the author’s procedures (p. iv) ... Steps 6 and 8 explain lucidly how to construct a domain and a taxonomic analysis” (excerpted from book review by James D. Sexton, 1980). See also: Presentation slides on coding and themeing your data, derived from Saldana, Spradley, and LeCompte Click to request access.
- Qualitative Data Analysis by Matthew B. Miles; A. Michael Huberman A practical sourcebook for researchers who make use of qualitative data, presenting the current state of the craft in the design, testing, and use of qualitative analysis methods. Strong emphasis is placed on data displays matrices and networks that go beyond ordinary narrative text. Each method of data display and analysis is described and illustrated.
- "A Survey of Qualitative Data Analytic Methods" in Chapter 4 (pp. 89–138) of Fundamentals of Qualitative Research by Johnny Saldana Provides an in-depth introduction to coding as a heuristic, particularly focusing on process coding, in vivo coding, descriptive coding, values coding, dramaturgical coding, and versus coding. Includes advice on writing analytic memos, developing categories, and themeing data.
- "Thematic Networks: An Analytic Tool for Qualitative Research." Qualitative Research : QR, 1(3), 385–405 by Jennifer Attride-Stirling Details a technique for conducting thematic analysis of qualitative material, presenting a step-by-step guide of the analytic process, with the aid of an empirical example. The analytic method presented employs established, well-known techniques; the article proposes that thematic analyses can be usefully aided by and presented as thematic networks.
- Using Thematic Analysis in Psychology by Virginia Braun and Victoria Clark Walks readers through the process of reflexive thematic analysis, step by step. The method may be adapted in fields outside of psychology as relevant. Pair this with One Size Fits All? What Counts as Quality Practice in Reflexive Thematic Analysis? by Virginia Braun and Victoria Clark
TESTING OR GENERATING THEORIES
The quality of your data analysis depends on how you situate what you learn within a wider body of knowledge. Consider the following advice:
Once you have coalesced around a theory, realize that a theory should reveal rather than color your discoveries. Allow your data to guide you to what's most suitable. Grounded theory researchers may develop their own theory where current theories fail to provide insight. This guide on Theoretical Models from Alfaisal University Library provides a helpful overview on using theory.
MANAGING & FINDING INTERVIEW DATA
Managing your elicited interview data, general guidance: .
- Research Data Management @ Harvard A reference guide with information and resources to help you manage your research data. See also: Harvard Research Data Security Policy , on the Harvard University Research Data Management website.
- Data Management For Researchers: Organize, Maintain and Share Your Data for Research Success by Kristin Briney. A comprehensive guide for scientific researchers providing everything they need to know about data management and how to organize, document, use and reuse their data.
- Open Science Framework (OSF) An open-source project management tool that makes it easy to collaborate within and beyond Harvard throughout a project's lifecycle. With OSF you can manage, store, and share documents, datasets, and other information with your research team. You can also publish your work to share it with a wider audience. Although data can be stored privately, because this platform is hosted on the Internet and designed with open access in mind, it is not a good choice for highly sensitive data.
- Free cloud storage solutions for Harvard affiliates to consider include: Google Drive , DropBox , or OneDrive ( up to DSL3 )
Data Confidentiality and Secure Handling:
- Data Security Levels at Harvard - Research Data Examples This resource provided by Harvard Data Security helps you determine what level of access is appropriate for your data. Determine whether it should be made available for public use, limited to the Harvard community, or be protected as either "confidential and sensitive," "high risk," or "extremely sensitive." See also: Harvard Data Classification Table
- Harvard's Best Practices for Protecting Privacy and Harvard Information Security Collaboration Tools Matrix Follow the nuts-and-bolts advice for privacy best practices at Harvard. The latter resource reveals the level of security that can be relied upon for a large number of technological tools and platforms used at Harvard to conduct business, such as email, Slack, Accellion Kiteworks, OneDrive/SharePoint, etc.
- “Protecting Participant Privacy While Maintaining Content and Context: Challenges in Qualitative Data De‐identification and Sharing.” Proceedings of the ASIST Annual Meeting 57 (1) (2020): e415-420 by Myers, Long, and Polasek Presents an informed and tested protocol, based on the De-Identification guidelines published by the Qualitative Data Repository (QDR) at Syracuse University. Qualitative researchers may consult it to guide their data de-identification efforts.
- QDS Qualitative Data Sharing Toolkit The Qualitative Data Sharing (QDS) project and its toolkit was funded by the NIH National Human Genome Research Institute (R01HG009351). It provides tools and resources to help researchers, especially those in the health sciences, share qualitative research data while protecting privacy and confidentiality. It offers guidance on preparing data for sharing through de-identification and access control. These health sciences research datasets in ICPSR's Qualitative Data Sharing (QDS) Project Series were de-identified using the QuaDS Software and the project’s QDS guidelines.
- Table of De-Identification Techniques
- Generative AI Harvard-affiliated researchers should not enter data classified as confidential ( Level 2 and above ), including non-public research data, into publicly-available generative AI tools, in accordance with the University’s Information Security Policy. Information shared with generative AI tools using default settings is not private and could expose proprietary or sensitive information to unauthorized parties.
- Harvard Information Security Quick Reference Guide Storage guidelines, based on the data's security classification level (according to its IRB classification) is displayed on page 2, under "handling."
- Email Encryption Harvard Microsoft 365 users can now send encrypted messages and files directly from the Outlook web or desktop apps. Encrypting an email adds an extra layer of security to the message and its attachments (up to 150MB), and means only the intended recipient (and their inbox delegates with full access) can view it. Message encryption in Outlook is approved for sending high risk ( level 4 ) data and below.
Sharing Qualitative Data:
- Repositories for Qualitative Data If you have cleared this intention with your IRB, secured consent from participants, and properly de-identified your data, consider sharing your interviews in one of the data repositories included in the link above. Depending on the nature of your research and the level of risk it may present to participants, sharing your interview data may not be appropriate. If there is any chance that sharing such data will be desirable, you will be much better off if you build this expectation into your plans from the beginning.
- Guide for Sharing Qualitative Data at ICPSR The Inter-university Consortium for Political and Social Research (ICPSR) has created this resource for investigators planning to share qualitative data at ICPSR. This guide provides an overview of elements and considerations for archiving qualitative data, identifies steps for investigators to follow during the research life cycle to ensure that others can share and reuse qualitative data, and provides information about exemplars of qualitative data
International Projects:
- Research Compliance Program for FAS/SEAS at Harvard The Faculty of Arts and Sciences (FAS), including the School of Engineering and Applied Sciences (SEAS), and the Office of the Vice Provost for Research (OVPR) have established a shared Research Compliance Program (RCP). An area of common concern for interview studies is international projects and collaboration . RCP is a resource to provide guidance on which international activities may be impacted by US sanctions on countries, individuals, or entities and whether licenses or other disclosure are required to ship or otherwise share items, technology, or data with foreign collaborators.
Finding Extant Interview Data
Finding journalistic interviews: .
- Academic Search Premier This all-purpose database is great for finding articles from magazines and newspapers. In the Advanced Search, it allows you to specify "Document Type": Interview.
- Guide to Newspapers and Newspaper Indexes Use this guide created to Harvard Librarians to identify newspapers collections you'd like to search. To locate interviews, try adding the term "interview" to your search, or explore a database's search interface for options to limit your search to interviews. Nexis Uni and Factiva are the two main databases for current news.
- Listen Notes Search for podcast episodes at this podcast aggregator, and look for podcasts that include interviews. Make sure to vet the podcaster for accuracy and quality! (Listen Notes does not do much vetting.)
- NPR and ProPublica are two sites that offer high-quality long-form reporting, including journalistic interviews, for free.
Finding Oral History and Social Research Interviews:
- To find oral histories, see the Oral History page of this guide for helpful resources on Oral History interviewing.
- Repositories for Qualitative Data It has not been a customary practice among qualitative researchers in the social sciences to share raw interview data, but some have made this data available in repositories, such as the ones listed on the page linked above. You may find published data from structured interview surveys (e.g., questionnaire-based computer-assisted telephone interview data), as well as some semi-structured and unstructured interviews.
- If you are merely interested in studies interpreting data collected using interviews, rather than finding raw interview data, try databases like PsycInfo , Sociological Abstracts , or Anthropology Plus , among others.
Finding Interviews in Archival Collections at Harvard Library:
In addition to the databases and search strategies mentioned under the "Finding Oral History and Social Research Interviews" category above, you may search for interviews and oral histories (whether in textual or audiovisual formats) held in archival collections at Harvard Library.
- HOLLIS searches all documented collections at Harvard, whereas HOLLIS for Archival Discovery searches only those with finding aids. Although HOLLIS for Archival Discovery covers less material, you may find it easier to parse your search results, especially when you wish to view results at the item level (within collections). Try these approaches:
Search in HOLLIS :
- To retrieve items available online, do an Advanced Search for interview* OR "oral histor*" (in Subject), with Resource Type "Archives/Manuscripts," then refine your search by selecting "Online" under "Show Only" on the right of your initial result list. Revise the search above by adding your topic in the Keywords or Subject field (for example: African Americans ) and resubmitting the search.
- To enlarge your results set, you may also leave out the "Online" refinement; if you'd like to limit your search to a specific repository, try the technique of searching for Code: Library + Collection on the "Advanced Search" page .
Search in HOLLIS for Archival Discovery :
- To retrieve items available online, search for interview* OR "oral histor*" limited to digital materials . Revise the search above by adding your topic (for example: artist* ) in the second search box (if you don't see the box, click +).
- To preview results by collection, search for interview* OR "oral histor*" limited to collections . Revise the search above by adding your topic (for example: artist* ) in the second search box (if you don't see the box, click +). Although this method does not allow you to isolate digitized content, you may find the refinement options on the right side of the screen (refine by repository, subject or names) helpful. Once your select a given collection, you may search within it (e.g., for your topic or the term interview).
UX & MARKET RESEARCH INTERVIEWS
Ux at harvard library .
- User Experience and Market Research interviews can inform the design of tangible products and services through responsive, outcome-driven insights. The User Research Center at Harvard Library specializes in this kind of user-centered design, digital accessibility, and testing. They also offer guidance and resources to members of the Harvard Community who are interested in learning more about UX methods. Contact [email protected] or consult the URC website for more information.
Websites
- User Interviews: The Beginner’s Guide (Chris Mears)
- Interviewing Users (Jakob Nielsen)
Books
- Interviewing Users: How to Uncover Compelling Insights by Steve Portigal; Grant McCracken (Foreword by) Interviewing is a foundational user research tool that people assume they already possess. Everyone can ask questions, right? Unfortunately, that's not the case. Interviewing Users provides invaluable interviewing techniques and tools that enable you to conduct informative interviews with anyone. You'll move from simply gathering data to uncovering powerful insights about people.
- Rapid Contextual Design by Jessamyn Wendell; Karen Holtzblatt; Shelley Wood This handbook introduces Rapid CD, a fast-paced, adaptive form of Contextual Design. Rapid CD is a hands-on guide for anyone who needs practical guidance on how to use the Contextual Design process and adapt it to tactical projects with tight timelines and resources. Rapid Contextual Design provides detailed suggestions on structuring the project and customer interviews, conducting interviews, and running interpretation sessions. The handbook walks you step-by-step through organizing the data so you can see your key issues, along with visioning new solutions, storyboarding to work out the details, and paper prototype interviewing to iterate the design all with as little as a two-person team with only a few weeks to spare *Includes real project examples with actual customer data that illustrate how a CD project actually works.
Videos

Instructional Presentations on Interview Skills
- Interview/Oral History Research for RSRA 298B: Master's Thesis Reading and Research (Spring 2023) Slideshow covers: Why Interviews?, Getting Context, Engaging Participants, Conducting the Interview, The Interview Guide, Note Taking, Transcription, File management, and Data Analysis.
- Interview Skills From an online class on February 13, 2023: Get set up for interview research. You will leave prepared to choose among the three types of interviewing methods, equipped to develop an interview schedule, aware of data management options and their ethical implications, and knowledgeable of technologies you can use to record and transcribe your interviews. This workshop complements Intro to NVivo, a qualitative data analysis tool useful for coding interview data.
NIH Data Management & Sharing Policy (DMSP) This policy, effective January 25, 2023, applies to all research, funded or conducted in whole or in part by NIH, that results in the generation of scientific data , including NIH-funded qualitative research. Click here to see some examples of how the DMSP policy has been applied in qualitative research studies featured in the 2021 Qualitative Data Management Plan (DMP) Competition . As a resource for the community, NIH has developed a resource for developing informed consent language in research studies where data and/or biospecimens will be stored and shared for future use. It is important to note that the DMS Policy does NOT require that informed consent obtained from research participants must allow for broad sharing and the future use of data (either with or without identifiable private information). See the FAQ for more information.
- << Previous: Remote Research & Virtual Fieldwork
- Next: Oral History >>
Except where otherwise noted, this work is subject to a Creative Commons Attribution 4.0 International License , which allows anyone to share and adapt our material as long as proper attribution is given. For details and exceptions, see the Harvard Library Copyright Policy ©2021 Presidents and Fellows of Harvard College.
Qualitative Interviewing
- Reference work entry
- First Online: 13 January 2019
- Cite this reference work entry

- Sally Nathan 2 ,
- Christy Newman 3 &
- Kari Lancaster 3
4382 Accesses
20 Citations
8 Altmetric
Qualitative interviewing is a foundational method in qualitative research and is widely used in health research and the social sciences. Both qualitative semi-structured and in-depth unstructured interviews use verbal communication, mostly in face-to-face interactions, to collect data about the attitudes, beliefs, and experiences of participants. Interviews are an accessible, often affordable, and effective method to understand the socially situated world of research participants. The approach is typically informed by an interpretive framework where the data collected is not viewed as evidence of the truth or reality of a situation or experience but rather a context-bound subjective insight from the participants. The researcher needs to be open to new insights and to privilege the participant’s experience in data collection. The data from qualitative interviews is not generalizable, but its exploratory nature permits the collection of rich data which can answer questions about which little is already known. This chapter introduces the reader to qualitative interviewing, the range of traditions within which interviewing is utilized as a method, and highlights the advantages and some of the challenges and misconceptions in its application. The chapter also provides practical guidance on planning and conducting interview studies. Three case examples are presented to highlight the benefits and risks in the use of interviewing with different participants, providing situated insights as well as advice about how to go about learning to interview if you are a novice.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Baez B. Confidentiality in qualitative research: reflections on secrets, power and agency. Qual Res. 2002;2(1):35–58. https://doi.org/10.1177/1468794102002001638 .
Article Google Scholar
Braun V, Clarke V. Successful qualitative research: a practical guide for beginners. London: Sage Publications; 2013.
Google Scholar
Braun V, Clarke V, Gray D. Collecting qualitative data: a practical guide to textual, media and virtual techniques. Cambridge: Cambridge University Press; 2017.
Book Google Scholar
Bryman A. Social research methods. 5th ed. Oxford: Oxford University Press; 2016.
Crotty M. The foundations of social research: meaning and perspective in the research process. Australia: Allen & Unwin; 1998.
Davies MB. Doing a successful research project: using qualitative or quantitative methods. New York: Palgrave MacMillan; 2007.
Dickson-Swift V, James EL, Liamputtong P. Undertaking sensitive research in the health and social sciences. Cambridge: Cambridge University Press; 2008.
Foster M, Nathan S, Ferry M. The experience of drug-dependent adolescents in a therapeutic community. Drug Alcohol Rev. 2010;29(5):531–9.
Gillham B. The research interview. London: Continuum; 2000.
Glaser B, Strauss A. The discovery of grounded theory: strategies for qualitative research. Chicago: Aldine Publishing Company; 1967.
Hesse-Biber SN, Leavy P. In-depth interview. In: The practice of qualitative research. 2nd ed. Thousand Oaks: Sage Publications; 2011. p. 119–47
Irvine A. Duration, dominance and depth in telephone and face-to-face interviews: a comparative exploration. Int J Qual Methods. 2011;10(3):202–20.
Johnson JM. In-depth interviewing. In: Gubrium JF, Holstein JA, editors. Handbook of interview research: context and method. Thousand Oaks: Sage Publications; 2001.
Kvale S. Interviews: an introduction to qualitative research interviewing. Thousand Oaks: Sage; 1996.
Kvale S. Doing interviews. London: Sage Publications; 2007.
Lancaster K. Confidentiality, anonymity and power relations in elite interviewing: conducting qualitative policy research in a politicised domain. Int J Soc Res Methodol. 2017;20(1):93–103. https://doi.org/10.1080/13645579.2015.1123555 .
Leavy P. Method meets art: arts-based research practice. New York: Guilford Publications; 2015.
Liamputtong P. Researching the vulnerable: a guide to sensitive research methods. Thousand Oaks: Sage Publications; 2007.
Liamputtong P. Qualitative research methods. 4th ed. South Melbourne: Oxford University Press; 2013.
Mays N, Pope C. Quality in qualitative health research. In: Pope C, Mays N, editors. Qualitative research in health care. London: BMJ Books; 2000. p. 89–102.
McLellan E, MacQueen KM, Neidig JL. Beyond the qualitative interview: data preparation and transcription. Field Methods. 2003;15(1):63–84. https://doi.org/10.1177/1525822x02239573 .
Minichiello V, Aroni R, Hays T. In-depth interviewing: principles, techniques, analysis. 3rd ed. Sydney: Pearson Education Australia; 2008.
Morris ZS. The truth about interviewing elites. Politics. 2009;29(3):209–17. https://doi.org/10.1111/j.1467-9256.2009.01357.x .
Nathan S, Foster M, Ferry M. Peer and sexual relationships in the experience of drug-dependent adolescents in a therapeutic community. Drug Alcohol Rev. 2011;30(4):419–27.
National Health and Medical Research Council. National statement on ethical conduct in human research. Canberra: Australian Government; 2007.
Neal S, McLaughlin E. Researching up? Interviews, emotionality and policy-making elites. J Soc Policy. 2009;38(04):689–707. https://doi.org/10.1017/S0047279409990018 .
O’Reilly M, Parker N. ‘Unsatisfactory saturation’: a critical exploration of the notion of saturated sample sizes in qualitative research. Qual Res. 2013;13(2):190–7. https://doi.org/10.1177/1468794112446106 .
Ostrander S. “Surely you're not in this just to be helpful”: access, rapport and interviews in three studies of elites. In: Hertz R, Imber J, editors. Studying elites using qualitative methods. Thousand Oaks: Sage Publications; 1995. p. 133–50.
Chapter Google Scholar
Patton M. Qualitative research & evaluation methods: integrating theory and practice. Thousand Oaks: Sage Publications; 2015.
Punch KF. Introduction to social research: quantitative and qualitative approaches. London: Sage; 2005.
Rhodes T, Bernays S, Houmoller K. Parents who use drugs: accounting for damage and its limitation. Soc Sci Med. 2010;71(8):1489–97. https://doi.org/10.1016/j.socscimed.2010.07.028 .
Riessman CK. Narrative analysis. London: Sage; 1993.
Ritchie J. Not everything can be reduced to numbers. In: Berglund C, editor. Health research. Melbourne: Oxford University Press; 2001. p. 149–73.
Rubin H, Rubin I. Qualitative interviewing: the art of hearing data. 2nd ed. Thousand Oaks: Sage Publications; 2012.
Serry T, Liamputtong P. The in-depth interviewing method in health. In: Liamputtong P, editor. Research methods in health: foundations for evidence-based practice. 3rd ed. South Melbourne: Oxford University Press; 2017. p. 67–83.
Silverman D. Doing qualitative research. 5th ed. London: Sage; 2017.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (coreq): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57. https://doi.org/10.1093/intqhc/mzm042 .
Download references
Author information
Authors and affiliations.
School of Public Health and Community Medicine, Faculty of Medicine, UNSW, Sydney, NSW, Australia
Sally Nathan
Centre for Social Research in Health, Faculty of Arts and Social Sciences, UNSW, Sydney, NSW, Australia
Christy Newman & Kari Lancaster
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Sally Nathan .
Editor information
Editors and affiliations.
School of Science and Health, Western Sydney University, Penrith, NSW, Australia
Pranee Liamputtong
Rights and permissions
Reprints and permissions
Copyright information
© 2019 Springer Nature Singapore Pte Ltd.
About this entry
Cite this entry.
Nathan, S., Newman, C., Lancaster, K. (2019). Qualitative Interviewing. In: Liamputtong, P. (eds) Handbook of Research Methods in Health Social Sciences. Springer, Singapore. https://doi.org/10.1007/978-981-10-5251-4_77
Download citation
DOI : https://doi.org/10.1007/978-981-10-5251-4_77
Published : 13 January 2019
Publisher Name : Springer, Singapore
Print ISBN : 978-981-10-5250-7
Online ISBN : 978-981-10-5251-4
eBook Packages : Social Sciences Reference Module Humanities and Social Sciences Reference Module Business, Economics and Social Sciences
Share this entry
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Qualitative Research 101: Interviewing
5 Common Mistakes To Avoid When Undertaking Interviews
By: David Phair (PhD) and Kerryn Warren (PhD) | March 2022
Undertaking interviews is potentially the most important step in the qualitative research process. If you don’t collect useful, useable data in your interviews, you’ll struggle through the rest of your dissertation or thesis. Having helped numerous students with their research over the years, we’ve noticed some common interviewing mistakes that first-time researchers make. In this post, we’ll discuss five costly interview-related mistakes and outline useful strategies to avoid making these.
Overview: 5 Interviewing Mistakes
- Not having a clear interview strategy /plan
- Not having good interview techniques /skills
- Not securing a suitable location and equipment
- Not having a basic risk management plan
- Not keeping your “ golden thread ” front of mind
1. Not having a clear interview strategy
The first common mistake that we’ll look at is that of starting the interviewing process without having first come up with a clear interview strategy or plan of action. While it’s natural to be keen to get started engaging with your interviewees, a lack of planning can result in a mess of data and inconsistency between interviews.
There are several design choices to decide on and plan for before you start interviewing anyone. Some of the most important questions you need to ask yourself before conducting interviews include:
- What are the guiding research aims and research questions of my study?
- Will I use a structured, semi-structured or unstructured interview approach?
- How will I record the interviews (audio or video)?
- Who will be interviewed and by whom ?
- What ethics and data law considerations do I need to adhere to?
- How will I analyze my data?
Let’s take a quick look at some of these.
The core objective of the interviewing process is to generate useful data that will help you address your overall research aims. Therefore, your interviews need to be conducted in a way that directly links to your research aims, objectives and research questions (i.e. your “golden thread”). This means that you need to carefully consider the questions you’ll ask to ensure that they align with and feed into your golden thread. If any question doesn’t align with this, you may want to consider scrapping it.
Another important design choice is whether you’ll use an unstructured, semi-structured or structured interview approach . For semi-structured interviews, you will have a list of questions that you plan to ask and these questions will be open-ended in nature. You’ll also allow the discussion to digress from the core question set if something interesting comes up. This means that the type of information generated might differ a fair amount between interviews.
Contrasted to this, a structured approach to interviews is more rigid, where a specific set of closed questions is developed and asked for each interviewee in exactly the same order. Closed questions have a limited set of answers, that are often single-word answers. Therefore, you need to think about what you’re trying to achieve with your research project (i.e. your research aims) and decided on which approach would be best suited in your case.
It is also important to plan ahead with regards to who will be interviewed and how. You need to think about how you will approach the possible interviewees to get their cooperation, who will conduct the interviews, when to conduct the interviews and how to record the interviews. For each of these decisions, it’s also essential to make sure that all ethical considerations and data protection laws are taken into account.
Finally, you should think through how you plan to analyze the data (i.e., your qualitative analysis method) generated by the interviews. Different types of analysis rely on different types of data, so you need to ensure you’re asking the right types of questions and correctly guiding your respondents.
Simply put, you need to have a plan of action regarding the specifics of your interview approach before you start collecting data. If not, you’ll end up drifting in your approach from interview to interview, which will result in inconsistent, unusable data.

2. Not having good interview technique
While you’re generally not expected to become you to be an expert interviewer for a dissertation or thesis, it is important to practice good interview technique and develop basic interviewing skills .
Let’s go through some basics that will help the process along.
Firstly, before the interview , make sure you know your interview questions well and have a clear idea of what you want from the interview. Naturally, the specificity of your questions will depend on whether you’re taking a structured, semi-structured or unstructured approach, but you still need a consistent starting point . Ideally, you should develop an interview guide beforehand (more on this later) that details your core question and links these to the research aims, objectives and research questions.
Before you undertake any interviews, it’s a good idea to do a few mock interviews with friends or family members. This will help you get comfortable with the interviewer role, prepare for potentially unexpected answers and give you a good idea of how long the interview will take to conduct. In the interviewing process, you’re likely to encounter two kinds of challenging interviewees ; the two-word respondent and the respondent who meanders and babbles. Therefore, you should prepare yourself for both and come up with a plan to respond to each in a way that will allow the interview to continue productively.
To begin the formal interview , provide the person you are interviewing with an overview of your research. This will help to calm their nerves (and yours) and contextualize the interaction. Ultimately, you want the interviewee to feel comfortable and be willing to be open and honest with you, so it’s useful to start in a more casual, relaxed fashion and allow them to ask any questions they may have. From there, you can ease them into the rest of the questions.
As the interview progresses , avoid asking leading questions (i.e., questions that assume something about the interviewee or their response). Make sure that you speak clearly and slowly , using plain language and being ready to paraphrase questions if the person you are interviewing misunderstands. Be particularly careful with interviewing English second language speakers to ensure that you’re both on the same page.
Engage with the interviewee by listening to them carefully and acknowledging that you are listening to them by smiling or nodding. Show them that you’re interested in what they’re saying and thank them for their openness as appropriate. This will also encourage your interviewee to respond openly.
Need a helping hand?
3. Not securing a suitable location and quality equipment
Where you conduct your interviews and the equipment you use to record them both play an important role in how the process unfolds. Therefore, you need to think carefully about each of these variables before you start interviewing.
Poor location: A bad location can result in the quality of your interviews being compromised, interrupted, or cancelled. If you are conducting physical interviews, you’ll need a location that is quiet, safe, and welcoming . It’s very important that your location of choice is not prone to interruptions (the workplace office is generally problematic, for example) and has suitable facilities (such as water, a bathroom, and snacks).
If you are conducting online interviews , you need to consider a few other factors. Importantly, you need to make sure that both you and your respondent have access to a good, stable internet connection and electricity. Always check before the time that both of you know how to use the relevant software and it’s accessible (sometimes meeting platforms are blocked by workplace policies or firewalls). It’s also good to have alternatives in place (such as WhatsApp, Zoom, or Teams) to cater for these types of issues.
Poor equipment: Using poor-quality recording equipment or using equipment incorrectly means that you will have trouble transcribing, coding, and analyzing your interviews. This can be a major issue , as some of your interview data may go completely to waste if not recorded well. So, make sure that you use good-quality recording equipment and that you know how to use it correctly.
To avoid issues, you should always conduct test recordings before every interview to ensure that you can use the relevant equipment properly. It’s also a good idea to spot check each recording afterwards, just to make sure it was recorded as planned. If your equipment uses batteries, be sure to always carry a spare set.

4. Not having a basic risk management plan
Many possible issues can arise during the interview process. Not planning for these issues can mean that you are left with compromised data that might not be useful to you. Therefore, it’s important to map out some sort of risk management plan ahead of time, considering the potential risks, how you’ll minimize their probability and how you’ll manage them if they materialize.
Common potential issues related to the actual interview include cancellations (people pulling out), delays (such as getting stuck in traffic), language and accent differences (especially in the case of poor internet connections), issues with internet connections and power supply. Other issues can also occur in the interview itself. For example, the interviewee could drift off-topic, or you might encounter an interviewee who does not say much at all.
You can prepare for these potential issues by considering possible worst-case scenarios and preparing a response for each scenario. For instance, it is important to plan a backup date just in case your interviewee cannot make it to the first meeting you scheduled with them. It’s also a good idea to factor in a 30-minute gap between your interviews for the instances where someone might be late, or an interview runs overtime for other reasons. Make sure that you also plan backup questions that could be used to bring a respondent back on topic if they start rambling, or questions to encourage those who are saying too little.
In general, it’s best practice to plan to conduct more interviews than you think you need (this is called oversampling ). Doing so will allow you some room for error if there are interviews that don’t go as planned, or if some interviewees withdraw. If you need 10 interviews, it is a good idea to plan for 15. Likely, a few will cancel , delay, or not produce useful data.

5. Not keeping your golden thread front of mind
We touched on this a little earlier, but it is a key point that should be central to your entire research process. You don’t want to end up with pages and pages of data after conducting your interviews and realize that it is not useful to your research aims . Your research aims, objectives and research questions – i.e., your golden thread – should influence every design decision and should guide the interview process at all times.
A useful way to avoid this mistake is by developing an interview guide before you begin interviewing your respondents. An interview guide is a document that contains all of your questions with notes on how each of the interview questions is linked to the research question(s) of your study. You can also include your research aims and objectives here for a more comprehensive linkage.
You can easily create an interview guide by drawing up a table with one column containing your core interview questions . Then add another column with your research questions , another with expectations that you may have in light of the relevant literature and another with backup or follow-up questions . As mentioned, you can also bring in your research aims and objectives to help you connect them all together. If you’d like, you can download a copy of our free interview guide here .
Recap: Qualitative Interview Mistakes
In this post, we’ve discussed 5 common costly mistakes that are easy to make in the process of planning and conducting qualitative interviews.
To recap, these include:
If you have any questions about these interviewing mistakes, drop a comment below. Alternatively, if you’re interested in getting 1-on-1 help with your thesis or dissertation , check out our dissertation coaching service or book a free initial consultation with one of our friendly Grad Coaches.

Psst... there’s more!
This post was based on one of our popular Research Bootcamps . If you're working on a research project, you'll definitely want to check this out ...
You Might Also Like:

Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Print Friendly
- University Libraries
- Research Guides
- Topic Guides
- Research Methods Guide
- Interview Research
Research Methods Guide: Interview Research
- Introduction
- Research Design & Method
- Survey Research
- Data Analysis
- Resources & Consultation
Tutorial Videos: Interview Method
Interview as a Method for Qualitative Research

Goals of Interview Research
- Preferences
- They help you explain, better understand, and explore research subjects' opinions, behavior, experiences, phenomenon, etc.
- Interview questions are usually open-ended questions so that in-depth information will be collected.
Mode of Data Collection
There are several types of interviews, including:
- Face-to-Face
- Online (e.g. Skype, Googlehangout, etc)
FAQ: Conducting Interview Research
What are the important steps involved in interviews?
- Think about who you will interview
- Think about what kind of information you want to obtain from interviews
- Think about why you want to pursue in-depth information around your research topic
- Introduce yourself and explain the aim of the interview
- Devise your questions so interviewees can help answer your research question
- Have a sequence to your questions / topics by grouping them in themes
- Make sure you can easily move back and forth between questions / topics
- Make sure your questions are clear and easy to understand
- Do not ask leading questions
- Do you want to bring a second interviewer with you?
- Do you want to bring a notetaker?
- Do you want to record interviews? If so, do you have time to transcribe interview recordings?
- Where will you interview people? Where is the setting with the least distraction?
- How long will each interview take?
- Do you need to address terms of confidentiality?
Do I have to choose either a survey or interviewing method?
No. In fact, many researchers use a mixed method - interviews can be useful as follow-up to certain respondents to surveys, e.g., to further investigate their responses.
Is training an interviewer important?
Yes, since the interviewer can control the quality of the result, training the interviewer becomes crucial. If more than one interviewers are involved in your study, it is important to have every interviewer understand the interviewing procedure and rehearse the interviewing process before beginning the formal study.
- << Previous: Survey Research
- Next: Data Analysis >>
- Last Updated: Aug 21, 2023 10:42 AM
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 05 October 2018
Interviews and focus groups in qualitative research: an update for the digital age
- P. Gill 1 &
- J. Baillie 2
British Dental Journal volume 225 , pages 668–672 ( 2018 ) Cite this article
29k Accesses
48 Citations
20 Altmetric
Metrics details
Highlights that qualitative research is used increasingly in dentistry. Interviews and focus groups remain the most common qualitative methods of data collection.
Suggests the advent of digital technologies has transformed how qualitative research can now be undertaken.
Suggests interviews and focus groups can offer significant, meaningful insight into participants' experiences, beliefs and perspectives, which can help to inform developments in dental practice.
Qualitative research is used increasingly in dentistry, due to its potential to provide meaningful, in-depth insights into participants' experiences, perspectives, beliefs and behaviours. These insights can subsequently help to inform developments in dental practice and further related research. The most common methods of data collection used in qualitative research are interviews and focus groups. While these are primarily conducted face-to-face, the ongoing evolution of digital technologies, such as video chat and online forums, has further transformed these methods of data collection. This paper therefore discusses interviews and focus groups in detail, outlines how they can be used in practice, how digital technologies can further inform the data collection process, and what these methods can offer dentistry.
You have full access to this article via your institution.
Similar content being viewed by others

Interviews in the social sciences

Professionalism in dentistry: deconstructing common terminology
A review of technical and quality assessment considerations of audio-visual and web-conferencing focus groups in qualitative health research, introduction.
Traditionally, research in dentistry has primarily been quantitative in nature. 1 However, in recent years, there has been a growing interest in qualitative research within the profession, due to its potential to further inform developments in practice, policy, education and training. Consequently, in 2008, the British Dental Journal (BDJ) published a four paper qualitative research series, 2 , 3 , 4 , 5 to help increase awareness and understanding of this particular methodological approach.
Since the papers were originally published, two scoping reviews have demonstrated the ongoing proliferation in the use of qualitative research within the field of oral healthcare. 1 , 6 To date, the original four paper series continue to be well cited and two of the main papers remain widely accessed among the BDJ readership. 2 , 3 The potential value of well-conducted qualitative research to evidence-based practice is now also widely recognised by service providers, policy makers, funding bodies and those who commission, support and use healthcare research.
Besides increasing standalone use, qualitative methods are now also routinely incorporated into larger mixed method study designs, such as clinical trials, as they can offer additional, meaningful insights into complex problems that simply could not be provided by quantitative methods alone. Qualitative methods can also be used to further facilitate in-depth understanding of important aspects of clinical trial processes, such as recruitment. For example, Ellis et al . investigated why edentulous older patients, dissatisfied with conventional dentures, decline implant treatment, despite its established efficacy, and frequently refuse to participate in related randomised clinical trials, even when financial constraints are removed. 7 Through the use of focus groups in Canada and the UK, the authors found that fears of pain and potential complications, along with perceived embarrassment, exacerbated by age, are common reasons why older patients typically refuse dental implants. 7
The last decade has also seen further developments in qualitative research, due to the ongoing evolution of digital technologies. These developments have transformed how researchers can access and share information, communicate and collaborate, recruit and engage participants, collect and analyse data and disseminate and translate research findings. 8 Where appropriate, such technologies are therefore capable of extending and enhancing how qualitative research is undertaken. 9 For example, it is now possible to collect qualitative data via instant messaging, email or online/video chat, using appropriate online platforms.
These innovative approaches to research are therefore cost-effective, convenient, reduce geographical constraints and are often useful for accessing 'hard to reach' participants (for example, those who are immobile or socially isolated). 8 , 9 However, digital technologies are still relatively new and constantly evolving and therefore present a variety of pragmatic and methodological challenges. Furthermore, given their very nature, their use in many qualitative studies and/or with certain participant groups may be inappropriate and should therefore always be carefully considered. While it is beyond the scope of this paper to provide a detailed explication regarding the use of digital technologies in qualitative research, insight is provided into how such technologies can be used to facilitate the data collection process in interviews and focus groups.
In light of such developments, it is perhaps therefore timely to update the main paper 3 of the original BDJ series. As with the previous publications, this paper has been purposely written in an accessible style, to enhance readability, particularly for those who are new to qualitative research. While the focus remains on the most common qualitative methods of data collection – interviews and focus groups – appropriate revisions have been made to provide a novel perspective, and should therefore be helpful to those who would like to know more about qualitative research. This paper specifically focuses on undertaking qualitative research with adult participants only.
Overview of qualitative research
Qualitative research is an approach that focuses on people and their experiences, behaviours and opinions. 10 , 11 The qualitative researcher seeks to answer questions of 'how' and 'why', providing detailed insight and understanding, 11 which quantitative methods cannot reach. 12 Within qualitative research, there are distinct methodologies influencing how the researcher approaches the research question, data collection and data analysis. 13 For example, phenomenological studies focus on the lived experience of individuals, explored through their description of the phenomenon. Ethnographic studies explore the culture of a group and typically involve the use of multiple methods to uncover the issues. 14
While methodology is the 'thinking tool', the methods are the 'doing tools'; 13 the ways in which data are collected and analysed. There are multiple qualitative data collection methods, including interviews, focus groups, observations, documentary analysis, participant diaries, photography and videography. Two of the most commonly used qualitative methods are interviews and focus groups, which are explored in this article. The data generated through these methods can be analysed in one of many ways, according to the methodological approach chosen. A common approach is thematic data analysis, involving the identification of themes and subthemes across the data set. Further information on approaches to qualitative data analysis has been discussed elsewhere. 1
Qualitative research is an evolving and adaptable approach, used by different disciplines for different purposes. Traditionally, qualitative data, specifically interviews, focus groups and observations, have been collected face-to-face with participants. In more recent years, digital technologies have contributed to the ongoing evolution of qualitative research. Digital technologies offer researchers different ways of recruiting participants and collecting data, and offer participants opportunities to be involved in research that is not necessarily face-to-face.
Research interviews are a fundamental qualitative research method 15 and are utilised across methodological approaches. Interviews enable the researcher to learn in depth about the perspectives, experiences, beliefs and motivations of the participant. 3 , 16 Examples include, exploring patients' perspectives of fear/anxiety triggers in dental treatment, 17 patients' experiences of oral health and diabetes, 18 and dental students' motivations for their choice of career. 19
Interviews may be structured, semi-structured or unstructured, 3 according to the purpose of the study, with less structured interviews facilitating a more in depth and flexible interviewing approach. 20 Structured interviews are similar to verbal questionnaires and are used if the researcher requires clarification on a topic; however they produce less in-depth data about a participant's experience. 3 Unstructured interviews may be used when little is known about a topic and involves the researcher asking an opening question; 3 the participant then leads the discussion. 20 Semi-structured interviews are commonly used in healthcare research, enabling the researcher to ask predetermined questions, 20 while ensuring the participant discusses issues they feel are important.
Interviews can be undertaken face-to-face or using digital methods when the researcher and participant are in different locations. Audio-recording the interview, with the consent of the participant, is essential for all interviews regardless of the medium as it enables accurate transcription; the process of turning the audio file into a word-for-word transcript. This transcript is the data, which the researcher then analyses according to the chosen approach.
Types of interview
Qualitative studies often utilise one-to-one, face-to-face interviews with research participants. This involves arranging a mutually convenient time and place to meet the participant, signing a consent form and audio-recording the interview. However, digital technologies have expanded the potential for interviews in research, enabling individuals to participate in qualitative research regardless of location.
Telephone interviews can be a useful alternative to face-to-face interviews and are commonly used in qualitative research. They enable participants from different geographical areas to participate and may be less onerous for participants than meeting a researcher in person. 15 A qualitative study explored patients' perspectives of dental implants and utilised telephone interviews due to the quality of the data that could be yielded. 21 The researcher needs to consider how they will audio record the interview, which can be facilitated by purchasing a recorder that connects directly to the telephone. One potential disadvantage of telephone interviews is the inability of the interviewer and researcher to see each other. This is resolved using software for audio and video calls online – such as Skype – to conduct interviews with participants in qualitative studies. Advantages of this approach include being able to see the participant if video calls are used, enabling observation of non-verbal communication, and the software can be free to use. However, participants are required to have a device and internet connection, as well as being computer literate, potentially limiting who can participate in the study. One qualitative study explored the role of dental hygienists in reducing oral health disparities in Canada. 22 The researcher conducted interviews using Skype, which enabled dental hygienists from across Canada to be interviewed within the research budget, accommodating the participants' schedules. 22
A less commonly used approach to qualitative interviews is the use of social virtual worlds. A qualitative study accessed a social virtual world – Second Life – to explore the health literacy skills of individuals who use social virtual worlds to access health information. 23 The researcher created an avatar and interview room, and undertook interviews with participants using voice and text methods. 23 This approach to recruitment and data collection enables individuals from diverse geographical locations to participate, while remaining anonymous if they wish. Furthermore, for interviews conducted using text methods, transcription of the interview is not required as the researcher can save the written conversation with the participant, with the participant's consent. However, the researcher and participant need to be familiar with how the social virtual world works to engage in an interview this way.
Conducting an interview
Ensuring informed consent before any interview is a fundamental aspect of the research process. Participants in research must be afforded autonomy and respect; consent should be informed and voluntary. 24 Individuals should have the opportunity to read an information sheet about the study, ask questions, understand how their data will be stored and used, and know that they are free to withdraw at any point without reprisal. The qualitative researcher should take written consent before undertaking the interview. In a face-to-face interview, this is straightforward: the researcher and participant both sign copies of the consent form, keeping one each. However, this approach is less straightforward when the researcher and participant do not meet in person. A recent protocol paper outlined an approach for taking consent for telephone interviews, which involved: audio recording the participant agreeing to each point on the consent form; the researcher signing the consent form and keeping a copy; and posting a copy to the participant. 25 This process could be replicated in other interview studies using digital methods.
There are advantages and disadvantages of using face-to-face and digital methods for research interviews. Ultimately, for both approaches, the quality of the interview is determined by the researcher. 16 Appropriate training and preparation are thus required. Healthcare professionals can use their interpersonal communication skills when undertaking a research interview, particularly questioning, listening and conversing. 3 However, the purpose of an interview is to gain information about the study topic, 26 rather than offering help and advice. 3 The researcher therefore needs to listen attentively to participants, enabling them to describe their experience without interruption. 3 The use of active listening skills also help to facilitate the interview. 14 Spradley outlined elements and strategies for research interviews, 27 which are a useful guide for qualitative researchers:
Greeting and explaining the project/interview
Asking descriptive (broad), structural (explore response to descriptive) and contrast (difference between) questions
Asymmetry between the researcher and participant talking
Expressing interest and cultural ignorance
Repeating, restating and incorporating the participant's words when asking questions
Creating hypothetical situations
Asking friendly questions
Knowing when to leave.
For semi-structured interviews, a topic guide (also called an interview schedule) is used to guide the content of the interview – an example of a topic guide is outlined in Box 1 . The topic guide, usually based on the research questions, existing literature and, for healthcare professionals, their clinical experience, is developed by the research team. The topic guide should include open ended questions that elicit in-depth information, and offer participants the opportunity to talk about issues important to them. This is vital in qualitative research where the researcher is interested in exploring the experiences and perspectives of participants. It can be useful for qualitative researchers to pilot the topic guide with the first participants, 10 to ensure the questions are relevant and understandable, and amending the questions if required.
Regardless of the medium of interview, the researcher must consider the setting of the interview. For face-to-face interviews, this could be in the participant's home, in an office or another mutually convenient location. A quiet location is preferable to promote confidentiality, enable the researcher and participant to concentrate on the conversation, and to facilitate accurate audio-recording of the interview. For interviews using digital methods the same principles apply: a quiet, private space where the researcher and participant feel comfortable and confident to participate in an interview.
Box 1: Example of a topic guide
Study focus: Parents' experiences of brushing their child's (aged 0–5) teeth
1. Can you tell me about your experience of cleaning your child's teeth?
How old was your child when you started cleaning their teeth?
Why did you start cleaning their teeth at that point?
How often do you brush their teeth?
What do you use to brush their teeth and why?
2. Could you explain how you find cleaning your child's teeth?
Do you find anything difficult?
What makes cleaning their teeth easier for you?
3. How has your experience of cleaning your child's teeth changed over time?
Has it become easier or harder?
Have you changed how often and how you clean their teeth? If so, why?
4. Could you describe how your child finds having their teeth cleaned?
What do they enjoy about having their teeth cleaned?
Is there anything they find upsetting about having their teeth cleaned?
5. Where do you look for information/advice about cleaning your child's teeth?
What did your health visitor tell you about cleaning your child's teeth? (If anything)
What has the dentist told you about caring for your child's teeth? (If visited)
Have any family members given you advice about how to clean your child's teeth? If so, what did they tell you? Did you follow their advice?
6. Is there anything else you would like to discuss about this?
Focus groups
A focus group is a moderated group discussion on a pre-defined topic, for research purposes. 28 , 29 While not aligned to a particular qualitative methodology (for example, grounded theory or phenomenology) as such, focus groups are used increasingly in healthcare research, as they are useful for exploring collective perspectives, attitudes, behaviours and experiences. Consequently, they can yield rich, in-depth data and illuminate agreement and inconsistencies 28 within and, where appropriate, between groups. Examples include public perceptions of dental implants and subsequent impact on help-seeking and decision making, 30 and general dental practitioners' views on patient safety in dentistry. 31
Focus groups can be used alone or in conjunction with other methods, such as interviews or observations, and can therefore help to confirm, extend or enrich understanding and provide alternative insights. 28 The social interaction between participants often results in lively discussion and can therefore facilitate the collection of rich, meaningful data. However, they are complex to organise and manage, due to the number of participants, and may also be inappropriate for exploring particularly sensitive issues that many participants may feel uncomfortable about discussing in a group environment.
Focus groups are primarily undertaken face-to-face but can now also be undertaken online, using appropriate technologies such as email, bulletin boards, online research communities, chat rooms, discussion forums, social media and video conferencing. 32 Using such technologies, data collection can also be synchronous (for example, online discussions in 'real time') or, unlike traditional face-to-face focus groups, asynchronous (for example, online/email discussions in 'non-real time'). While many of the fundamental principles of focus group research are the same, regardless of how they are conducted, a number of subtle nuances are associated with the online medium. 32 Some of which are discussed further in the following sections.
Focus group considerations
Some key considerations associated with face-to-face focus groups are: how many participants are required; should participants within each group know each other (or not) and how many focus groups are needed within a single study? These issues are much debated and there is no definitive answer. However, the number of focus groups required will largely depend on the topic area, the depth and breadth of data needed, the desired level of participation required 29 and the necessity (or not) for data saturation.
The optimum group size is around six to eight participants (excluding researchers) but can work effectively with between three and 14 participants. 3 If the group is too small, it may limit discussion, but if it is too large, it may become disorganised and difficult to manage. It is, however, prudent to over-recruit for a focus group by approximately two to three participants, to allow for potential non-attenders. For many researchers, particularly novice researchers, group size may also be informed by pragmatic considerations, such as the type of study, resources available and moderator experience. 28 Similar size and mix considerations exist for online focus groups. Typically, synchronous online focus groups will have around three to eight participants but, as the discussion does not happen simultaneously, asynchronous groups may have as many as 10–30 participants. 33
The topic area and potential group interaction should guide group composition considerations. Pre-existing groups, where participants know each other (for example, work colleagues) may be easier to recruit, have shared experiences and may enjoy a familiarity, which facilitates discussion and/or the ability to challenge each other courteously. 3 However, if there is a potential power imbalance within the group or if existing group norms and hierarchies may adversely affect the ability of participants to speak freely, then 'stranger groups' (that is, where participants do not already know each other) may be more appropriate. 34 , 35
Focus group management
Face-to-face focus groups should normally be conducted by two researchers; a moderator and an observer. 28 The moderator facilitates group discussion, while the observer typically monitors group dynamics, behaviours, non-verbal cues, seating arrangements and speaking order, which is essential for transcription and analysis. The same principles of informed consent, as discussed in the interview section, also apply to focus groups, regardless of medium. However, the consent process for online discussions will probably be managed somewhat differently. For example, while an appropriate participant information leaflet (and consent form) would still be required, the process is likely to be managed electronically (for example, via email) and would need to specifically address issues relating to technology (for example, anonymity and use, storage and access to online data). 32
The venue in which a face to face focus group is conducted should be of a suitable size, private, quiet, free from distractions and in a collectively convenient location. It should also be conducted at a time appropriate for participants, 28 as this is likely to promote attendance. As with interviews, the same ethical considerations apply (as discussed earlier). However, online focus groups may present additional ethical challenges associated with issues such as informed consent, appropriate access and secure data storage. Further guidance can be found elsewhere. 8 , 32
Before the focus group commences, the researchers should establish rapport with participants, as this will help to put them at ease and result in a more meaningful discussion. Consequently, researchers should introduce themselves, provide further clarity about the study and how the process will work in practice and outline the 'ground rules'. Ground rules are designed to assist, not hinder, group discussion and typically include: 3 , 28 , 29
Discussions within the group are confidential to the group
Only one person can speak at a time
All participants should have sufficient opportunity to contribute
There should be no unnecessary interruptions while someone is speaking
Everyone can be expected to be listened to and their views respected
Challenging contrary opinions is appropriate, but ridiculing is not.
Moderating a focus group requires considered management and good interpersonal skills to help guide the discussion and, where appropriate, keep it sufficiently focused. Avoid, therefore, participating, leading, expressing personal opinions or correcting participants' knowledge 3 , 28 as this may bias the process. A relaxed, interested demeanour will also help participants to feel comfortable and promote candid discourse. Moderators should also prevent the discussion being dominated by any one person, ensure differences of opinions are discussed fairly and, if required, encourage reticent participants to contribute. 3 Asking open questions, reflecting on significant issues, inviting further debate, probing responses accordingly, and seeking further clarification, as and where appropriate, will help to obtain sufficient depth and insight into the topic area.
Moderating online focus groups requires comparable skills, particularly if the discussion is synchronous, as the discussion may be dominated by those who can type proficiently. 36 It is therefore important that sufficient time and respect is accorded to those who may not be able to type as quickly. Asynchronous discussions are usually less problematic in this respect, as interactions are less instant. However, moderating an asynchronous discussion presents additional challenges, particularly if participants are geographically dispersed, as they may be online at different times. Consequently, the moderator will not always be present and the discussion may therefore need to occur over several days, which can be difficult to manage and facilitate and invariably requires considerable flexibility. 32 It is also worth recognising that establishing rapport with participants via online medium is often more challenging than via face-to-face and may therefore require additional time, skills, effort and consideration.
As with research interviews, focus groups should be guided by an appropriate interview schedule, as discussed earlier in the paper. For example, the schedule will usually be informed by the review of the literature and study aims, and will merely provide a topic guide to help inform subsequent discussions. To provide a verbatim account of the discussion, focus groups must be recorded, using an audio-recorder with a good quality multi-directional microphone. While videotaping is possible, some participants may find it obtrusive, 3 which may adversely affect group dynamics. The use (or not) of a video recorder, should therefore be carefully considered.
At the end of the focus group, a few minutes should be spent rounding up and reflecting on the discussion. 28 Depending on the topic area, it is possible that some participants may have revealed deeply personal issues and may therefore require further help and support, such as a constructive debrief or possibly even referral on to a relevant third party. It is also possible that some participants may feel that the discussion did not adequately reflect their views and, consequently, may no longer wish to be associated with the study. 28 Such occurrences are likely to be uncommon, but should they arise, it is important to further discuss any concerns and, if appropriate, offer them the opportunity to withdraw (including any data relating to them) from the study. Immediately after the discussion, researchers should compile notes regarding thoughts and ideas about the focus group, which can assist with data analysis and, if appropriate, any further data collection.
Qualitative research is increasingly being utilised within dental research to explore the experiences, perspectives, motivations and beliefs of participants. The contributions of qualitative research to evidence-based practice are increasingly being recognised, both as standalone research and as part of larger mixed-method studies, including clinical trials. Interviews and focus groups remain commonly used data collection methods in qualitative research, and with the advent of digital technologies, their utilisation continues to evolve. However, digital methods of qualitative data collection present additional methodological, ethical and practical considerations, but also potentially offer considerable flexibility to participants and researchers. Consequently, regardless of format, qualitative methods have significant potential to inform important areas of dental practice, policy and further related research.
Gussy M, Dickson-Swift V, Adams J . A scoping review of qualitative research in peer-reviewed dental publications. Int J Dent Hygiene 2013; 11 : 174–179.
Article Google Scholar
Burnard P, Gill P, Stewart K, Treasure E, Chadwick B . Analysing and presenting qualitative data. Br Dent J 2008; 204 : 429–432.
Gill P, Stewart K, Treasure E, Chadwick B . Methods of data collection in qualitative research: interviews and focus groups. Br Dent J 2008; 204 : 291–295.
Gill P, Stewart K, Treasure E, Chadwick B . Conducting qualitative interviews with school children in dental research. Br Dent J 2008; 204 : 371–374.
Stewart K, Gill P, Chadwick B, Treasure E . Qualitative research in dentistry. Br Dent J 2008; 204 : 235–239.
Masood M, Thaliath E, Bower E, Newton J . An appraisal of the quality of published qualitative dental research. Community Dent Oral Epidemiol 2011; 39 : 193–203.
Ellis J, Levine A, Bedos C et al. Refusal of implant supported mandibular overdentures by elderly patients. Gerodontology 2011; 28 : 62–68.
Macfarlane S, Bucknall T . Digital Technologies in Research. In Gerrish K, Lathlean J (editors) The Research Process in Nursing . 7th edition. pp. 71–86. Oxford: Wiley Blackwell; 2015.
Google Scholar
Lee R, Fielding N, Blank G . Online Research Methods in the Social Sciences: An Editorial Introduction. In Fielding N, Lee R, Blank G (editors) The Sage Handbook of Online Research Methods . pp. 3–16. London: Sage Publications; 2016.
Creswell J . Qualitative inquiry and research design: Choosing among five designs . Thousand Oaks, CA: Sage, 1998.
Guest G, Namey E, Mitchell M . Qualitative research: Defining and designing In Guest G, Namey E, Mitchell M (editors) Collecting Qualitative Data: A Field Manual For Applied Research . pp. 1–40. London: Sage Publications, 2013.
Chapter Google Scholar
Pope C, Mays N . Qualitative research: Reaching the parts other methods cannot reach: an introduction to qualitative methods in health and health services research. BMJ 1995; 311 : 42–45.
Giddings L, Grant B . A Trojan Horse for positivism? A critique of mixed methods research. Adv Nurs Sci 2007; 30 : 52–60.
Hammersley M, Atkinson P . Ethnography: Principles in Practice . London: Routledge, 1995.
Oltmann S . Qualitative interviews: A methodological discussion of the interviewer and respondent contexts Forum Qualitative Sozialforschung/Forum: Qualitative Social Research. 2016; 17 : Art. 15.
Patton M . Qualitative Research and Evaluation Methods . Thousand Oaks, CA: Sage, 2002.
Wang M, Vinall-Collier K, Csikar J, Douglas G . A qualitative study of patients' views of techniques to reduce dental anxiety. J Dent 2017; 66 : 45–51.
Lindenmeyer A, Bowyer V, Roscoe J, Dale J, Sutcliffe P . Oral health awareness and care preferences in patients with diabetes: a qualitative study. Fam Pract 2013; 30 : 113–118.
Gallagher J, Clarke W, Wilson N . Understanding the motivation: a qualitative study of dental students' choice of professional career. Eur J Dent Educ 2008; 12 : 89–98.
Tod A . Interviewing. In Gerrish K, Lacey A (editors) The Research Process in Nursing . Oxford: Blackwell Publishing, 2006.
Grey E, Harcourt D, O'Sullivan D, Buchanan H, Kipatrick N . A qualitative study of patients' motivations and expectations for dental implants. Br Dent J 2013; 214 : 10.1038/sj.bdj.2012.1178.
Farmer J, Peressini S, Lawrence H . Exploring the role of the dental hygienist in reducing oral health disparities in Canada: A qualitative study. Int J Dent Hygiene 2017; 10.1111/idh.12276.
McElhinney E, Cheater F, Kidd L . Undertaking qualitative health research in social virtual worlds. J Adv Nurs 2013; 70 : 1267–1275.
Health Research Authority. UK Policy Framework for Health and Social Care Research. Available at https://www.hra.nhs.uk/planning-and-improving-research/policies-standards-legislation/uk-policy-framework-health-social-care-research/ (accessed September 2017).
Baillie J, Gill P, Courtenay P . Knowledge, understanding and experiences of peritonitis among patients, and their families, undertaking peritoneal dialysis: A mixed methods study protocol. J Adv Nurs 2017; 10.1111/jan.13400.
Kvale S . Interviews . Thousand Oaks (CA): Sage, 1996.
Spradley J . The Ethnographic Interview . New York: Holt, Rinehart and Winston, 1979.
Goodman C, Evans C . Focus Groups. In Gerrish K, Lathlean J (editors) The Research Process in Nursing . pp. 401–412. Oxford: Wiley Blackwell, 2015.
Shaha M, Wenzell J, Hill E . Planning and conducting focus group research with nurses. Nurse Res 2011; 18 : 77–87.
Wang G, Gao X, Edward C . Public perception of dental implants: a qualitative study. J Dent 2015; 43 : 798–805.
Bailey E . Contemporary views of dental practitioners' on patient safety. Br Dent J 2015; 219 : 535–540.
Abrams K, Gaiser T . Online Focus Groups. In Field N, Lee R, Blank G (editors) The Sage Handbook of Online Research Methods . pp. 435–450. London: Sage Publications, 2016.
Poynter R . The Handbook of Online and Social Media Research . West Sussex: John Wiley & Sons, 2010.
Kevern J, Webb C . Focus groups as a tool for critical social research in nurse education. Nurse Educ Today 2001; 21 : 323–333.
Kitzinger J, Barbour R . Introduction: The Challenge and Promise of Focus Groups. In Barbour R S K J (editor) Developing Focus Group Research . pp. 1–20. London: Sage Publications, 1999.
Krueger R, Casey M . Focus Groups: A Practical Guide for Applied Research. 4th ed. Thousand Oaks, California: SAGE; 2009.
Download references
Author information
Authors and affiliations.
Senior Lecturer (Adult Nursing), School of Healthcare Sciences, Cardiff University,
Lecturer (Adult Nursing) and RCBC Wales Postdoctoral Research Fellow, School of Healthcare Sciences, Cardiff University,
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to P. Gill .
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Gill, P., Baillie, J. Interviews and focus groups in qualitative research: an update for the digital age. Br Dent J 225 , 668–672 (2018). https://doi.org/10.1038/sj.bdj.2018.815
Download citation
Accepted : 02 July 2018
Published : 05 October 2018
Issue Date : 12 October 2018
DOI : https://doi.org/10.1038/sj.bdj.2018.815
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Translating brand reputation into equity from the stakeholder’s theory: an approach to value creation based on consumer’s perception & interactions.
- Olukorede Adewole
International Journal of Corporate Social Responsibility (2024)
Perceptions and beliefs of community gatekeepers about genomic risk information in African cleft research
- Abimbola M. Oladayo
- Oluwakemi Odukoya
- Azeez Butali
BMC Public Health (2024)
Assessment of women’s needs, wishes and preferences regarding interprofessional guidance on nutrition in pregnancy – a qualitative study
- Merle Ebinghaus
- Caroline Johanna Agricola
- Birgit-Christiane Zyriax
BMC Pregnancy and Childbirth (2024)
‘Baby mamas’ in Urban Ghana: an exploratory qualitative study on the factors influencing serial fathering among men in Accra, Ghana
- Rosemond Akpene Hiadzi
- Jemima Akweley Agyeman
- Godwin Banafo Akrong
Reproductive Health (2023)
Revolutionising dental technologies: a qualitative study on dental technicians’ perceptions of Artificial intelligence integration
- Galvin Sim Siang Lin
- Yook Shiang Ng
- Kah Hoay Chua
BMC Oral Health (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Qualitative Research : Definition
Qualitative research is the naturalistic study of social meanings and processes, using interviews, observations, and the analysis of texts and images. In contrast to quantitative researchers, whose statistical methods enable broad generalizations about populations (for example, comparisons of the percentages of U.S. demographic groups who vote in particular ways), qualitative researchers use in-depth studies of the social world to analyze how and why groups think and act in particular ways (for instance, case studies of the experiences that shape political views).
Events and Workshops
- Introduction to NVivo Have you just collected your data and wondered what to do next? Come join us for an introductory session on utilizing NVivo to support your analytical process. This session will only cover features of the software and how to import your records. Please feel free to attend any of the following sessions below: April 25th, 2024 12:30 pm - 1:45 pm Green Library - SVA Conference Room 125 May 9th, 2024 12:30 pm - 1:45 pm Green Library - SVA Conference Room 125
- Next: Choose an approach >>
- Choose an approach
- Find studies
- Learn methods
- Getting Started
- Get software
- Get data for secondary analysis
- Network with researchers

- Last Updated: May 23, 2024 1:27 PM
- URL: https://guides.library.stanford.edu/qualitative_research
Root out friction in every digital experience, super-charge conversion rates, and optimize digital self-service
Uncover insights from any interaction, deliver AI-powered agent coaching, and reduce cost to serve
Increase revenue and loyalty with real-time insights and recommendations delivered to teams on the ground
Know how your people feel and empower managers to improve employee engagement, productivity, and retention
Take action in the moments that matter most along the employee journey and drive bottom line growth
Whatever they’re are saying, wherever they’re saying it, know exactly what’s going on with your people
Get faster, richer insights with qual and quant tools that make powerful market research available to everyone
Run concept tests, pricing studies, prototyping + more with fast, powerful studies designed by UX research experts
Track your brand performance 24/7 and act quickly to respond to opportunities and challenges in your market
Explore the platform powering Experience Management
- Free Account
- For Digital
- For Customer Care
- For Human Resources
- For Researchers
- Financial Services
- All Industries
Popular Use Cases
- Customer Experience
- Employee Experience
- Net Promoter Score
- Voice of Customer
- Customer Success Hub
- Product Documentation
- Training & Certification
- XM Institute
- Popular Resources
- Customer Stories
- Artificial Intelligence
Market Research
- Partnerships
- Marketplace
The annual gathering of the experience leaders at the world’s iconic brands building breakthrough business results, live in Salt Lake City.
- English/AU & NZ
- Español/Europa
- Español/América Latina
- Português Brasileiro
- REQUEST DEMO
- Experience Management
- Qualitative Research Interviews
Try Qualtrics for free
How to carry out great interviews in qualitative research.
11 min read An interview is one of the most versatile methods used in qualitative research. Here’s what you need to know about conducting great qualitative interviews.

What is a qualitative research interview?
Qualitative research interviews are a mainstay among q ualitative research techniques, and have been in use for decades either as a primary data collection method or as an adjunct to a wider research process. A qualitative research interview is a one-to-one data collection session between a researcher and a participant. Interviews may be carried out face-to-face, over the phone or via video call using a service like Skype or Zoom.
There are three main types of qualitative research interview – structured, unstructured or semi-structured.
- Structured interviews Structured interviews are based around a schedule of predetermined questions and talking points that the researcher has developed. At their most rigid, structured interviews may have a precise wording and question order, meaning that they can be replicated across many different interviewers and participants with relatively consistent results.
- Unstructured interviews Unstructured interviews have no predetermined format, although that doesn’t mean they’re ad hoc or unplanned. An unstructured interview may outwardly resemble a normal conversation, but the interviewer will in fact be working carefully to make sure the right topics are addressed during the interaction while putting the participant at ease with a natural manner.
- Semi-structured interviews Semi-structured interviews are the most common type of qualitative research interview, combining the informality and rapport of an unstructured interview with the consistency and replicability of a structured interview. The researcher will come prepared with questions and topics, but will not need to stick to precise wording. This blended approach can work well for in-depth interviews.
Free eBook: The qualitative research design handbook
What are the pros and cons of interviews in qualitative research?
As a qualitative research method interviewing is hard to beat, with applications in social research, market research, and even basic and clinical pharmacy. But like any aspect of the research process, it’s not without its limitations. Before choosing qualitative interviewing as your research method, it’s worth weighing up the pros and cons.
Pros of qualitative interviews:
- provide in-depth information and context
- can be used effectively when their are low numbers of participants
- provide an opportunity to discuss and explain questions
- useful for complex topics
- rich in data – in the case of in-person or video interviews , the researcher can observe body language and facial expression as well as the answers to questions
Cons of qualitative interviews:
- can be time-consuming to carry out
- costly when compared to some other research methods
- because of time and cost constraints, they often limit you to a small number of participants
- difficult to standardize your data across different researchers and participants unless the interviews are very tightly structured
- As the Open University of Hong Kong notes, qualitative interviews may take an emotional toll on interviewers
Qualitative interview guides
Semi-structured interviews are based on a qualitative interview guide, which acts as a road map for the researcher. While conducting interviews, the researcher can use the interview guide to help them stay focused on their research questions and make sure they cover all the topics they intend to.
An interview guide may include a list of questions written out in full, or it may be a set of bullet points grouped around particular topics. It can prompt the interviewer to dig deeper and ask probing questions during the interview if appropriate.
Consider writing out the project’s research question at the top of your interview guide, ahead of the interview questions. This may help you steer the interview in the right direction if it threatens to head off on a tangent.
Avoid bias in qualitative research interviews
According to Duke University , bias can create significant problems in your qualitative interview.
- Acquiescence bias is common to many qualitative methods, including focus groups. It occurs when the participant feels obliged to say what they think the researcher wants to hear. This can be especially problematic when there is a perceived power imbalance between participant and interviewer. To counteract this, Duke University’s experts recommend emphasizing the participant’s expertise in the subject being discussed, and the value of their contributions.
- Interviewer bias is when the interviewer’s own feelings about the topic come to light through hand gestures, facial expressions or turns of phrase. Duke’s recommendation is to stick to scripted phrases where this is an issue, and to make sure researchers become very familiar with the interview guide or script before conducting interviews, so that they can hone their delivery.
What kinds of questions should you ask in a qualitative interview?
The interview questions you ask need to be carefully considered both before and during the data collection process. As well as considering the topics you’ll cover, you will need to think carefully about the way you ask questions.
Open-ended interview questions – which cannot be answered with a ‘yes’ ‘no’ or ‘maybe’ – are recommended by many researchers as a way to pursue in depth information.
An example of an open-ended question is “What made you want to move to the East Coast?” This will prompt the participant to consider different factors and select at least one. Having thought about it carefully, they may give you more detailed information about their reasoning.
A closed-ended question , such as “Would you recommend your neighborhood to a friend?” can be answered without too much deliberation, and without giving much information about personal thoughts, opinions and feelings.
Follow-up questions can be used to delve deeper into the research topic and to get more detail from open-ended questions. Examples of follow-up questions include:
- What makes you say that?
- What do you mean by that?
- Can you tell me more about X?
- What did/does that mean to you?
As well as avoiding closed-ended questions, be wary of leading questions. As with other qualitative research techniques such as surveys or focus groups, these can introduce bias in your data. Leading questions presume a certain point of view shared by the interviewer and participant, and may even suggest a foregone conclusion.
An example of a leading question might be: “You moved to New York in 1990, didn’t you?” In answering the question, the participant is much more likely to agree than disagree. This may be down to acquiescence bias or a belief that the interviewer has checked the information and already knows the correct answer.
Other leading questions involve adjectival phrases or other wording that introduces negative or positive connotations about a particular topic. An example of this kind of leading question is: “Many employees dislike wearing masks to work. How do you feel about this?” It presumes a positive opinion and the participant may be swayed by it, or not want to contradict the interviewer.
Harvard University’s guidelines for qualitative interview research add that you shouldn’t be afraid to ask embarrassing questions – “if you don’t ask, they won’t tell.” Bear in mind though that too much probing around sensitive topics may cause the interview participant to withdraw. The Harvard guidelines recommend leaving sensitive questions til the later stages of the interview when a rapport has been established.
More tips for conducting qualitative interviews
Observing a participant’s body language can give you important data about their thoughts and feelings. It can also help you decide when to broach a topic, and whether to use a follow-up question or return to the subject later in the interview.
Be conscious that the participant may regard you as the expert, not themselves. In order to make sure they express their opinions openly, use active listening skills like verbal encouragement and paraphrasing and clarifying their meaning to show how much you value what they are saying.
Remember that part of the goal is to leave the interview participant feeling good about volunteering their time and their thought process to your research. Aim to make them feel empowered , respected and heard.
Unstructured interviews can demand a lot of a researcher, both cognitively and emotionally. Be sure to leave time in between in-depth interviews when scheduling your data collection to make sure you maintain the quality of your data, as well as your own well-being .
Recording and transcribing interviews
Historically, recording qualitative research interviews and then transcribing the conversation manually would have represented a significant part of the cost and time involved in research projects that collect qualitative data.
Fortunately, researchers now have access to digital recording tools, and even speech-to-text technology that can automatically transcribe interview data using AI and machine learning. This type of tool can also be used to capture qualitative data from qualitative research (focus groups,ect.) making this kind of social research or market research much less time consuming.
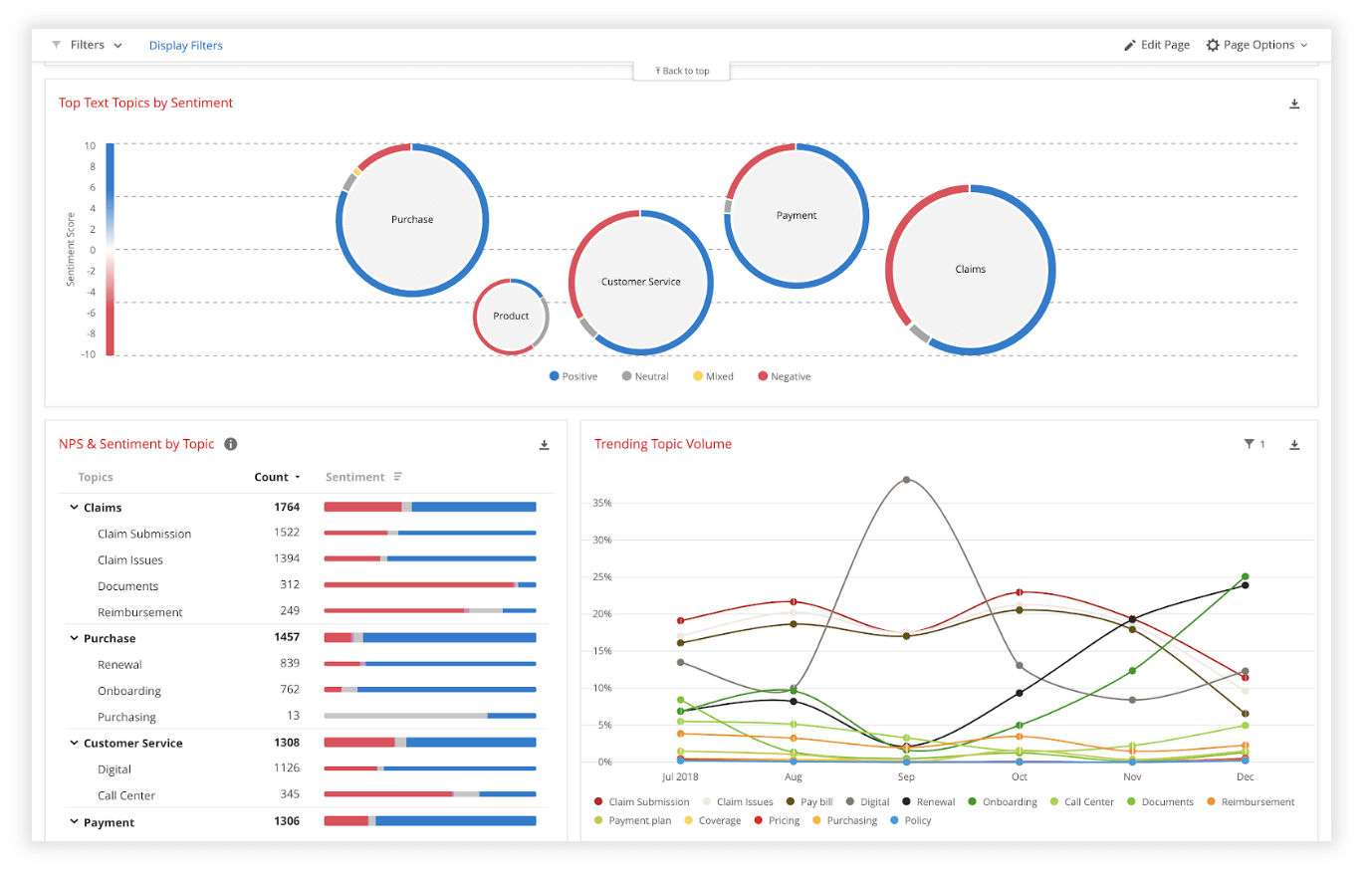
Data analysis
Qualitative interview data is unstructured, rich in content and difficult to analyze without the appropriate tools. Fortunately, machine learning and AI can once again make things faster and easier when you use qualitative methods like the research interview.
Text analysis tools and natural language processing software can ‘read’ your transcripts and voice data and identify patterns and trends across large volumes of text or speech. They can also perform khttps://www.qualtrics.com/experience-management/research/sentiment-analysis/
which assesses overall trends in opinion and provides an unbiased overall summary of how participants are feeling.
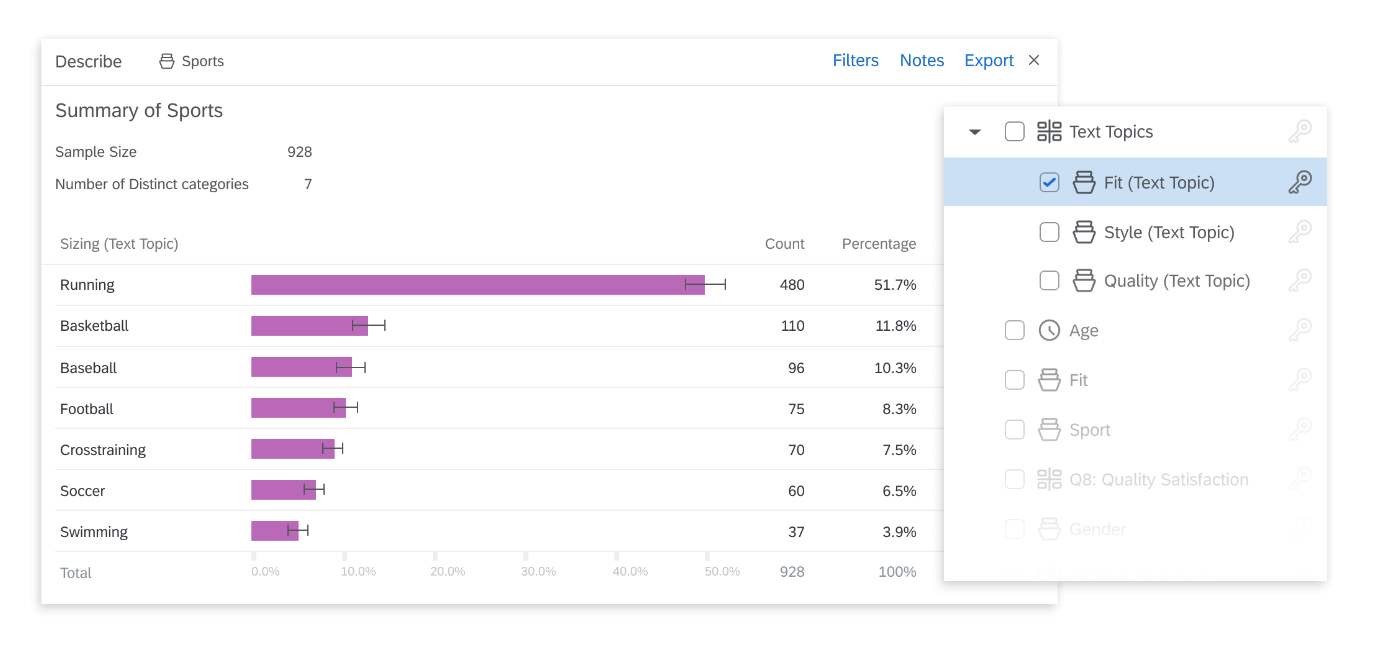
Another feature of text analysis tools is their ability to categorize information by topic, sorting it into groupings that help you organize your data according to the topic discussed.
All in all, interviews are a valuable technique for qualitative research in business, yielding rich and detailed unstructured data. Historically, they have only been limited by the human capacity to interpret and communicate results and conclusions, which demands considerable time and skill.
When you combine this data with AI tools that can interpret it quickly and automatically, it becomes easy to analyze and structure, dovetailing perfectly with your other business data. An additional benefit of natural language analysis tools is that they are free of subjective biases, and can replicate the same approach across as much data as you choose. By combining human research skills with machine analysis, qualitative research methods such as interviews are more valuable than ever to your business.
Related resources
Market intelligence 10 min read, marketing insights 11 min read, ethnographic research 11 min read, qualitative vs quantitative research 13 min read, qualitative research questions 11 min read, qualitative research design 12 min read, primary vs secondary research 14 min read, request demo.
Ready to learn more about Qualtrics?
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Interviews in qualitative research
Affiliation.
- 1 University of Western Sydney, Australia.
- PMID: 25783145
- DOI: 10.7748/nr.22.4.6.s2
Interviews are a common method of data collection in nursing research. They are frequently used alone in a qualitative study or combined with other data collection methods in mixed or multi-method research. Semi-structured interviews, where the researcher has some predefined questions or topics but then probes further as the participant responds, can produce powerful data that provide insights into the participants' experiences, perceptions or opinions.
PubMed Disclaimer
Similar articles
- Researcher or nurse? Difficulties of undertaking semi-structured interviews on sensitive topics. Ashton S. Ashton S. Nurse Res. 2014 Sep;22(1):27-31. doi: 10.7748/nr.22.1.27.e1255. Nurse Res. 2014. PMID: 25251817
- Use of interviews in nursing research. Mitchell G. Mitchell G. Nurs Stand. 2015 Jun 24;29(43):44-8. doi: 10.7748/ns.29.43.44.e8905. Nurs Stand. 2015. PMID: 26103871
- Methodological and ethical issues related to qualitative telephone interviews on sensitive topics. Mealer M, Jones Rn J. Mealer M, et al. Nurse Res. 2014 Mar;21(4):32-7. doi: 10.7748/nr2014.03.21.4.32.e1229. Nurse Res. 2014. PMID: 24673351
- A review of qualitative methodologies used to explore patient perceptions of arts and healthcare. Moss H, Donnellan C, O'Neill D. Moss H, et al. Med Humanit. 2012 Dec;38(2):106-9. doi: 10.1136/medhum-2012-010196. Epub 2012 Aug 14. Med Humanit. 2012. PMID: 22893595 Review.
- A reflection on the use of semi-structured interviews. Dearnley C. Dearnley C. Nurse Res. 2005;13(1):19-28. doi: 10.7748/nr2005.07.13.1.19.c5997. Nurse Res. 2005. PMID: 16220838 Review.
- I Am Afraid I Will Not Be Able to Walk, That Is What Worries Me-The Experience of Patients with Knee Osteoarthritis before Total Knee Arthroplasty: A Qualitative Study. Longo UG, Corradini A, Marchetti A, Di Sarno C, D'Angelo C, Arias C, De Marinis MG, de Sire A, Denaro V. Longo UG, et al. J Clin Med. 2024 May 13;13(10):2878. doi: 10.3390/jcm13102878. J Clin Med. 2024. PMID: 38792420 Free PMC article.
- Development and implementation of a high-fidelity simulation training course for medical and nursing collaboration based on the Fink integrated course design model. Jiang MH, Dou LW, Dong B, Zhang M, Li YP, Lin CX. Jiang MH, et al. Front Med (Lausanne). 2024 Mar 5;11:1286582. doi: 10.3389/fmed.2024.1286582. eCollection 2024. Front Med (Lausanne). 2024. PMID: 38504918 Free PMC article.
- Barriers and facilitators influencing hearing help-seeking behaviors for adults in a peri-urban community in South Africa: a preventive audiology study. Mtimkulu TK, Khoza-Shangase K, Petrocchi-Bartal L. Mtimkulu TK, et al. Front Public Health. 2023 Oct 17;11:1095090. doi: 10.3389/fpubh.2023.1095090. eCollection 2023. Front Public Health. 2023. PMID: 37920587 Free PMC article.
- The Role of Distance from Home to Hospital on Parental Experience in the NICU: A Qualitative Study. Bourque SL, Williams VN, Scott J, Hwang SS. Bourque SL, et al. Children (Basel). 2023 Sep 20;10(9):1576. doi: 10.3390/children10091576. Children (Basel). 2023. PMID: 37761537 Free PMC article.
- Exploring Young Adults' Views About Aroha, a Chatbot for Stress Associated With the COVID-19 Pandemic: Interview Study Among Students. Kang A, Hetrick S, Cargo T, Hopkins S, Ludin N, Bodmer S, Stevenson K, Holt-Quick C, Stasiak K. Kang A, et al. JMIR Form Res. 2023 Oct 12;7:e44556. doi: 10.2196/44556. JMIR Form Res. 2023. PMID: 37527545 Free PMC article.
- Search in MeSH
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Open access
- Published: 24 April 2024
Trauma-Informed Healthcare Leadership? Evidence and opportunities from interviews with leaders during COVID-19
- Sonia Rose Harris ORCID: orcid.org/0000-0002-4599-5684 1 ,
- Alexis Amano ORCID: orcid.org/0000-0001-7136-2197 2 ,
- Marcy Winget ORCID: orcid.org/0000-0002-5893-280X 3 ,
- Kelley M Skeff 3 &
- Cati G Brown-Johnson ORCID: orcid.org/0000-0002-5415-3665 3
BMC Health Services Research volume 24 , Article number: 515 ( 2024 ) Cite this article
565 Accesses
Metrics details
COVID-19 impacted the mental health of healthcare workers, who endured pressures as they provided care during a prolonged crisis. We aimed to explore whether and how a Trauma-Informed Care (TIC) approach was reflected in qualitative perspectives from healthcare leaders of their experience during COVID-19 (2020–2021).
Semi-structured interviews with healthcare leaders from four institutions were conducted. Data analysis consisted of four stages informed by interpretative phenomenological analysis: 1) deductive coding using TIC assumptions, 2) inductive thematic analysis of coded excerpts, 3) keyword-in-context coding of full transcripts for 6 TIC principles with integration into prior inductive themes, and 4) interpretation of themes through 6 TIC principles (safety; trustworthiness and transparency; peer support; collaboration and mutuality; empowerment, voice, and choice; and awareness of cultural, historical, and gender issues).
The actions of leaders ( n = 28) that were reported as successful and supportive responses to the COVID-19 pandemic or else missed opportunities reflected core principles of Trauma-Informed Care. To promote safety , leaders reported affirmative efforts to protect staff by providing appropriate physical protection, and enhanced psychological safety by providing channels for communication about emotional well-being. To promote trustworthiness and transparency, leaders listened to their staff, shared current COVID-19 information, and increased frequency of meetings to disseminate accurate information. To promote mutual support , strategies included wellness check-ins, sharing uplifting stories, affirming common goals, articulating fears, and leading by example. Examples of empowerment included: making time and adjusting modalities for flexible communication; naming challenges outside of the hospital; and functioning as a channel for complaints.
Reported missed opportunities included needing more dedicated time and space for healthcare employees to process emotions, failures in leadership managing their own anxiety, and needing better support for middle managers. Awareness of the TIC principle of cultural, historical, and gender issues was largely absent. Results informed the nascent Trauma-Informed Healthcare Leadership (TIHL) framework.
Conclusions
We propose the Trauma-Informed Healthcare Leadership framework as a useful schema for action and analysis. This approach yields recommendations for healthcare leaders including creating designated spaces for emotional processing, and establishing consistent check-ins that reference personal and professional well-being.
Peer Review reports
In the early years (2020–2021) of the COVID-19 pandemic, the incidence of depression and anxiety increased in the United States (US), and overall psychological well-being decreased [ 1 , 2 , 3 ]. The mental health of healthcare workers was particularly negatively impacted as they endured unrelenting challenges in providing patient care during the prolonged crisis [ 3 , 4 , 5 ]. Negative contributors to mental health for these healthcare workers included: feeling stressed and stretched too thin, concern about exposing family/network to illness, emotional and physical exhaustion, a lack of appropriate emotional support from colleagues and supervisors, and struggles with managing home responsibilities and isolation caused by work requirements [ 6 ]. In response to these negative impacts on healthcare personnel, the US Department of Health and Human Services issued recommendations to transform workplace culture, with goals to 1) empower through reduced administrative tasks, 2) eliminate punitive policies for seeking mental health care, and 3) prioritize social connection by increasing flexibility in scheduling and building peer- and team-based care models [ 7 ]. Healthcare personnel were still expected to continue performing their duties and deliver quality healthcare, often without time for recovery or restoration [ 6 , 7 ].
Previous disaster management reports (e.g., after the 2003 Severe Acute Respiratory Syndrome (SARS) outbreak [ 8 ], 9/11 attack on the United States, and Hurricane Katrina in New Orleans) include lessons learned about the impacts of traumatic events on healthcare workers, such as need for resources that facilitate reflection on new stressors, for systems that mitigate the impact of interpersonal isolation, and for mental health resources without financial barriers for healthcare workers [ 9 , 10 , 11 ]. Analyses of the impact of COVID-19 on healthcare workers showed similar themes [ 3 , 6 , 7 , 10 ], and emphasized the need for hospital- and health system preparedness [ 12 ].
Trauma-informed care (TIC) is considered a gold standard for effective care to support patient mental health [ 13 , 14 , 15 , 16 ]. The TIC framework emphasizes a shift from asking “what’s wrong with you” to “what happened to you,” emphasizing the need for a complete understanding of a person’s lived experience in accounting for and understanding their actions [ 17 ]. This perspective underscores the need to understand a person’s behavior in the context of their life experience [ 17 ]. In medical centers, the application of TIC involves changing organizational culture through policies and procedures and incorporating an understanding of the impact on trauma into routine care [ 18 ]. The US Substance Abuse and Mental Health Services Administration (SAMHSA) outlines four key assumptions (four R’s) in TIC [ 19 ]: 1) Realize the impact of trauma on individuals, families, and groups; 2) Recognize signs of trauma; 3) Respond by applying major TIC principles; 4) avoid Re-traumatization. In addition to these four assumptions, TIC is built on 6 principles [ 19 ]: safety; trustworthiness and transparency; peer support; collaboration and mutuality; empowerment, voice, and choice; and awareness of cultural, historical, and gender issues and oppression. TIC has been widely applied, for instance in schools, social work practices, treatment of domestic violence, juvenile justice, homelessness services, and child welfare agencies [ 15 , 16 , 18 , 20 , 21 ]. Within the last decade, TIC principles have also been applied in healthcare settings; reports in healthcare indicate that TIC can improve patient care outcomes [ 13 , 22 ].
We aimed to explore whether and how a Trauma-Informed Care (TIC) approach was reflected in qualitative perspectives from healthcare leaders of their experience during COVID-19 (2020–2021). Our hope was that this analysis could inform leaders in healthcare about how to support teams and avoid pitfalls during ongoing and future crises.
Participating Institutions and Sampling: Administrative and medical leaders at four healthcare organizations across the United States (from Colorado, Michigan, and Northern California) were invited to participate in a qualitative study. Eligibility included Vice Presidents, Directors, Division Chiefs, and other high-level leadership, with goal of a sample balanced across levels of leadership and also subject matter expertise (e.g., Nursing, IT, Finance.) Institutions represented a convenience sample including three academic medicine centers and one community institution.
Interview Questions/Guide: The interview guide (Additional File 1 ) was developed based on our team’s previous study [ 23 ], and focused on understanding healthcare leader feelings of joy and distress during COVID-19. The guide aimed to identify both gratifying and distressing professional experiences prior to and during the COVID-19 pandemic. We received pilot feedback from a high-level administrator with expertise in wellness.
Recruitment Strategy: Per methods outlined in Skeff et al. [ 23 ], we recruited in a multi-step process to protect the confidentiality of participants. Once a site contact was in place at each institution, the research team furnished them with IRB-approved introduction emails, which underscored research goals and purpose. These emails were sent to potential participants directly from the site contacts. Subsequently, the research team (AA/CBJ) responded directly to potential participants, without cc’ing connecting site contacts. We contacted potential participants no more than three times by email; site contacts were not informed as to who did or did not choose to participate.
Interviews: Two women researchers, with PhD and Master’s level training and expertise in qualitative research (CBJ, AA) conducted phone and video interviews (Zoom, Zoom Video Communications, San Jose, USA); Site A and B interviews were collected August to September 2021, Site C interviews October to November 2021, and Site D interviews in November 2021. Interviews were in-depth and semi-structured, each interview (one per participant) lasted between 30–60 min. One interviewer was additionally a subject matter expert in a related topic area: physician wellness and burnout (CBJ).
Participants provided written consent to participate and verbal consent to record interviews and were assured of the anonymity of interview reporting. Interviews were professionally transcribed (Rev, Rev.com, Inc, San Francisco, USA); any identifying information was deleted.
Qualitative analysis method and rigor: Data analysis for this study used an interpretative phenomenological analysis with theme clustering using TIC Framework [ 24 ]. Data analysis was conducted in four phases: 1) a priori coding using the four TIC assumptions; 2) inductive thematic coding of those excerpts; 3) keyword assisted coding of the full transcripts for elements of the six TIC Principles, and subsequent integration of those excerpts into prior inductive themes; and 4) interpretation of themes through the six TIC Principles. First, we used a priori coding with the deductive framework of TIC assumptions: realize, recognize, respond, and resist re-traumatization . Two qualitative researchers (AA and SRH) consecutively reviewed all transcripts and coded the excerpts to the four assumptions. We identified significant overlap between the four assumptions within the data set; multiple excerpts were coded for all four TIC assumptions. While this addressed our objective of whether TIC elements could be observed in leadership experiences of gratification and distress, it did not address our subsequent question of how TIC might be evidenced in interviews.
Thus, as a second phase, SRH and CBJ used consensus coding approaches to organize TIC excerpts into inductive themes (e.g., listening) using twice-weekly meetings to come to consensus through an iterative process. We simultaneously reviewed literature for other Trauma-Informed Care organizing frameworks to help understand the data.
A third phase of analysis involved mapping inductive themes from the TIC excerpts to the 6 principles of Trauma-Informed Care : 1. Safety; 2. Trustworthiness and transparency; 3. Collaboration and mutuality; 4. Peer support; 5. Empowerment, voice, and choice; and 6. Awareness of cultural, historical, and gender issues . Safety was defined as all people within the organization feeling physically and psychologically safe. Trustworthiness and transparency were defined as organizational activities conducted transparently with a goal of increasing trust. Peer support refers to mutual self-help. Collaboration and mutuality were defined as emphasizing teamwork and power sharing. Empowerment, voice, and choice refer to building on individual strengths and shared decision making and choice. Finally, awareness of cultural, historical, and gender issues was defined as awareness of oppression with efforts to move away from prejudice and bias. These definitions were adapted from the Substance Abuse and Mental Health Service Administration [ 19 ]. Two authors (SRH and CBJ) met weekly to come to consensus over a two-month period [ 25 ]. In addition to this focused consensus analysis, all co-authors reviewed developing organizational patterns of the results during monthly research team meetings.
To ensure a comprehensive account of healthcare leaders’ experiences with this trauma-informed lens, one researcher (SRH) conducted additional coding using a modified keyword-in context approach [ 26 ]. SRH used keywords to search the data set for TIC principles and close synonyms using qualitative software (NVivo 12, QSR International, Melbourne, AUS). Passages containing a keyword were reviewed by two authors (SRH and CBJ) and incorporated into the analysis when the passage included a term used in a way that matched the definitions of the TIC principles used in this dataset. Final structure for the data was organized by the TIC principles.
This project was presented for discussion and feedback in a lecture format and small group sessions to over 40 healthcare leaders interested in clinician wellness and healthcare worker burnout in February and March 2024. This project was approved by our Institutional Review Board (Protocol # 39948).
Participants
Twenty-eight interviews were conducted via phone or Zoom with participants from four healthcare institutions across the United States (in Colorado, Michigan, and Northern California). These institutions represented both academic medical centers and community hospitals. Participants included healthcare leadership in finance, service lines, operations, and education. They filled specific roles of Chief Financial Officer, Chief Nursing Officer, Chief Medical Officer, Executive Director, or Director. Participants were 61% women ( n = 17/28) and included ages across deciles from 30 to 70. 75% were white ( n = 21/28) and all had 10 + years of experience in the field of health care administration. All participants who consented for an interview completed their interview. To maintain anonymity, participants have been assigned a random participant number (1–28). We use the term “leaders” throughout our results to highlight their role as leaders in their setting.
Overall, the actions of leaders that were reported as either successful responses to the COVID-19 pandemic or missed opportunities to alleviate distress mapped to core principles of trauma-informed care. Safety; trustworthiness and transparency; and empowerment, voice, and choice were reflected in our data. Principles of peer support and collaboration and mutuality were combined in our analysis as “mutual support” because while we saw examples of teamwork and power-sharing (collaboration and mutuality), there were not distinct elements of mutual self-help (peer support) perhaps due to power differentials between staff and leadership. The sixth assumption, awareness of cultural, historical, and gender issues, was largely absent from our data set. Leaders’ supportive actions and strategies are presented by TIC principle below. Table 1 provides further qualitative examples, organized first by TIC principle, then by theme. Table 1 also includes recommended future actions based on our data.
Safety . Healthcare leaders employed the principle of safety, which is defined as all members of the organization feeling both physically and psychologically safe, by (1) promoting protection to ensure physical health and (2) by not taking complaints personally. Leaders reported a missed opportunity for supporting psychological safety by not providing more attention, space, and time for emotional processing.
Promoting physical protection . Healthcare leaders reported that addressing staff concerns about physical safety—including the limited supply of personal protective equipment (PPE)—was paramount to supporting staff wellness during COVID-19. Some department’s PPE allotment was lower than staff needs. The disparity in resources raised staff fears and anxiety. In response, leaders reported feeling successful when they increased communication and specifically identified best practices vs. realistic approaches in the current environment.
Even though you know that [reusing masks with different patients, washing masks] is not best practice, it’s better than nothing—but it’s not best practice…. It was hard conversations about what is appropriate and what was the best we could do versus best practice. (Participant 2)
One leader reported using extension intravenous (IV) tubing so that nursing staff could monitor the IVs of patients from outside the intensive care unit (ICU) room. While the participant reported receiving complaints from system executives, there were no negative patient outcomes and staff were extremely satisfied.
In the end, we had absolutely zero negative patient outcomes, and our patients got better care. And the nursing staff was extremely satisfied with that, because they were able to not have to sit in that room with a patient shedding the virus. (Participant 4)
Not taking complaints personally . In best-case scenarios, interviewed healthcare leaders managed to not take complaints personally or respond in anger when they received complaints from staff for situations beyond leadership control. This spirit of acceptance created space for venting frustration without retaliation, supporting psychological safety. When leaders found themselves the target of anger, effective managers worked to let it go. “The anger of the staff that’s directed towards you, even though it’s probably not personal, but you’re the punching bag about not keeping [staff] safe” (Participant 1). In best circumstances leaders looked for potential root causes of the frustration: fear, concern for their team, lack of control:
I’d get an angry email from the head of the department and he’s just looking… out for their staff right? And, and their nurses and their other employees. So I totally get it, right. Cause I’m doing the same for mine… (Participant 8)
Missed opportunity- Not providing more attention, space, and time for emotional processing . Interviewed healthcare leaders reported that they recognized a responsibility as team leads to create space for staff to process emotions by encouraging staff to speak freely without concerns of minimization or retaliation. They reported that not dealing with the emotions of staff during the crisis setting of COVID-19 had a lasting impact:
Even now, we continue to see that and how people are very short with one another, and they don’t allow mistakes in other people and there’s a lot of unneeded hysteria, and I think that it stems back to us not really dealing with all of these emotions that we went through last year. And how do you deal with that on an administrative level, in a hospital when you have hundreds of people reporting to you? I don’t really know the answer to that, but if there was anything that I could have done better, that would’ve been anything. (Participant 7)
Trustworthiness and Transparency . To promote trustworthiness and transparency, defined as organizational activities conducted transparently to increase trust, leaders reported: (1) listening; (2) increasing frequency of information dissemination; and (3) making decisions transparently. Missed opportunities to establish trustworthiness and transparency included: (4) overcommunicating on time off and (5) not containing leadership anxiety.
Listening . Intentional listening in one-on-one interactions worked well to identify specific concerns. Leaders recognized their responsibility to “hear people out, because they need to feel like they've been heard” (Participant 4). Listening with patience established two levels of trust: “So what helps... What I need to do is give myself time to listen and to let people know what we're doing for them. So, both those things take time… one kind of helps establish understanding, trust, and the other helps establish … the next level of trust where, ‘oh, he is acting on some of the things I expressed earlier'” (Participant 4). By listening, one participant learned that staff valued hearing that managers may not have an answer but were making efforts to address staff concerns:
I think that there's a value in just listening and acknowledging and we may not have an answer, and no one does. I feel that to recognize that [transparency] exists, I think goes such a long way and I think that's why we've developed such a great rapport with many of our frontline teams, because they feel, and they see that we hear them. (Participant 5)
Increasing frequency of information dissemination. Healthcare leaders increased the frequency and modality of information dissemination about COVID-19 in response to the changing environment. Specific examples included: increasing team meetings; weekly huddles; and frequent actionable information-sharing. Leaders increased the frequency of communication to address the constant flux of COVID-19 information. A participant recalled increasing meetings to twice a month. Frequent communication in established settings created opportunities to address changing circumstances.
Leaders recognized that timely sharing of information about decision-making and the availability of resources increased trust among staff members and inhibited the spread of rumors.
When communication breaks down, that’s when rumor control starts. So, I think just being fully transparent with where you’re at, whether you had PPE, whether you didn’t. Whether you had to a process together to reuse N-95s…. [The staff] can trust you. Because it comes down to trust, it really does, it comes down to trust. (Participant 25)
Making decisions transparently . When leaders were transparent about their decision-making processes, they could communicate effectively that they were acting in the best interest of staff and patients. When they lacked information due to changing guidelines or circumstances, they reported discomfort.
I think also not always being able to answer questions or give our teams the most. Part of it is we don’t know the answers. And so not being able to provide direction to our team sometimes just because the information was changing. I felt a little bit not powerless, but I felt I always wanted to try to do more, and I couldn’t. So, I think that doesn’t feel great. (Participant 18)
Missed Opportunity- Overcommunicating on time off. Healthcare leaders noted that too much communication, specifically on weekends, sent a message that staff should continue to work even on their days off, which could undermine trust.
When we have the command center set up and there’s these things going, and we say, "Hey, it’s the weekend. You don’t need to do this." And then yet on the weekend, we’re sending them texts or emails and all these pieces... I have definitely heard from quite a few of them for feeling like... They tell us to try and work on... taking care of ourselves and resting and removing ourselves. And then yet these emails come in and it definitely comes across as we expect you to respond to these. (Participant 13)
Missed Opportunity- Containing leadership anxiety . Leaders reported missed opportunities that centered on failures to manage their own anxiety and contain it within their leadership team. Interviewees shared that they failed to protect staff from leadership anxiety, which created more chaos:
The major leadership failure here was that leaders didn’t contain anxiety within their teams. They let that anxiety fuel their own anxiety and threw it out for the organization. So we just all run and collided into each other. It was really damaging, and it took a lot of time to manage… (Participant 17)
Empowerment, Voice, and Choice (Empowerment) . Leaders communicated with staff with flexible times and modalities to promote individual empowerment defined as sharing decision making and choice. Leaders reported that they gave staff options for how and when to connect. Building pathways of support required leaders “to flex our hours, be on our emails constantly, circle back with the staff” (Participant 4). Leaders also added communication modalities - frequent emails, in-person and virtual huddle meetings, personal cell phone communications, texting options, and in-person meetings - to increase accessibility:
I gave my personal cell phone out in addition to my work cell phone, so that the staff could text or call me at any point in time. And they did, and I answered them back and went down and listened to them and their fears…Very difficult time. (Participant 4)
Mutual Support . To promote mutual support, defined as mutual self-help and teamwork, leaders reported: (1) checking on staff wellness and creating personal touch points to foster connection, particularly in virtual settings; (2) leading by example; and (3) sharing positive messages. Leaders reported a missed opportunity for mutual support by not supporting middle managers.
Checking on wellness and creating personal touch points . Leaders strengthened individual relationships with staff through developing or expanding wellness check-ins and personal touch points. These conversations set precedents to communicate about emotional well-being. For example, one leader shared that, in response to work-from-home requirements, they transitioned to “good morning” (Participant 22) emails, increased touch points with staff, and articulated interest in the impact of (home) stressors outside of work. These efforts opened pathways of communication and supported staff well-being:
We established this routine of almost good morning type emails... almost akin to if you were walking down the hallway and going in somebody’s door and just saying good morning. …it was also good from a wellness perspective, just from the standpoint of “we got to just talk” . (Participant 22)
Leading by Example . Leaders led by example, modeling desired behaviors while working to understand the unique needs of staff members. One leader noted that it was the responsibility of the leader to step in when no one else would:
I remember this one time my team doesn’t want to come in back to work, I have a patient I need to discharge. He’s homeless, he refused to wear a mask. He’s coming out to the nursing station, nursing staff [and] doctors freaked out. I remember, I wear a mask ... At that time, we also didn’t have all the PPE that we have, right? I physically went into the room and I have to push the patient’s belongings out, so he can go to a hotel. Somebody has to do the job and at the end, someone has to do it. If nobody does it, a leader has to step in and do it. (Participant 3)
Identifying a common goal . Identifying a common goal motivated teams and set universal expectations for how to respond to the new environment. One participant reported that a shared goal equipped teams to respond cohesively to the crisis.
I think it was obviously a very scary time, a lot of uncertainty surrounding when the pandemic first became, I guess, an outbreak. And one of those things that I felt like went really well as a hospital administrator is the team got together very quickly. The common goal was definitely our motivator to be able to kind of think things through. (Participant 5)
One leader spoke specifically about the common goal of “getting the job done” (Participant 5) . This participant saw team members pivot from their own responsibilities to working collaboratively for team success.
Sharing positive messages. Healthcare leaders reported that positive messages motivated the team and alleviated stress and fear during the early crisis of COVID-19. They reflected awareness that the challenges would impact each person differently recognizing that individual circumstances and prior experiences influence reactions, articulating both the recognize and realize assumption in TIC. In times of crisis, people will experience highs and lows at different times. The responsibility to engage in uplifting communication shifted by day and mood among team members. Positive messages served to “motivate” and to help people “feel better” (Participant 25).
Additionally, sharing positive moments and uplifting stories helped people “rise to the occasion” (Participant 25). To boost morale and positive messaging, leaders focused team messages to emphasize that no two people were having identical experiences during the pandemic, whether at work or at home.
Supporting everybody who was in a different situation. Some people had babies at home, some people had elementary school kids that you can’t just sit in front of a computer and think they’re going to work. There was no two people experiencing the same environment or anxiety, whether it was work-related or not. (Participant 28)
Positive communication unified and strengthened teams to respond to the crisis:
What I really appreciated about our team was it was as though different people were at a high on different days. And so, those people who were feeling better did a really nice job of just building up the team and supporting us and helping us feel good. (Participant 22)
Even in a shared experience, people react differently; however, leaders emphasized unequivocal support for the team, regardless of where they might be.
Missed Opportunity- Supporting middle management . Finally, one leader noted that the demands on middle management coming from front-line teams as well as executive and higher-level leadership were extreme. These leaders could have been better supported by higher-level leadership.
I think the first thing that comes to my mind is trying to figure out the best way to support middle management. Those people that are sort of in between trying to keep the team of frontline people together, but then also have the demands coming down from them, and trying to figure out with the current situation, how do we support that group, so they don’t feel like they’re supposed to be working 24 hours a day, seven days a week, and help them address their own burnout. (Participant 13)
Cultural, Historical, and Gender Issues . One leader reported naming and addressing oppression and racism occurring outside the hospital, acknowledging that there would be an impact on staff. As team leads, participants were also responsible for addressing challenges that could impact staff function, even when they occurred outside of the hospital system and outside of leadership control. For example, one leader described using their leadership platform to talk about George Floyd’s murder and the potential impact of racism on staff:
And I think the one that was really scary, but I felt like I had to do it, was to just talk about race. … I could not let that moment in time go by us without acknowledging how much pain many people… were feeling. (Participant 15)
The Trauma-Informed Healthcare Leadership approach
Our reported results informed the nascent Trauma-Informed Healthcare Leadership (TIHL) approach. The TIHL approach (Fig. 1 & Table 2 ) highlights successful actions and missed opportunities by leaders in different relationships/settings: one-on-one management, team participation and leadership, and at the system level. To promote safety , leaders reported affirmative efforts to protect staff by providing appropriate physical protection (e.g., PPE), and enhanced psychological safety by providing channels for communication about emotional well-being. To promote trustworthiness and transparency, leaders listened to their staff, shared up to date COVID-19 information, and increased frequency of huddles and meetings to disseminate accurate information. To promote mutual support , strategies included wellness check-ins, sharing uplifting stories, affirming common goals, articulating fears; and leading by example. Examples of empowerment included: making time and adjusting modalities for flexible communication; naming challenges outside of the hospital; and functioning as a channel for complaints.
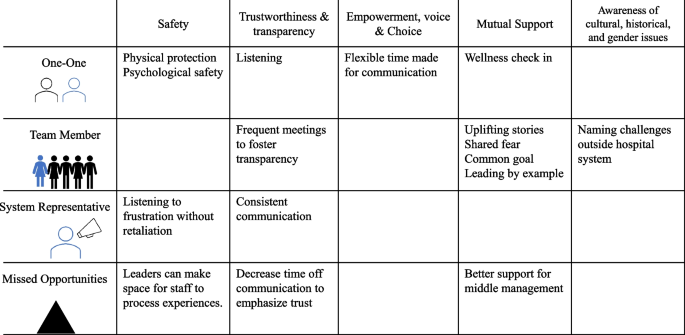
Trauma-Informed Healthcare Leadership: Successful actions and missed opportunities by leaders in one-on-one, team, and system relationships during COVID, mapped to principles of Trauma-Informed Care
This study documents evidence of hospital administrator actions reflecting principles of trauma-informed care (TIC) during the crisis setting of the COVID-19 pandemic. Leaders reported successful actions and missed opportunities to support staff that mapped to core principles of trauma-informed care: safety; trustworthiness and transparency; peer support/collaboration and mutuality; and empowerment, voice, and choice. Awareness of the TIC principle of cultural, historical, and gender issues was largely absent.
Traumatic events, whether experienced at work or outside of employment, can manifest in behaviors or feelings that may not be related to the original stressor [ 27 ]. Through this work, we identified core behaviors to seed the proposed Trauma-Informed Healthcare Leadership (TIHL) framework (Fig. 1 and Table 2 ). These behaviors, which are mapped to the 6 key principles of TIC, suggest actions leaders can take to prevent distress and/or mitigate trauma at different levels of relationships. Based on our data and evidence in the literature, we believe that the application of the Trauma-Informed Healthcare Leadership approach may establish some of the necessary supports to alleviate stress and anxiety related to traumatic events in healthcare—that can manifest as other behaviors or contribute to burnout. Like the Sanctuary Model or other trauma-informed organizational practices [ 28 , 29 , 30 , 31 ], the proposed Trauma-Informed Healthcare Leadership framework could support leaders and staff during healthcare system strain. The Trauma-Informed Healthcare Leadership framework, however, might be more accessible to a broader set of healthcare systems due to its concise approach and strong origin in the well-established Trauma-Informed Care principles. Perhaps a best-case scenario for a system interested in addressing healthcare worker needs during and after crisis would be to start with the Trauma-Informed Healthcare Leadership approach and extend into the Sanctuary Model as time and resources allow [ 28 ].
Addressing Gaps: Supporting mental health, providing dedicated time and space for emotions, elevating needs of middle managers
Notably, leaders reported missed opportunities in the areas of safety, trust, and mutual support , pointing to an underlying gap in leadership awareness and tools to support health care worker emotional experience and mental health. Leaders noted a range of failures related to mental health supports, from a lack of dedicated space for healthcare employees to process emotions related to stressors, to limitations in managing leadership anxiety. Successes exist in the behavioral health sphere in the form of trauma-informed supervision, which we posit could be applied to remedy these gaps. Behavioral health supervision works to prevent and mitigate vicarious trauma and serves as a protective factor against anxiety and depression [ 14 ]. This practice combines knowledge of trauma with supervision and emphasizes that the relationship between supervisor and supervisees must be built on trust, with clear expectations regarding boundaries, listening, and the open exchange of feedback [ 14 ]. Additionally, emotional processing may look different for each individual and change on any given day [ 32 ]. Creating space for emotional processing could be designated spaces for verbal communication about feelings or creating time in the day for rest, exercise, or preparing nutritious food [ 32 ].
While trauma-informed supervision is useful to address gaps, it manifests in a one-to-one relationship; further research is needed to address the application of trauma-informed supervision in a one-to-many or system-mediated relationship. To support teams of health care workers, individuals must have access to a variety of psychological supports—not only through resources such as Employee Assistance Programs, but also by the allocation of time and space for individual processing, as well as with their administrators and managers. Previous literature indicates that providing dedicated spaces through restorative circles (i.e., structured times and space to discuss emotions and perception) to process emotions and self-reflect could increase self-awareness, compassion, and tolerance of stress for all involved.[ 33 ]
Lastly, with respect to leadership-identified gaps, this study also validates the need for targeted support for middle management and frontline managers. Middle managers are essential to the success of the healthcare system because these leaders provide direct support to staff [ 34 ], and this direct manager relationship is more predictive of retention than any other relationship in a work environment [ 35 , 36 , 37 ]. Additionally, previous work indicates that leadership qualities of supervisors impact staff well-being and predict burnout [ 38 ]. However, despite their importance, middle and front line managers may be limited by HR and system constraints [ 39 , 40 ]. Therefore, leveraging resources to support middle level managers may enhance both safety and mutual support (TIC Principles)—and be protective against burnout and attrition. Application of trauma-informed care in elementary school settings that trained administrators in trauma-informed approaches (to apply to students) reduced administrator burnout [ 41 ]. It stands to reason that trauma-informed training for leadership and middle managers with the first goal of supporting their staff may similarly have additional benefits of reducing leadership burnout and fatigue.
Addressing (Lack of) Awareness of Cultural, Historical, and Gender Issues
To address observed blind spot of cultural, historical, and gender issues , system level anti-oppression work is needed. Responses that mapped to the final TIC principle, awareness of cultural, historical, and gender issues , were very rarely discussed by our participants, suggesting that leaders are further hindered in their ability to address the intersection of traumatic experiences. Historically marginalized healthcare workers may be at greater risk for burnout at work[ 42 , 43 ] and poorer mental health in general [ 44 ], in addition to potentially being more vulnerable, as a population, to the impacts of trauma [ 45 , 46 ]. Previous research on racism experienced by physicians of color in health-care settings reports that physicians frequently face overt racism as well as microaggressions in their workplace [ 47 ].
Creating recognition of societal, community, and organizational oppression among healthcare leaders and staff may be the first step in addressing cultural, historical, and gender issues , but naming these issues is only the very first step. Healthcare system leadership may look to anti-racist actions in healthcare delivery to address racism and oppression in the hospital system, such as The Healing ARC or Presence 5 for Racial Justice [ 48 , 49 ]. The Healing ARC, a race-conscious approach developed by two physicians at Brigham and Women’s Hospital, calls for a shift towards holding healthcare institutions accountable for actions that result in racial inequities in health [ 50 , 51 , 52 ]. The Healing ARC is built on three components: 1) acknowledgement, meaning acknowledging how racism has added to inequities in health; 2) redress, meaning putting in place compensatory actions to account for actions; and 3) closure, meaning institutions work collaboratively with the community that has been harmed to affirm that harm has been addressed and repaid [ 50 , 51 , 52 ]. These components are similar to other restorative justice approaches emphasizing acknowledgement of harm [ 33 , 48 ]. Leaders can look to establish this or a similar model within their own system to address institutionalized racism and oppression [ 33 , 53 ].
Limitations
This study has limitations in terms of data collection and analysis. First, the focus of the interviews was not trauma-informed care. Had we asked about TIC principles, participants may have provided more focused responses, particularly regarding awareness of oppression. However, the open nature of interviews can also be seen as a strength of this study. Additionally, we only conducted one interview with each participant. Given the sensitive nature (asking about moments of joy and distress and role during the pandemic) of our interviews, a longitudinal approach may have supported greater relationship rapport and trust, which could have provided more robust examples. Finally, we cannot speak to motivation of behaviors, i.e., were their responses intentionally or unintentionally brought out of trauma-informed care. In terms of participants, our sample only includes leadership. To strengthen the Trauma-Informed Healthcare Leadership approach, it will need validation across staff. Finally, trauma-informed care does not inform a strict adoptions model; instead, this approach offers principles and assumptions. Adapting to TIHL will include defining TIC in the healthcare leadership space while offering recommendations. We hope this work is a first step in that direction.
Healthcare leaders demonstrated application of principles of trauma-informed care during the early crisis of COVID-19, specifically supporting safety, trust, mutual support, and empowerment for staff. They also reported gaps and missed opportunities related to: 1) providing more dedicated time and space for healthcare employees to process emotions related to stressors, 2) failures in managing leadership anxiety, and 3) the need for better support for middle managers. Notably, few participants addressed the principle of cultural, historical, and gender issues, indicating that efforts to promote anti-racist and anti-oppression inclusive work cultures that actively work to address continued discrimination and oppressive practices may be needed. Based on our results and corroborating literature, we propose the Trauma-Informed Healthcare Leadership framework, a straightforward approach with specific recommendations for leadership. Future research can validate and query this emerging approach and expand to middle managers and non-administrator leaders within the healthcare system.
Availability of data and materials
The data that supports these findings are available from the corresponding author, CBJ, upon reasonable request.
Abbreviations
Trauma-Informed Care
Trauma-Informed Healthcare Leadership
United States
Severe Acute Respiratory Syndrome
Substance Abuse and Mental Health Services Administration
Institutional Review Board
Personal protective equipment
Intravenous
Intensive care unit
Coiro MJ, Watson KH, Ciriegio A, et al. Coping with COVID-19 stress: Associations with depression and anxiety in a diverse sample of U.S. adults. Curr Psychol. Published online November 4, 2021. https://doi.org/10.1007/s12144-021-02444-6 .
Kujawa A, Green H, Compas BE, Dickey L, Pegg S. Exposure to COVID-19 pandemic stress: Associations with depression and anxiety in emerging adults in the United States. Depress Anxiety. 2020;37(12):1280–8.
Article CAS PubMed Google Scholar
Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav Immun. 2020;1(89):531–42.
Article Google Scholar
Elbay RY, Kurtulmuş A, Arpacıoğlu S, Karadere E. Depression, anxiety, stress levels of physicians and associated factors in Covid-19 pandemics. Psychiatry Res. 2020;1(290): 113130.
Li Y, Scherer N, Felix L, Kuper H. Prevalence of depression, anxiety and post-traumatic stress disorder in health care workers during the COVID-19 pandemic: A systematic review and meta-analysis. PLoS ONE. 2021;16(3): e0246454.
Article CAS PubMed PubMed Central Google Scholar
De Kock JH, Latham HA, Cowden RG. The mental health of healthcare workers during the COVID-19 pandemic: a narrative review. Curr Opin Psychiatry. 2022;35(5):311–6.
Article PubMed Google Scholar
Mental Health America. [cited 2022 Oct 24]. The Mental Health of Healthcare Workers in COVID-19. Available from: https://mhanational.org/mental-health-healthcare-workers-covid-19
SARS | Basics Factsheet | CDC. [cited 2022 Dec 9]. Available from: https://www.cdc.gov/sars/about/fs-sars.html
Iwai Y, Holdren S, Rosen LT, Hu NY. Narrative trajectories of disaster response: ethical preparedness from Katrina to COVID-19. Med Humanit. 2022;48(2):e8–e8.
DePierro J, Lowe S, Katz C. Lessons learned from 9/11: Mental health perspectives on the COVID-19 pandemic. Psychiatry Res. 2020;1(288): 113024.
Zhong S, Clark M, Hou XY, Zang YL, Fitzgerald G. Development of hospital disaster resilience: conceptual framework and potential measurement. Emerg Med J. 2014;31(11):930–8.
Hendel S, d’Arville A. Reimagining health preparedness in the aftermath of COVID-19. Br J Anaesth. 2022;128(2):e100–3.
King S, Chen KLD, Chokshi B. Becoming Trauma Informed: Validating a Tool to Assess Health Professional’s Knowledge, Attitude, and Practice. Pediatr Qual Saf. 2019;4(5): e215.
Article PubMed PubMed Central Google Scholar
Berger R, Quiros L. Best practices for training trauma-informed practitioners: Supervisors’ voice. Traumatology. 2016;22(2):145–54.
Raja S, Hasnain M, Hoersch M, Gove-Yin S, Rajagopalan C. Trauma Informed Care in Medicine: Current Knowledge and Future Research Directions. Fam Community Health. 2015;38(3):216–26.
Reeves E. A Synthesis of the Literature on Trauma-Informed Care. Issues Ment Health Nurs. 2015;36(9):698–709.
Winfrey O, Perry BD. What Happened to You?: Conversations on Trauma, Resilience, and Healing. 1st ed. An Oprah Book: Flatiron Books; 2021. p. 304.
Google Scholar
Marsac ML, Kassam-Adams N, Hildenbrand AK, Nicholls E, Winston FK, Leff SS, et al. Implementing a Trauma-Informed Approach in Pediatric Health Care Networks. JAMA Pediatr. 2016;170(1):70–7.
Substance Abuse and Mental Health Services Administration. SAMHSA’s Concept of Trauma and Guidance for a Trauma-Informed Approach. Rockville, MD: : Substance Abuse and Mental Health Services Administration; 2014. Report No.: HHS Publication No. (SMA) 14–4884. Available from: https://ncsacw.samhsa.gov/userfiles/files/SAMHSA_Trauma.pdf
Knight C. Trauma Informed Practice and Care: Implications for Field Instruction. Clin Soc Work J. 2019;47(1):79–89.
Koetting C. Trauma-Informed Care: Helping Patients with a Painful Past. J Christ Nurs Q Publ Nurses Christ Fellowsh. 2016;33(4):206–13.
Morrissey JP, Jackson EW, Ellis AR, Amaro H, Brown VB, Najavits LM. Twelve-month outcomes of trauma-informed interventions for women with co-occurring disorders. Psychiatr Serv Wash DC. 2005;56(10):1213–22.
Skeff KM, Brown-Johnson CG, Asch SM, Zionts DL, Winget M, Kerem Y. Professional Behavior and Value Erosion: A Qualitative Study of Physicians and the Electronic Health Record. J Healthc Manag Am Coll Healthc Exec. 2022;67(5):339–52.
Smith J. https://www.apa.org . [cited 2023 Dec 5]. Essentials of Interpretative Phenomenological Analysis. Available from: https://www.apa.org/pubs/books/essentials-interpretative-phenomenological-analysis
Creswell JW, Miller DL. Determining Validity in Qualitative Inquiry. Theory Pract. 2000;39(3):124–30.
Seale C, Charteris-Black J. The SAGE Handbook of Qualitative Methods in Health Research. In London: SAGE Publications Ltd; 2022. Available from: https://methods.sagepub.com/book/sage-hdbk-qualitative-methods-in-health-research
Van der Kolk BA. The Body keeps the score: brain, mind and body in the healing of trauma. New York, NY: Penguin Books; 2015. p. 445.
Esaki N, Benamati J, Yanosy S, Middleton JS, Hopson LM, Hummer VL, et al. The Sanctuary Model: Theoretical Framework. Fam Soc J Contemp Soc Serv. 2013;94(2):87–95.
Bloom S. Caring for the Caregiver: Avoiding and Treating Vicarious Trauma. In 2003. p. 459–70.
Galvin E, O’Donnell R, Avery J, Morris H, Mousa A, Halfpenny N, et al. Residential Out-of-Home Care Staff Perceptions of Implementing a Trauma-Informed Approach: The Sanctuary Model. J Child Adolesc Trauma. 2022;15(3):653–67.
Unick GJ, Bassuk EL, Richard MK, Paquette K. Organizational trauma-informed care: Associations with individual and agency factors. Psychol Serv. 2019;16(1):134–42.
Dr. Lisa Feldman Barrett: How to Understand Emotions | Huberman Lab Podcast. 2023 [cited 2023 Nov 9]. Available from: https://www.youtube.com/watch?v=FeRgqJVALMQ
Lauridsen MB, Munkejord MC. Creating Conditions for Professional Development through a Trauma-Informed and Restorative Practice. Soc Work. 2022;67(2):135–44.
Embertson MK. The importance of middle managers in healthcare organizations. J Healthc Manag Am Coll Healthc Exec. 2006;51(4):223–32.
Naz S, Li C, Nisar QA, Khan MAS, Ahmad N, Anwar F. A Study in the Relationship Between Supportive Work Environment and Employee Retention: Role of Organizational Commitment and Person-Organization Fit as Mediators. SAGE Open. 2020;10(2):2158244020924694.
Allen DG, Bryant PC, Vardaman JM. Retaining Talent: Replacing Misconceptions With Evidence-Based Strategies. Acad Manag Perspect. 2010;24(2):48–64.
Mackenzie ML, Wallach DF. "The Boss-Employee Relationship: Influence on Job Retention" (2012). Faculty Works: Business (1973-2022). 11. https://digitalcommons.molloy.edu/bus_fac/11 .
West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. The Lancet. 2016;388(10057):2272–81.
Kilroy J, Townsend K, Dundon T. Embedding reciprocity in human resource management: A social exchange theory of the role of frontline managers. [cited 2022 Dec 19]. Available from: https://onlinelibrary.wiley.com/doi/full/ https://doi.org/10.1111/1748-8583.12468
Townsend K, Wilkinson A, Bamber G, Allan C. Accidental, unprepared, and unsupported: clinical nurses becoming managers. Int J Hum Resour Manag. 2012;23(1):204–20.
Kim S, Crooks CV, Bax K, Shokoohi M. Impact of Trauma-Informed Training and Mindfulness-Based Social-Emotional Learning Program on Teacher Attitudes and Burnout: A Mixed-Methods Study. School Ment Health. 2021;13(1):55–68.
Joseph MM, Ahasic AM, Clark J, Templeton K. State of Women in Medicine: History, Challenges, and the Benefits of a Diverse Workforce. Pediatrics. 2021;148(Suppl 2):e2021051440C.
Harvey SB, Epstein RM, Glozier N, Petrie K, Strudwick J, Gayed A, et al. Mental illness and suicide among physicians. Lancet Lond Engl. 2021;398(10303):920–30.
Article CAS Google Scholar
Paradies Y, Ben J, Denson N, Elias A, Priest N, Pieterse A, et al. Racism as a Determinant of Health: A Systematic Review and Meta-Analysis. PLoS ONE. 2015;10(9): e0138511.
Anderson M. For black Americans, experiences of racial discrimination vary by education level, gender. Pew Research Center. [cited 2022 Dec 12]. Available from: https://www.pewresearch.org/fact-tank/2019/05/02/for-black-americans-experiences-of-racial-discrimination-vary-by-education-level-gender/
Williams MT, Metzger IW, Leins C, DeLapp C. Assessing racial trauma within a DSM–5 framework: The UConn Racial/Ethnic Stress & Trauma Survey. Pract Innov. 2018;3:242–60.
Serafini K, Coyer C, Speights JB, Donovan D, Guh J, Washington J, et al. Racism as Experienced by Physicians of Color in the Health Care Setting. Fam Med. 2020;52(4):282–7.
Brown-Johnson C, Cox J, Shankar M, Baratta J, De Leon G, Garcia R, et al. The Presence 5 for Racial Justice Framework for anti-racist communication with Black patients. Health Serv Res. [cited 2022 Sep 21];n/a(n/a). Available from: https://onlinelibrary.wiley.com/doi/abs/ https://doi.org/10.1111/1475-6773.14015
Shankar M, Henderson K, Garcia R, Li G, Titer K, Acholonu RG, et al. Presence 5 for Racial Justice Workshop: Fostering Dialogue Across Medical Education to Disrupt Anti-Black Racism in Clinical Encounters. MedEdPORTAL J Teach Learn Resour. 2022;18:11227.
Ansell DA, James B, De Maio FG. A Call for Antiracist Action. N Engl J Med. 2022;387(1): e1.
Boston Review. [cited 2022 Dec 13]. An Antiracist Agenda for Medicine. Available from: https://www.bostonreview.net/articles/michelle-morsebram-wispelwey-what-we-owe-patients-case-medical-reparations/
P W, H M, WilsonMichael, MazimbaSula, K H, P A, et al. Leveraging Clinical Decision Support for Racial Equity: A Sociotechnical Innovation. NEJM Catal Innov Care Deliv. 2022 Jul 25 [cited 2022 Dec 13]; Available from: https://catalyst.nejm.org/doi/full/ https://doi.org/10.1056/CAT.22.0076
Coates R, Umbreit M, Vos B. Restorative justice circles: An exploratory study. Contemp Justice Rev. 2003;6(3):265–78.
Download references
Acknowledgements
Not applicable
This study was funded by Stanford University School of Medicine.
Author information
Authors and affiliations.
School of Social Work, University of Minnesota, St. Paul, MN, USA
Sonia Rose Harris
UCLA Fielding School of Public Health, Los Angeles, CA, USA
Alexis Amano
Stanford University School of Medicine, Palo Alto, CA, USA
Marcy Winget, Kelley M Skeff & Cati G Brown-Johnson
You can also search for this author in PubMed Google Scholar
Contributions
CBJ, SRH, AA, MW, and KS contributed to conception and design. SRH and CBJ wrote the main manuscript text. AA and CBJ conducted data collection. SRH, AA, and CBJ conducted data analysis, which was reviewed in monthly meetings by MW and KS. All authors reviewed the manuscript.
Corresponding author
Correspondence to Cati G Brown-Johnson .
Ethics declarations
Ethics approval and consent to participate.
This project was approved by our Stanford University Institutional Review Board (Protocol # 39948). All the methods and procedures carried out in this study were in accordance with relevant guidelines and regulation. Written consent was obtained from all participants to participate. Verbal informed consent was obtained from all participants at the beginning of the interview to record and transcribe interviews. This was approved by the Stanford University Institutional Review Board.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Interview Protocol
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Harris, S., Amano, A., Winget, M. et al. Trauma-Informed Healthcare Leadership? Evidence and opportunities from interviews with leaders during COVID-19. BMC Health Serv Res 24 , 515 (2024). https://doi.org/10.1186/s12913-024-10946-9
Download citation
Received : 15 May 2023
Accepted : 02 April 2024
Published : 24 April 2024
DOI : https://doi.org/10.1186/s12913-024-10946-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Administrators
- Qualitative methods
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
- Open access
- Published: 03 June 2024
The use of evidence to guide decision-making during the COVID-19 pandemic: divergent perspectives from a qualitative case study in British Columbia, Canada
- Laura Jane Brubacher ORCID: orcid.org/0000-0003-2806-9539 1 , 2 ,
- Chris Y. Lovato 1 ,
- Veena Sriram 1 , 3 ,
- Michael Cheng 1 &
- Peter Berman 1
Health Research Policy and Systems volume 22 , Article number: 66 ( 2024 ) Cite this article
144 Accesses
2 Altmetric
Metrics details
The challenges of evidence-informed decision-making in a public health emergency have never been so notable as during the COVID-19 pandemic. Questions about the decision-making process, including what forms of evidence were used, and how evidence informed—or did not inform—policy have been debated.
We examined decision-makers' observations on evidence-use in early COVID-19 policy-making in British Columbia (BC), Canada through a qualitative case study. From July 2021- January 2022, we conducted 18 semi-structured key informant interviews with BC elected officials, provincial and regional-level health officials, and civil society actors involved in the public health response. The questions focused on: (1) the use of evidence in policy-making; (2) the interface between researchers and policy-makers; and (3) key challenges perceived by respondents as barriers to applying evidence to COVID-19 policy decisions. Data were analyzed thematically, using a constant comparative method. Framework analysis was also employed to generate analytic insights across stakeholder perspectives.
Overall, while many actors’ impressions were that BC's early COVID-19 policy response was evidence-informed, an overarching theme was a lack of clarity and uncertainty as to what evidence was used and how it flowed into decision-making processes. Perspectives diverged on the relationship between 'government' and public health expertise, and whether or not public health actors had an independent voice in articulating evidence to inform pandemic governance. Respondents perceived a lack of coordination and continuity across data sources, and a lack of explicit guidelines on evidence-use in the decision-making process, which resulted in a sense of fragmentation. The tension between the processes involved in research and the need for rapid decision-making was perceived as a barrier to using evidence to inform policy.
Conclusions
Areas to be considered in planning for future emergencies include: information flow between policy-makers and researchers, coordination of data collection and use, and transparency as to how decisions are made—all of which reflect a need to improve communication. Based on our findings, clear mechanisms and processes for channeling varied forms of evidence into decision-making need to be identified, and doing so will strengthen preparedness for future public health crises.
Peer Review reports
The challenges of evidence-informed decision-making Footnote 1 in a public health emergency have never been so salient as during the COVID-19 pandemic, given its unprecedented scale, rapidly evolving virology, and multitude of global information systems to gather, synthesize, and disseminate evidence on the SARS-CoV-2 virus and associated public health and social measures [ 1 , 2 , 3 ]. Early in the COVID-19 pandemic, rapid decision-making became central for governments globally as they grappled with crucial decisions for which there was limited evidence. Critical questions exist, in looking retrospectively at these decision-making processes and with an eye to strengthening future preparedness: Were decisions informed by 'evidence'? What forms of evidence were used, and how, by decision-makers? [ 4 , 5 , 6 ].
Scientific evidence, including primary research, epidemiologic research, and knowledge synthesis, is one among multiple competing influences that inform decision-making processes in an outbreak such as COVID-19 [ 7 ]. Indeed, the use of multiple forms of evidence has been particularly notable as it applies to COVID-19 policy-making. Emerging research has also documented the important influence of ‘non-scientific’ evidence such as specialized expertise and experience, contextual information, and level of available resources [ 8 , 9 , 10 ]. The COVID-19 pandemic has underscored the politics of evidence-use in policy-making [ 11 ]; what evidence is used and how can be unclear, and shaped by political bias [ 4 , 5 ]. Moreover, while many governments have established scientific advisory boards, the perspectives of these advisors were reportedly largely absent from COVID-19 policy processes [ 6 ]. How evidence and public health policy interface—and intersect—is a complex question, particularly in the dynamic context of a public health emergency.
Within Canada, a hallmark of the public health system and endorsed by government is evidence-informed decision-making [ 12 ]. In British Columbia (BC), Canada, during the early phases of COVID-19 (March—June 2020), provincial public health communication focused primarily on voluntary compliance with recommended public health and social measures, and on supporting those most affected by the pandemic. Later, the response shifted from voluntary compliance to mandatory enforceable government orders [ 13 ]. Like many other jurisdictions, the government’s public messaging in BC asserted that the province took an approach to managing the COVID-19 pandemic and developing related policy that was based on scientific evidence, specifically. For example, in March 2021, in announcing changes to vaccination plans, Dr. Bonnie Henry, the Provincial Health Officer, stated, " This is science in action " [ 14 ]. As a public health expert with scientific voice, the Provincial Health Officer has been empowered to speak on behalf of the BC government across the COVID-19 pandemic progression. While this suggests BC is a jurisdiction which has institutionalized scientifically-informed decision-making as a core tenet of effective public health crisis response, it remains unclear as to whether BC’s COVID-19 response could, in fact, be considered evidence-informed—particularly from the perspectives of those involved in pandemic decision-making and action. Moreover, if evidence-informed, what types of evidence were utilized and through what mechanisms, how did this evidence shape decision-making, and what challenges existed in moving evidence to policy and praxis in BC’s COVID-19 response?
The objectives of this study were: (1) to explore and characterize the perspectives of BC actors involved in the COVID-19 response with respect to evidence-use in COVID-19 decision-making; and (2) to identify opportunities for and barriers to evidence-informed decision-making in BC’s COVID-19 response, and more broadly. This inquiry may contribute to identifying opportunities for further strengthening the synthesis and application of evidence (considered broadly) to public health policy and decision-making, particularly in the context of future public health emergencies, both in British Columbia and other jurisdictions.
Study context
This qualitative study was conducted in the province of British Columbia (BC), Canada, a jurisdiction with a population of approximately five million people [ 15 ]. Within BC’s health sector, key actors involved in the policy response to COVID-19 included: elected officials, the BC Government’s Ministry of Health (MOH), the Provincial Health Services Authority (PHSA), Footnote 2 the Office of the Provincial Health Officer (PHO), Footnote 3 the BC Centre for Disease Control (BCCDC), Footnote 4 and Medical Health Officers (MHOs) and Chief MHOs at regional and local levels.
Health research infrastructure within the province includes Michael Smith Health Research BC [ 16 ] and multiple post-secondary research and education institutions (e.g., The University of British Columbia). Unlike other provincial (e.g., Ontario) and international (e.g., UK) jurisdictions, BC did not establish an independent, formal scientific advisory panel or separate organizational structure for public health intelligence in COVID-19. That said, a Strategic Research Advisory Council was established, reporting to the MOH and PHO, to identify COVID-19 research gaps and commission needed research for use within the COVID-19 response [ 17 ].
This research was part of a multidisciplinary UBC case study investigating the upstream determinants of the COVID-19 response in British Columbia, particularly related to institutions, politics, and organizations and how these interfaced with, and affected, pandemic governance [ 18 ]. Ethics approval for this study was provided by the University of British Columbia (UBC)’s Institutional Research Ethics Board (Certificate #: H20-02136).
Data collection
From July 2021 to January 2022, 18 semi-structured key informant interviews were conducted with BC elected officials, provincial and regional-level health officials, and civil society actors (e.g., within non-profit research organizations, unions) (Table 1 ). Initially, respondents were purposively sampled, based on their involvement in the COVID-19 response and their positioning within the health system organizational structure. Snowball sampling was used to identify additional respondents, with the intent of representing a range of organizational roles and actor perspectives. Participants were recruited via email invitation and provided written informed consent to participate.
Interviews were conducted virtually using Zoom® videoconferencing, with the exception of one hybrid in-person/Zoom® interview. Each interview was approximately one hour in duration. One to two research team members led each interview. The full interview protocol focused on actors’ descriptions of decision-making processes across the COVID-19 pandemic progression, from January 2020 to the date of the interviews, and they were asked to identify key decision points (e.g., emergency declaration, business closures) [see Additional File 1 for the full semi-structured interview guide]. For this study, we used a subset of interview questions focused on evidence-use in the decision-making process, and the organizational structures or actors involved, in BC's early COVID-19 pandemic response (March–August 2020). Questions were adapted to be relevant to a respondent’s expertise and particular involvement in the response. ‘Evidence’ was left undefined and considered broadly by the research team (i.e., both ‘scientific’/research-based and ‘non-scientific’ inputs) within interview questions, and therefore at the discretion of the participant as to what inputs they perceived and described as ‘evidence’ that informed or did not inform pandemic decision-making. Interviews were audio-recorded over Zoom® with permission and transcribed using NVivo Release 1.5© software. Each transcript was then manually verified for accuracy by 1–2 members of the research team.
Data analysis
An inductive thematic analysis was conducted, using a constant comparative method, to explore points of divergence and convergence across interviews and stakeholder perspectives [ 19 ]. Transcripts were inductively coded in NVivo Release 1.5© software, which was used to further organize and consolidate codes, generate a parsimonious codebook to fit the data, and retrieve interview excerpts [ 20 ]. Framework analysis was also employed as an additional method for generating analytic insights across stakeholder perspectives and contributed to refining the overall coding [ 21 ]. Triangulation across respondents and analytic methods, as well as team collaboration in reviewing and refining the codebook, contributed to validity of the analysis [ 22 ].
How did evidence inform early COVID-19 policy-making in BC?
Decision-makers described their perceptions on the use of evidence in policy-making; the interface between researchers and policy-makers; and specific barriers to evidence-use in policy-making within BC’s COVID-19 response. In discussing the use of evidence, respondents focused on ‘scientific’ evidence; however, they noted a lack of clarity as to how and what evidence flowed into decision-making. They also acknowledged that ‘scientific’ evidence was one of multiple factors influencing decisions. The themes described below reflect the narrative underlying their perspectives.
Perceptions of evidence-use
Multiple provincial actors generally expressed confidence or had an overall impression that decisions were evidence-based (IDI5,9), stating definitively that, "I don’t think there was a decision we made that wasn’t evidence-informed" (IDI9) and that "the science became a driver of decisions that were made" (IDI5). However, at the regional health authority level, one actor voiced skepticism that policy decisions were consistently informed by scientific evidence specifically, stating, "a lot of decisions [the PHO] made were in contrast to science and then shifted to be by the science" ( IDI6). The evolving nature of the available evidence and scientific understanding of the virus throughout the pandemic was acknowledged. For instance, one actor stated that, "I’ll say the response has been driven by the science; the science has been changing…from what I’ve seen, [it] has been a very science-based response" (IDI3).
Some actors narrowed in on certain policy decisions they believed were or were not evidence-informed. Policy decisions in 2020 that actors believed were directly informed by scientific data included the early decision to restrict informal, household gatherings; to keep schools open for in-person learning; to implement a business safety plan requirement across the province; and to delay the second vaccine dose for maximum efficacy. One provincial public health actor noted that an early 2020 decision made, within local jurisdictions, to close playgrounds was not based on scientific evidence. Further, the decision prompted public health decision-makers to centralize some decision-making to the provincial level, to address decisions being made 'on the ground' that were not based on scientific evidence (IDI16). Similarly, they added that the policy decision to require masking in schools was not based on scientific evidence; rather, "it's policy informed by the noise of your community." As parents and other groups within the community pushed for masking, this was "a policy decision to help schools stay open."
Early in the pandemic response, case data in local jurisdictions were reportedly used for monitoring and planning. These "numerator data" (IDI1), for instance case or hospitalization counts, were identified as being the primary mode of evidence used to inform decisions related to the implementation or easing of public health and social measures. The ability to generate epidemiological count data early in the pandemic due to efficient scaling up of PCR testing for COVID-19 was noted as a key advantage (IDI16). As the pandemic evolved in 2020, however, perspectives diverged in relation to the type of data that decision-makers relied on. For example, it was noted that BCCDC administered an online, voluntary survey to monitor unintended consequences of public health and social measures and inform targeted interventions. Opinions varied on whether this evidence was successfully applied in decision-making. One respondent emphasized this lack of application of evidence and perceived that public health orders were not informed by the level and type of evidence available, beyond case counts: "[In] a communicable disease crisis like a pandemic, the collateral impact slash damage is important and if you're going to be a public health institute, you actually have to bring those to the front, not just count cases" (IDI1).
There also existed some uncertainty and a perceived lack of transparency or clarity as to how or whether data analytic ‘entities’, such as BCCDC or research institutions, fed directly into decision-making. As a research actor shared, "I’m not sure that I know quite what all those channels really look like…I’m sure that there’s a lot of improvement that could be driven in terms of how we bring strong evidence to actual policy and practice" (IDI14). Another actor explicitly named the way information flowed into decision-making in the province as "organic" (IDI7). They also noted the lack of a formal, independent science advisory panel for BC’s COVID-19 response, which existed in other provincial and international jurisdictions. Relatedly, one regional health authority actor perceived that the committee that was convened to advise the province on research, and established for the purpose of applying research to the COVID-19 response, "should have focused more on knowledge translation, but too much time was spent commissioning research and asking what kinds of questions we needed to ask rather than looking at what was happening in other jurisdictions" (IDI6). Overall, multiple actors noted a lack of clarity around application of evidence and who is responsible for ensuring evidence is applied. As a BCCDC actor expressed, in relation to how to prevent transmission of COVID-19:
We probably knew most of the things that we needed to know about May of last year [2020]. So, to me, it’s not even what evidence you need to know about, but who’s responsible for making sure that you actually apply the evidence to the intervention? Because so many of our interventions have been driven by peer pressure and public expectation rather than what we know to be the case [scientifically] (IDI1).
Some described the significance of predictive disease modelling to understand the COVID-19 trajectory and inform decisions, as well as to demonstrate to the public the effectiveness of particular measures, which "help[ed] sustain our response" (IDI2). Others, however, perceived that "mathematical models were vastly overused [and] overvalued in decision-making around this pandemic" (IDI1) and that modellers stepped outside their realm of expertise in providing models and policy recommendations through the public media.
Overall, while many actors’ impressions were that the response was evidence-informed, an overarching theme was a lack of clarity and uncertainty with respect to how evidence actually flowed into decision-making processes, as well as what specific evidence was used and how. Participants noted various mechanisms created or already in place prior to COVID-19 that fed data into, and facilitated, decision-making. There was an acknowledgement that multiple forms of evidence—including scientific data, data on public perceptions, as well as public pressure—appeared to have influenced decision-making.
Interface between researchers and policy-makers
There was a general sense that the Ministry supported the use of scientific and research-based evidence specifically. Some actors identified particular Ministry personnel as being especially amenable to research and focused on data to inform decisions and implementation. More broadly, the government-research interface was characterized by one actor as an amicable one, a "research-friendly government", and that the Ministry of Health (MOH), specifically, has a research strategy whereby, "it’s literally within their bureaucracy to become a more evidence-informed organization" (IDI11). The MOH was noted to have funded a research network intended to channel evidence into health policy and practice, and which reported to the research side of the MOH.
Other actors perceived relatively limited engagement with the broader scientific community. Some perceived an overreliance on 'in-house expertise' or a "we can do that [ourselves] mentality" within government that precluded academic researchers’ involvement, as well as a sense of "not really always wanting to engage with academics to answer policy questions because they don’t necessarily see the value that comes" (IDI14). With respect to the role of research, an actor stated:
There needs to be a provincial dialogue around what evidence is and how it gets situated, because there’s been some tension around evidence being produced and not used or at least not used in the way that researchers think that it should be (IDI11).
Those involved in data analytics within the MOH acknowledged a challenge in making epidemiological data available to academic researchers, because "at the time, you’re just trying to get decisions made" (IDI7). Relatedly, a research actor described the rapid instigation of COVID-19 research and pivoting of academic research programs to respond to the pandemic, but perceived a slow uptake of these research efforts from the MOH and PHSA for decision-making and action. Nevertheless, they too acknowledged the challenge of using research evidence, specifically, in an evolving and dynamic pandemic:
I think we’ve got to be realistic about what research in a pandemic situation can realistically contribute within very short timelines. I mean, some of these decisions have to be made very quickly...they were intuitive decisions, I think some of them, rather than necessarily evidence-based decisions (IDI14).
Relatedly, perspectives diverged on the relationship between 'government' and public health expertise, and whether or not public health actors had an independent voice in articulating evidence to inform governance during the pandemic. Largely from Ministry stakeholders, and those within the PHSA, the impressions were that Ministry actors were relying on public health advice and scientific expertise. As one actor articulated, "[the] government actually respected and acknowledged and supported public health expertise" (IDI9). Others emphasized a "trust of the people who understood the problem" (IDI3)—namely, those within public health—and perceived that public health experts were enabled "to take a lead role in the health system, over politics" (IDI12). This perspective was not as widely held by those in the public health sector, as one public health actor expressed, "politicians and bureaucrats waded into public health practice in a way that I don't think was appropriate" and that, "in the context of a pandemic, it’s actually relatively challenging to bring true expert advice because there’s too many right now. Suddenly, everybody’s a public health expert, but especially bureaucrats and politicians." They went on to share that the independence of public health to speak and act—and for politicians to accept independent public health advice—needs to be protected and institutionalized as "core to good governance" (IDI1). Relatedly, an elected official linked this to the absence of a formal, independent science table to advise government and stated that, "I think we should have one established permanently. I think we need to recognize that politicians aren't always the best at discerning scientific evidence and how that should play into decision-making" (IDI15).
These results highlight the divergent perspectives participants had as to the interface between research and policy-making and a lack of understanding regarding process and roles.
Challenges in applying evidence to policy decisions
Perspectives converged with respect to the existence of numerous challenges with and barriers to applying evidence to health policy and decision-making. These related to the quality and breadth of available data, both in terms of absence and abundance. For instance, as one public health actor noted in relation to health policy-making, "you never have enough information. You always have an information shortage, so you're trying to make the best decisions you can in the absence of usually really clear information" (IDI8). On the other hand, as evidence emerged en masse across jurisdictions in the pandemic, there were challenges with synthesizing evidence in a timely fashion for 'real-time' decision-making. A regional health authority actor highlighted this challenge early in the COVID-19 pandemic and perceived that there was not a provincial group bringing new synthesized information to decision-makers on a daily basis (IDI6). Other challenges related to the complexity of the political-public health interface with respect to data and scientific expertise, which "gets debated and needs to be digested by the political process. And then decisions are made" (IDI5). This actor further expressed that debate among experts needs to be balanced with efficient crisis response, that one has to "cut the debate short. For the sake of expediency, you need to react."
It was observed that, in BC’s COVID-19 response, data was gathered from multiple sources with differing data collection procedures, and sometimes with conflicting results—for instance, 'health system data' analyzed by the PHSA and 'public health data' analyzed by the BCCDC. This was observed to present challenges from a political perspective in discerning "who’s actually getting the 'right' answers" (IDI7). An added layer of complexity was reportedly rooted in how to communicate such evidence to the public and "public trust in the numbers" (IDI7), particularly as public understanding of what evidence is, how it is developed, and why it changes, can influence public perceptions of governance.
Finally, as one actor from within the research sector noted, organizationally and governance-wise, the system was "not very well set up to actually use research evidence…if we need to do better at using evidence in practice, we need to fix some of those things. And we actually know what a lot of those things are." For example , "there’s no science framework for how organizations work within that" and " governments shy away from setting science policy " (IDI11). This challenge was framed as having a macro-level dimension, as higher-level leadership structures were observed to not incentivize the development and effective use of research among constituent organizations, and also micro-level implications. From their perspective, researchers will struggle without such policy frameworks to obtain necessary data-sharing agreements with health authorities, nor will they be able to successfully navigate other barriers to conducting action-oriented research that informs policy and practice.
Similarly, a research actor perceived that the COVID-19 pandemic highlighted pre-existing fragmentation, "a pretty disjointed sort of enterprise" in how research is organized in the province:
I think pandemics need strong leadership and I think pandemic research response needed probably stronger leadership than it had. And I think that’s to do with [how] no one really knew who was in charge because no one really was given the role of being truly in charge of the research response (IDI14).
This individual underscored that, at the time of the interview, there were nearly 600 separate research projects being conducted in BC that focused on COVID-19. From their perspective, this reflected the need for more centralized direction to provide leadership, coordinate research efforts, and catalyze collaborations.
Overall, respondents perceived a lack of coordination and continuity across data sources, and a lack of explicit guidelines on evidence-use in the decision-making process, which resulted in a sense of fragmentation. The tension between the processes involved in research and the need for rapid decision-making was perceived as a barrier to using evidence to inform policy.
This study explored the use of evidence to inform early COVID-19 decision-making within British Columbia, Canada, from the perspectives of decision-makers themselves. Findings underscore the complexity of synthesizing and applying evidence (i.e., ‘scientific’ or research-based evidence most commonly discussed) to support public health policy in 'real-time', particularly in the context of public health crisis response. Despite a substantial and long-established literature on evidence-based clinical decision-making [ 23 , 24 ], understanding is more limited as to how public health crisis decision-making can be evidence-informed or evidence-based. By contributing to a growing global scholarship of retrospective examinations of COVID-19 decision-making processes [ 25 , 26 , 27 , 28 ], our study aimed to broaden this understanding and, thus, support the strengthening of public health emergency preparedness in Canada, and globally.
Specifically, based on our findings on evidence-based public health practice, we found that decision-makers clearly emphasized ‘evidence-based’ or ‘evidence-informed’ as meaning ‘scientific’ evidence. They acknowledged other forms of evidence such as professional expertise and contextual information as influencing factors. We identified four key points related to the process of evidence-use in BC's COVID-19 decision-making, with broader implications as well:
Role Differences: The tensions we observed primarily related to a lack of clarity among the various agencies involved as to their respective roles and responsibilities in a public health emergency, a finding that aligns with research on evidence-use in prior pandemics in Canada [ 29 ]. Relatedly, scientists and policy-makers experienced challenges with communication and information-flow between one another and the public, which may reflect their different values and standards, framing of issues and goals, and language [ 30 ].
Barriers to Evidence-Use: Coordination and consistency in how data are collected across jurisdictions reportedly impeded efficiency and timeliness of decision-making. Lancaster and Rhodes (2020) suggest that evidence itself should be treated as a process, rather than a commodity, in evidence-based practice [ 31 ]. Thus, shifting the dialogue from 'barriers to evidence use' to an approach that fosters dialogue across different forms of evidence and different actors in the process may be beneficial.
Use of Evidence in Public Health versus Medicine: Evidence-based public health can be conflated with the concept of evidence-based medicine, though these are distinct in the type of information that needs to be considered. While ‘research evidence’ was the primary type of evidence used, other important types of evidence informed policy decisions in the COVID-19 public health emergency—for example, previous experience, public values, and preferences. This concurs with Brownson’s (2009) framework of factors driving decision-making in evidence-based public health [ 32 ]. Namely, that a balance between multiple factors, situated in particular environmental and organizational context, shapes decision-making: 1) best available research evidence; 2) clients'/population characteristics, state, needs, values, and preferences; and 3) resources, including a practitioner’s expertise. Thus, any evaluation of evidence-use in public health policy must take into consideration this multiplicity of factors at play, and draw on frameworks specific to public health [ 33 ]. Moreover, public health decision-making requires much more attention to behavioural factors and non-clinical impacts, which is distinct from the largely biology-focused lens of evidence-based medicine.
Transparency: Many participants emphasized a lack of explanation about why certain decisions were made and a lack of understanding about who was involved in decisions and how those decisions were made. This point was confirmed by a recent report on lessons learned in BC during the COVID-19 pandemic in which the authors describe " the desire to know more about the reasons why decisions were taken " as a " recurring theme " (13:66). These findings point to a need for clear and transparent mechanisms for channeling evidence, irrespective of the form used, into public health crisis decision-making.
Our findings also pointed to challenges associated with the infrastructure for utilizing research evidence in BC policy-making, specifically a need for more centralized authority on the research side of the public health emergency response to avoid duplication of efforts and more effectively synthesize findings for efficient use. Yet, as a participant questioned, what is the realistic role of research in a public health crisis response? Generally, most evidence used to inform crisis response measures is local epidemiological data or modelling data [ 7 ]. As corroborated by our findings, challenges exist in coordinating data collection and synthesis of these local data across jurisdictions to inform 'real-time' decision-making, let alone to feed into primary research studies [ 34 ].
On the other hand, as was the case in the COVID-19 pandemic, a 'high noise' research environment soon became another challenge as data became available to researchers. Various mechanisms have been established to try and address these challenges amid the COVID-19 pandemic, both to synthesize scientific evidence globally and to create channels for research evidence to support timely decision-making. For instance: 1) research networks and collaborations are working to coordinate research efforts (e.g., COVID-END network [ 35 ]); 2) independent research panels or committees within jurisdictions provide scientific advice to inform decision-making; and 3) research foundations, funding agencies, and platforms for knowledge mobilization (e.g., academic journals) continue to streamline funding through targeted calls for COVID-19 research grant proposals, or for publication of COVID-19 research articles. While our findings describe the varied forms of evidence used in COVID-19 policy-making—beyond scientific evidence—they also point to the opportunity for further investments in infrastructure that coordinates, streamlines, and strengthens collaborations between health researchers and decision-makers that results in timely uptake of results into policy decisions.
Finally, in considering these findings, it is important to note the study's scope and limitations: We focused on evidence use in a single public health emergency, in a single province. Future research could expand this inquiry to a multi-site analysis of evidence-use in pandemic policy-making, with an eye to synthesizing lessons learned and best practices. Additionally, our sample of participants included only one elected official, so perspectives were limited from this type of role. The majority of participants were health officials who primarily referred to and discussed evidence as ‘scientific’ or research-based evidence. Further work could explore the facilitators and barriers to evidence-use from the perspectives of elected officials and Ministry personnel, particularly with respect to the forms of evidence—considered broadly—and other varied inputs, that shape decision-making in the public sphere. This could include a more in-depth examination of policy implementation and how the potential societal consequences of implementation factor into public health decision-making.
We found that the policy decisions made during the initial stages of the COVID-19 pandemic were perceived by actors in BC's response as informed by—not always based on—scientific evidence, specifically; however, decision-makers also considered other contextual factors and drew on prior pandemic-related experience to inform decision-making, as is common in evidence-based public health practice [ 32 ]. The respondents' experiences point to specific areas that need to be considered in planning for future public health emergencies, including information flow between policy-makers and researchers, coordination in how data are collected, and transparency in how decisions are made—all of which reflect a need to improve communication. Furthermore, shifting the discourse from evidence as a commodity to evidence-use as a process will be helpful in addressing barriers to evidence-use, as well as increasing understanding about the public health decision-making process as distinct from clinical medicine. Finally, there is a critical need for clear mechanisms that channel evidence (whether ‘scientific’, research-based, or otherwise) into health crisis decision-making, including identifying and communicating the decision-making process to those producing and synthesizing evidence. The COVID-19 pandemic experience is an opportunity to reflect on what needs to be done to guild our public health systems for the future [ 36 , 37 ]. Understanding and responding to the complexities of decision-making as we move forward, particularly with respect to the synthesis and use of evidence, can contribute to strengthening preparedness for future public health emergencies.
Availability of data and materials
The data that support the findings of this study are not publicly available to maintain the confidentiality of research participants.
The terms 'evidence-informed' and 'evidence-based' decision-making are used throughout this paper, though are distinct. The term 'evidence-informed' suggests that evidence is used and considered, though not necessarily solely determinative in decision-making [ 38 ].
The Provincial Health Services Authority (PHSA) works with the Ministry of Health (MOH) and regional health authorities to oversee the coordination and delivery of programs.
The Office of the Provincial Health Officer (PHO) has binding legal authority in the case of an emergency, and responsibility to monitor the health of BC’s population and provide independent advice to Ministers and public offices on public health issues.
The British Columbia Centre for Disease Control (BCCDC) is a program of the PHSA and provides provincial and national disease surveillance, detection, treatment, prevention, and consultation.
Abbreviations
British Columbia
British Columbia Centre for Disease Control
Coronavirus Disease 2019
Medical Health Officer
Ministry of Health
Provincial Health Officer
Provincial Health Services Authority
Severe Acute Respiratory Syndrome Coronavirus—2
University of British Columbia
Rubin O, Errett NA, Upshur R, Baekkeskov E. The challenges facing evidence-based decision making in the initial response to COVID-19. Scand J Public Health. 2021;49(7):790–6.
Article PubMed Google Scholar
Williams GA, Ulla Díez SM, Figueras J, Lessof S, Ulla SM. Translating evidence into policy during the COVID-19 pandemic: bridging science and policy (and politics). Eurohealth (Lond). 2020;26(2):29–48.
Google Scholar
Vickery J, Atkinson P, Lin L, Rubin O, Upshur R, Yeoh EK, et al. Challenges to evidence-informed decision-making in the context of pandemics: qualitative study of COVID-19 policy advisor perspectives. BMJ Glob Heal. 2022;7(4):1–10.
Piper J, Gomis B, Lee K. “Guided by science and evidence”? The politics of border management in Canada’s response to the COVID-19 pandemic. Front Polit Sci. 2022;4
Cairney P. The UK government’s COVID-19 policy: what does “Guided by the science” mean in practice? Front Polit Sci. 2021;3(March):1–14.
Colman E, Wanat M, Goossens H, Tonkin-Crine S, Anthierens S. Following the science? Views from scientists on government advisory boards during the COVID-19 pandemic: a qualitative interview study in five European countries. BMJ Glob Heal. 2021;6(9):1–11.
Salajan A, Tsolova S, Ciotti M, Suk JE. To what extent does evidence support decision making during infectious disease outbreaks? A scoping literature review. Evid Policy. 2020;16(3):453–75.
Article Google Scholar
Cairney P. The UK government’s COVID-19 policy: assessing evidence-informed policy analysis in real time. Br Polit. 2021;16(1):90–116.
Lancaster K, Rhodes T, Rosengarten M. Making evidence and policy in public health emergencies: lessons from COVID-19 for adaptive evidence-making and intervention. Evid Policy. 2020;16(3):477–90.
Yang K. What can COVID-19 tell us about evidence-based management? Am Rev Public Adm. 2020;50(6–7):706–12.
Parkhurst J. The politics of evidence: from evidence-based policy to the good governance of evidence. Abingdon: Routledge; 2017.
Office of the Prime Minister. Minister of Health Mandate Letter [Internet]. 2021. https://pm.gc.ca/en/mandate-letters/2021/12/16/minister-health-mandate-letter
de Faye B, Perrin D, Trumpy C. COVID-19 lessons learned review: Final report. Victoria, BC; 2022.
First Nations Health Authority. Evolving vaccination plans is science in action: Dr. Bonnie Henry. First Nations Health Authority. 2021.
BC Stats. 2021 Sub-provincial population estimates highlights. Vol. 2021. Victoria, BC; 2022.
Michael Smith Health Research BC [Internet]. 2023. healthresearchbc.ca. Accessed 25 Jan 2023.
Michael Smith Health Research BC. SRAC [Internet]. 2023. https://healthresearchbc.ca/strategic-provincial-advisory-committee-srac/ . Accessed 25 Jan 2023.
Brubacher LJ, Hasan MZ, Sriram V, Keidar S, Wu A, Cheng M, et al. Investigating the influence of institutions, politics, organizations, and governance on the COVID-19 response in British Columbia, Canada: a jurisdictional case study protocol. Heal Res Policy Syst. 2022;20(1):1–10.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101.
DeCuir-Gunby JT, Marshall PL, McCulloch AW. Developing and using a codebook for the analysis of interview data: an example from a professional development research project. Field Methods. 2011;23(2):136–55.
Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13(117):1–8.
Creswell JW, Miller DL. Determining validity in qualitative inquiry. Theory Pract. 2000;39(3):124–30.
Sackett D. How to read clinical journals: I. Why to read them and how to start reading them critically. Can Med Assoc J. 1981;1245:555–8.
Evidence Based Medicine Working Group. Evidence-based medicine: a new approach to teaching the practice of medicine. JAMA Netw. 1992;268(17):2420–5.
Allin S, Fitzpatrick T, Marchildon GP, Quesnel-Vallée A. The federal government and Canada’s COVID-19 responses: from “we’re ready, we’re prepared” to “fires are burning.” Heal Econ Policy Law. 2022;17(1):76–94.
Bollyky TJ, Hulland EN, Barber RM, Collins JK, Kiernan S, Moses M, et al. Pandemic preparedness and COVID-19: an exploratory analysis of infection and fatality rates, and contextual factors associated with preparedness in 177 countries, from Jan 1, 2020, to Sept 30, 2021. Lancet. 2022;6736(22):1–24.
Kuhlmann S, Hellström M, Ramberg U, Reiter R. Tracing divergence in crisis governance: responses to the COVID-19 pandemic in France, Germany and Sweden compared. Int Rev Adm Sci. 2021;87(3):556–75.
Haldane V, De Foo C, Abdalla SM, Jung AS, Tan M, Wu S, et al. Health systems resilience in managing the COVID-19 pandemic: lessons from 28 countries. Nat Med. 2021;27(6):964–80.
Article CAS PubMed Google Scholar
Rosella LC, Wilson K, Crowcroft NS, Chu A, Upshur R, Willison D, et al. Pandemic H1N1 in Canada and the use of evidence in developing public health policies—a policy analysis. Soc Sci Med. 2013;83:1–9.
Article PubMed PubMed Central Google Scholar
Saner M. A map of the interface between science & policy. Ottawa, Ontario; 2007. Report No.: January 1.
Lancaster K, Rhodes T. What prevents health policy being “evidence-based”? New ways to think about evidence, policy and interventions in health. Br Med Bull. 2020;135(1):38–49.
Brownson RC, Fielding JE, Maylahn CM. Evidence-based public health: a fundamental concept for public health practice. Annu Rev Public Health. 2009;30:175–201.
Rychetnik L, Frommer M, Hawe P, Shiell A. Criteria for evaluating evidence on public health interventions. J Epidemiol Community Health. 2002;56:119–27.
Article CAS PubMed PubMed Central Google Scholar
Khan Y, Brown A, Shannon T, Gibson J, Généreux M, Henry B, et al. Public health emergency preparedness: a framework to promote resilience. BMC Public Health. 2018;18(1):1–16.
COVID-19 Evidence Network to Support Decision-Making. COVID-END [Internet]. 2023. https://www.mcmasterforum.org/networks/covid-end . Accessed 25 Jan 2023.
Canadian Institutes of Health Research. Moving forward from the COVID-19 pandemic: 10 opportunities for strengthening Canada’s public health systems. 2022.
Di Ruggiero E, Bhatia D, Umar I, Arpin E, Champagne C, Clavier C, et al. Governing for the public’s health: Governance options for a strengthened and renewed public health system in Canada. 2022.
Adjoa Kumah E, McSherry R, Bettany-Saltikov J, Hamilton S, Hogg J, Whittaker V, et al. Evidence-informed practice versus evidence-based practice educational interventions for improving knowledge, attitudes, understanding, and behavior toward the application of evidence into practice: a comprehensive systematic review of undergraduate studen. Campbell Syst Rev. 2019;15(e1015):1–19.
Download references
Acknowledgements
We would like to extend our gratitude to current and former members of the University of British Columbia Working Group on Health Systems Response to COVID-19 who contributed to various aspects of this study, including Shelly Keidar, Kristina Jenei, Sydney Whiteford, Dr. Md Zabir Hasan, Dr. David M. Patrick, Dr. Maxwell Cameron, Mahrukh Zahid, Dr. Yoel Kornreich, Dr. Tammi Whelan, Austin Wu, Shivangi Khanna, and Candice Ruck.
Financial support for this work was generously provided by the University of British Columbia's Faculty of Medicine (Grant No. GR004683) and Peter Wall Institute for Advanced Studies (Grant No. GR016648), as well as a Canadian Institutes of Health Research Operating Grant (Grant No. GR019157). These funding bodies were not involved in the design of the study, the collection, analysis or interpretation of data, or in the writing of this manuscript.
Author information
Authors and affiliations.
School of Population and Public Health, University of British Columbia, Vancouver, Canada
Laura Jane Brubacher, Chris Y. Lovato, Veena Sriram, Michael Cheng & Peter Berman
School of Public Health Sciences, University of Waterloo, Waterloo, Canada
Laura Jane Brubacher
School of Public Policy and Global Affairs, University of British Columbia, Vancouver, Canada
Veena Sriram
You can also search for this author in PubMed Google Scholar
Contributions
CYL, PB, and VS obtained funding for and designed the study. LJB, MC, and PB conducted data collection. LJB and VS analyzed the qualitative data. CYL and LJB collaboratively wrote the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Laura Jane Brubacher .
Ethics declarations
Ethics approval and consent to participate.
This case study received the approval of the UBC Behavioural Research Ethics Board (Certificate # H20-02136). Participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Semi-structured interview guide [* = questions used for this specific study]
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Brubacher, L.J., Lovato, C.Y., Sriram, V. et al. The use of evidence to guide decision-making during the COVID-19 pandemic: divergent perspectives from a qualitative case study in British Columbia, Canada. Health Res Policy Sys 22 , 66 (2024). https://doi.org/10.1186/s12961-024-01146-2
Download citation
Received : 08 February 2023
Accepted : 29 April 2024
Published : 03 June 2024
DOI : https://doi.org/10.1186/s12961-024-01146-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Decision-making
- Public health
- Policy-making
- Qualitative
Health Research Policy and Systems
ISSN: 1478-4505
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Open access
- Published: 07 June 2024
Experiences of co-producing person-centred and cohesive clinical pathways in the national system for knowledge-based management in Swedish healthcare: a qualitative study
- Sylvia Määttä 1 ,
- Christina Petersson 2 ,
- Boel Andersson Gäre 3 ,
- Göran Henriks 4 ,
- Henrik Ånfors 5 ,
- Christin Lundberg 6 &
- Ylva Nilsagård 7
Research Involvement and Engagement volume 10 , Article number: 55 ( 2024 ) Cite this article
22 Accesses
Metrics details
When the 21 Swedish county councils decided to collaborate in the creation of a national system for knowledge-based management, patient participation was mandatory. Patient and next-of-kin representatives (PR) co-produced person-centred and cohesive clinical pathways together with healthcare professionals (HPR). Research on co-production in healthcare at the national level is scarce. The aim of this study is to explore experiences of patient participation from the perspectives of both PRs and HPRs when co-producing clinical pathways within the Swedish nationwide healthcare system for knowledge-based management.
A qualitative study was conducted. A strategic sample of nine PRs and eight HPRs were interviewed individually between August 2022 and January 2023 using a semi-structured interview guide. We analysed data using an inductive content analysis.
Three main categories were identified: (1) Finding appropriate patient representativeness; (2) Working methods that facilitate a patient perspective; and (3) Influence of the patient perspective in the clinical pathways.
Conclusions
The study demonstrates the importance of patient and next-of-kin participation in the construction of clinical pathways at the national level. The results provide a platform for further research on patient participation on the national level and add to studies on if and how patient participation on this level has an impact on how the clinical pathways are put into practice at the micro level, and the support provided at the meso level. The study contributes to the growing body of literature studying patient participation and co-production.
Trial registration
Region Örebro County ID 276,940. An advisory opinion was obtained from the Swedish Ethical Review Authority (2021-05899-01).
Plain english summary
Co-production of guidelines and clinical pathways with patients and next-of-kin representatives is increasingly emphasised at different levels in healthcare internationally. However, little has been documented and explored regarding experiences of patient participation on a national level. Patient participation was mandatory when a national system for knowledge-based management of healthcare was launched in Sweden. Knowledge management of healthcare is the collection of methods relating to creating, sharing, using and managing the knowledge and information of an organization. All 21 of Sweden’s regions and the government have supported this collaborative system consisting of multi-professional national working groups with patient representatives. The groups develop clinical pathways aiming to enhance a coordinated, equal and effective healthcare. The person-centred clinical pathways describe assessment, diagnosis, planning and evaluation for a condition, for example for patients with a hip fracture, or congestive heart failure. The study focuses on experiences of patient participation in the national working groups. We interviewed nine patient representatives and eight healthcare professional representatives from eleven different groups. Our findings show the importance of identifying and finding appropriate patient representativeness, having working methods that facilitate a patient perspective and the patient perspective influencing the clinical pathways. This study on patient participation in the construction of clinical pathways at the national level contributes to the growing body of literature on co-production of knowledge support. The findings highlight important learning for the continued development of meaningful patient participation on the national level. It also raises curiosity on how the national approach with co-production influences local levels where the guidelines are used.
Peer Review reports
Increasingly, co-production between patients, their next-of-kin and healthcare professionals is emphasised to achieve safer and more person-centred health, healthcare and health science [ 1 , 2 , 3 , 4 ]. Co-production is defined by Batalden [ 5 ] as “the interdependent work of users and professionals who are creating, designing, producing, delivering, assessing, and evaluating the relationships and actions that contribute to the health of individuals and populations”. Co-production has many applications [ 6 ] and is here used as an umbrella term, covering a range of “co”-words, for example co-design and co-creation between patients and healthcare professionals (for a discussion on concepts used, see e.g. [ 5 , 7 , 8 ]). .
There is a lack of consensus on the relations between the terms used to describe patient participation in co-production. Terms such as patient involvement, patient engagement and shared decision-making can be discerned, among others [ 9 , 10 , 11 , 12 ]. A suggested linking of the terms was presented by [ 13 ] Hedberg et al., which can be further discussed. In addition, the level on which patient participation takes place is often blurred. Inspired by Arnstein’s classical description of a ladder of citizen participation [ 14 ], Carman et al. [ 15 ] designed a model for patient participation at micro, meso and macro levels that often is used in the context of patient participation [ 9 , 16 ]. Care meetings between patients and healthcare professionals occur at the micro level. At the meso level, patients and their next-of-kin may participate in teams working with quality improvement of healthcare services. At the macro level – hereafter termed the national level – patients can participate in co-producing national care programmes, guidelines, and clinical pathways [ 17 ].
In this article the concept of “patient participation” is used, referring to the participation of a person with lived experiences of a health issue or condition, and the term “patient representative” (PR) is used for patients representing others with experiences of the same condition or who are next-of-kin to a person with a certain condition [ 18 ].
Patient participation at the swedish national level
Although Swedish healthcare has a high standard, there is room for improvement. Despite primarily being funded by general taxation, there are examples where Swedish healthcare does not succeed in providing equal care and equal access to healthcare services for the whole population. This challenge of inequity was one of the drivers for the development of the knowledge-based management system. The responsibility for legislation, monitoring, education, and training of healthcare professionals lies at the national level. The responsibility for both specialised healthcare and primary healthcare services rests on the 21 regional councils, while the 290 municipalities are responsible for long-term care for older people and persons with disabilities. The regional councils are combined into six larger healthcare regions to enhance an efficient use of resources through cooperation.
In 2017, the regional councils received a recommendation to sign an agreement for a cohesive system for knowledge-based management [ 19 ]. The system was inspired by the Intermountain Healthcare system (the largest nonprofit health system in the Intermountain West, United States) [ 20 ] and formulated in accordance with Swedish healthcare laws [ 21 ]. The shared vision is: “We count our success in lives and equal health and make each other successful”. The system includes interplaying micro, meso and macro levels and is based on the interaction between knowledge support and support for follow-up, open comparison, analysis, leadership, and development (see Fig. 1 ). SALAR is an employer organisation and an organisation that represents and advocates local government in Sweden. All of Sweden’s municipalities and healthcare regions own and are members of SALAR.
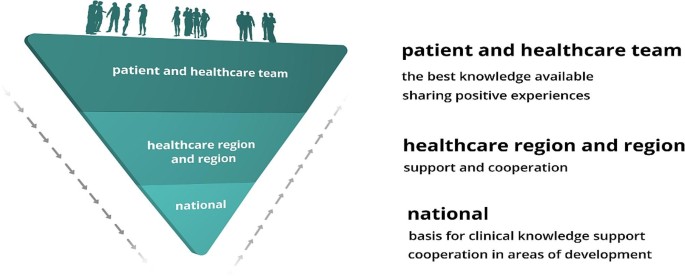
The interplay between micro (team), meso and macro system levels in the Swedish national system for knowledge-based management (figure printed with permission from SALAR’s administrative function)
Patient participation has from the start been considered a vital part of the system. At the national level, patient representatives and healthcare professional representatives participate in national working groups to co-produce person-centred and cohesive clinical pathways. The clinical pathways portrayed here, which will be described more later, focus on major diagnoses, intending to meet the challenges that Swedish healthcare is facing and to support a nationwide person-centred, cohesive, effective, and equal healthcare.
Knowledge gap
The impact of patient participation in research and quality improvement projects at the micro and meso levels are explored to some extent [ 22 , 23 , 24 , 25 , 26 ]. However, healthcare professionals and patient representatives jointly constructing clinical pathways is a significant but less studied strategy. To our knowledge, empirical research that addresses how patient participation is experienced by patient representatives and healthcare professional representatives on a national level is scarce. It is important to study since experiences of patient participation at this level may influence future national, regional, and local initiatives. Consequently, the aim of this study is to explore experiences of patient participation from the perspectives of both patient and healthcare professional representatives when co-producing clinical pathways. The context is within the nationwide system for knowledge-based management of Swedish healthcare and if participants expressed that their participation influenced the end-products.
Study design
We conducted a qualitative study, using an inductive content analysis following Elo and Kyngäs [ 27 ].
Study context
The working groups in the national system of knowledge-based management constitute the context of this study. In addition to being maintained by the regions, the system has been supported by the Swedish government with a total of 90 million euros. Hosted by the six larger healthcare regions, 26 national programme groups have been established, addressing for example infectious diseases, diseases of the nervous system, and lung- and allergy diseases. Each programme group identifies conditions that could benefit from a clinical pathway and recommends starting a national multi-professional and multi-disciplinary working group that they will supervise.
A national working group produces national clinical pathways aiming to be implemented at the micro level. A clinical pathway describes assessment, diagnosis, planning, and evaluation for a specific condition. A description of the pathway from the patient perspective is mandatory. After going through an open referral process, the clinical pathways are approved for implementation throughout Swedish healthcare by the steering committee of the national system. They are presented at open digital seminars and published on a website. The meso level supports both the national and the local (micro) level as an intermediary [ 28 ]. It is the responsibility of each regional council to decide when and how the clinical pathways are put to action locally.
The larger healthcare regions, municipalities and professional organisations are invited by the national programme groups to nominate healthcare personnel to the national working groups. The nomination procedure includes a specific requirement of formal competences and disclosing conflicts of interest. Patient representatives are also recruited to the groups according to the policy and guideline for patient participation that was launched in the development of the system at an early stage, stressing that there should be at least one patient representative in each group, preferably from a national patient organisation [ 19 ]. It also states the level of remuneration to the participating patient representatives. At present, there is no formal request for a specific profile or competence of these representatives. The national programme group finally determines the composition of the working group and appoints both patient representatives and other members of the group. The national working groups are led by a chairperson and a process leader.
During the process of producing a clinical pathway, support is provided by the chairperson, the process leader, and the national administrative function for the system at SALAR (see Table 1 ).
Participant selection for the study
Strategic sampling was used in the study [ 29 ]. To give a broad picture of patient participation, eligible informants needed to have experience of participating in national working groups producing clinical pathways for (1) acute or chronic conditions, as well as groups that had been (2) working together for a shorter or longer period. Patient representatives, chairpersons and process leaders in the national working groups were invited to participate in the study. Eligible informants were approached and invited by email. In the email, the aim of the study was explained and, if informants were interested in being interviewed, a time for a digital interview was suggested. Informants answered by email and a digital link was sent. Informed consent was required.
The informants were encouraged to find an undisturbed, quiet place of their choice when participating in the interview. We invited nine patient representatives and nine healthcare professional representatives, of which one declined participation due to lack of time.
The final sample thus consisted of 17 informants: nine patient representatives (3 males) and eight healthcare professional representatives (3 males) (two chairpersons and six process leaders). As described above, strategic sampling was used to give a broad picture of the experiences of patient participation. During the study period several national working groups (with approximately 12–17 participants in each working group) were on-going, producing clinical pathways. 3 of the 6 clinical pathways that were finalised in 2020, 4 in the 6 that were finalised in 2021 and 5 in the 12 that were finalised in 2022 were represented in the study. Informants represented 18 different national working groups, related to 11 national programme groups working with a variety of acute and chronic diseases.
Data collection
All interviews were undertaken in an online video session, conducted in Swedish and guided by a semi-structured interview guide with open questions followed by explanatory questions to gain a deeper understanding; see additional files for the interview guide for patient (Appendix 1) and healthcare professional representatives (Appendix 2). The interview guide was iteratively discussed and refined in the research group, including two patient representatives who were not part of the interviews that followed.
Informants were encouraged to speak openly and share their perceptions and experiences. To deepen the dialogue, probing questions were posed: “Could you elaborate on that?” and “Can you give an example?”. The interviews were audio-visually recorded and transcribed verbatim. All interviews were undertaken between August 2022 and January 2023. The duration of the interviews was approximately 30 to 45 min.
Data analysis
Data were analysed using inductive qualitative content analysis, moving from the specific to the general to develop categories that describe the phenomenon [ 27 ]. The transcribed interviews were analysed by going back and forth in the transcriptions. An individual code was given to each informant to be able to identify their specific role: patient or next-of-kin representative, or healthcare professional representative.
The analysis began with a first round of the authors (SM, CP and YN) listening to all audio-recorded interviews and then reading all transcripts to gain a sense of the whole. In this preparatory phase, units of analysis were selected. A unit of analysis was determined to be one or more sentences, or part of a sentence, that described something related to any of the research questions asked. Then, open codes were created while reading the transcripts together (manifest) and organising the data by identifying categories and creating a first set of generic categories (abstraction). In the second round, all preliminary generic categories were discussed together with three other authors (HÅ, GH and BAG), which led to merging, dividing, and re-naming the categories initially developed. Special attention was given to potential overlaps between the generic categories. In the third round, the generic categories were discussed again with one of the authors (HÅ) and all generic categories were checked if they were coherent. All main categories were formulated and visualised through a figure, and a main category was created. Examples of the analytic process from unit of analysis to categories are described in Table 2 . Quotations capturing the data were used to illustrate the analytic process. The quotes were translated into English and then re-translated into Swedish to ensure consistency of meanings. We used Excel Office 365 to organise the data during the analysis.
This study identified three main categories in which expressions from both patient representatives and healthcare professional representatives were included. There was a conformity in the experiences shared, with a difference being that patient representatives voiced greater concern regarding the implementation and utilization of the clinical pathways.
The main categories were: (1) finding appropriate patient representativeness; (2) working methods that facilitate a patient perspective; and (3) influence of the patient perspective in the clinical pathways. The main categories prepared the way towards person-centeredness in the clinical pathways processes (see Fig. 2 ). In the following we present the main and generic categories, illustrated by quotations from the informants.

The three main categories and the generic categories
Finding appropriate patient representativeness
We identified a need to clarify prerequisites and demands in recruitment as well as formal and informal competence to find appropriate patient representativeness.
The prerequisites and demands for the recruitment of a patient representative to a national working group were unclear and not explicit. A description of the role was lacking, leading to a feeling of initially working and performing ad hoc (PR5). Not having prerequisites and demands would be equivalent to a risk of “positive special treatment”, an undemanding attitude towards the patient representatives (HPR1). Therefore, the role needed to be clarified, describing the responsibilities of patient representatives and what they were expected to do (HPR8). The remuneration offered for the assignment ought to give room for demands to be made concerning attendance and performance in the working groups (HPR1). Comparisons were made to the specified requirements that existed in the recruitment of other members: “Because we still want this [patient participation] as one of all the others … that’s where we want to get to” (HPR1).
The importance of recruiting appropriate patient representatives for patient participation in the national working groups was stressed. Recruiting from a national patient association provided uniformity in how all members are recruited as “Others in national working groups representing an organisation” (HPR1, HPR4). Recruiting patient representatives could, however, be problematic, as “… we had a hard time finding any [patient representatives] so we had to hunt a bit …” (HPR3). This could be because there was no relevant patient association for the current working group (HPR1) or because some patient groups had not formed a patient organisation, for example when having a certain disease could be experienced as stigmatising and not something you want to show off (HPR4). Recruitment could be facilitated, for example, by having more than one patient representative in a group (HPR4). Being more than one appointed representative had the advantage of being able to cover for each other. Closer contact, dialogue and collaboration with patient associations could also be useful.
Patient participation in a national working group was rather complex, demanding both formal and informal competence. Formal competence was described as patient representatives knowing how to produce material, and how to write and comment on materials that have been produced (HPR2). It was suitable to have experience of working and participating in a group (PR9) and an advantage to have worked with process development (PR3). Formal competence also consisted of being used to interviewing others and forming one’s own opinion (HPR4). Some stressed the need for formal competence of chairpersons and process leaders as well, declaring low competence and inexperience to be a difficulty when working with patient participation (HPR8).
Informal competence was based on patient representatives’ experience, compared to other group members, of being patients in Swedish healthcare and thus having “a different competence base, it is an experience-based competence base …” (HPR1). Patient representatives in the national working groups were “…extremely professional and good at calling in what, how … we can get good answers, or answers that develop care for the target group” (HPR3). Informal competence was also about being receptive, waiting for a good opportunity to describe one’s own experiences. It was “… good to be a little cool in the beginning and not to cling, … to listen …” (PR4), to blend in and be responsive (HPR4). At the beginning of the national working group’s work, it was more uncertain when “… you should go in and explain yourself” (PR1), but as the group work continued it became easier. Informal competence was also about really speaking up when needed (HPR4), listening first and not being shy to give comments and express your opinion later (PR4). Entering a group could be perceived as challenging when working together with highly trained specialists (HPR5). It was therefore important to be confident in oneself, brave and tough, daring to take one’s place (HPR5) and to “… realise that experience is also competence” (PR8). Being a patient representative in a national working group contributed to the development of care, personal development and a greater understanding of the challenges, obstacles and opportunities in health care (PR4).
Working methods that facilitate a patient perspective
This main category discerned that a patient perspective was facilitated by group members’ interaction . It showed the importance of how one represents , strategies to support participation , meeting forms , learning from each other , and getting support from SALAR .
Group members’ interactions contributed to creating a good climate in the national working groups. There was a friendly tone in the groups, all members had room to speak, patient representatives were listened to and the “personal chemistry was right” (PR3, PR4). In the groups, patient representatives were met by civil discourse and respect (PR1, PR6, PR7, PR9) and felt included (PR1, PR9). Initially some patient representatives experienced feeling inferior in the company of well-educated and well-known professionals: “Of course, you get a little bit star struck when you see the list of participants” (PR4), but rules for group interactions, for example to avoid unnecessary medical language and abbreviations (PR8), led to an experience of feeling equal. Group members being open with their knowledge added to the experience of equality and of “being players at the same level” (PR4). The patient representatives’ interaction in the group was increased by all members having the same focus, namely, to improve healthcare for the patients (PR6). They were more active when the group was divided into smaller groups (PR1, PR8) and when they took part in planning a group meeting (PR8).
Patient participation in the national working groups was multifaceted. The representatives had to represent both their own experience and that of others and have a double perspective: “you don’t represent yourself as a patient or a close relative, of course you contribute with your experiences, that’s how it is, but you also have a task anchor the current work with [those] affected in the network” (HPR7). The double perspective was important to consider when recruiting patient representatives (HPR2, HPR4). Signs of having a double perspective were, for example, saying “we” instead of “I”: “It also signals that she knows others who have been in the same situation, so that in some way she is perceived by the group as actually representing the entire patient group, not just herself” (HPR4). It was also important to have the know-how for which of the two perspectives should be put forward: “Because it is a balancing act right here and the difficulty for the patient representatives to share their own experience but also put a limit where … yes where is the limit for my own … so to speak, commitment, and my own experience linked to the patient group that one represents” (HPR7).
The double perspective was promoted by taking a broader, generalised role, representing all categories of patients, and thinking “… how is it for other patients and not just for me” (PR5). This perspective could be obtained in several ways. Some based the work in the national working group by discussing with the relevant patient organisations (PR1, PR6), with different types of networks (HPR7), Facebook groups (PR5) or interviews with members in relevant patient organisations (PR5). Establishing their own opinion with a broader group as reference point gave a sense of self-assurance (PR8) and made it easier to take responsibility for their contributions to the content in the clinical pathway (PR6).
Patient participation was strengthened by a variety of strategies. Healthcare professional representatives had separate meetings with the patient representatives, digitally, by telephone and email contact, where they offered information and could ask questions and reflect on their experiences of working in the national working group (HPR6). During the group’s working meetings, one strategy was to divide the group into smaller ones. Another was an inviting strategy to include and involve patient representatives. This was done, for example, by directing specific questions to them: “Do you have something to say here? You can also write something in the chat …” (HPR2). The inviting strategy was important for patient representatives to feel welcomed in the group (PR8). This strategy was especially important if the discussion among other members became too medically oriented (HPR2). Another strategy was to help patient representatives not to overemphasise and talk too much about their own experiences (HPR1). If such a situation occurred, they were supported by “leading them [the PRs] away” from their own medical histories and their own diagnoses (HPR2).
The meeting forms in the national working groups varied and were conducted physically and digitally. Physical meetings gave room to get to know one another better compared to meeting via digital platforms. For some, an introductory meeting was held physically, giving them the chance to get to know one another and to ask questions about the assignment (PR6). At a physical meeting, more questions can be asked (PR2). Due to the restrictions surrounding the COVID-19 pandemic, however, the physical meetings switched to digital ones. For some patient representatives, all working group meetings were digital. During digital meetings, they did not want to interrupt and ask, “beginner questions” (PR3). However, digital meetings were time saving as participants in the working groups came from all over the country (PR7). Forming small groups digitally could slightly compensate as a way for group members to get to know each other better and a way for the knowledge and opinions of patient representatives to be expressed in a better way (PR1).
Patient participation in national working groups enhanced learning for both healthcare professional and patient representatives. The latter gained deeper knowledge both on the specific disease and on scientific matters. Participation in the group opened a new world for them, for example by grasping the complexity of healthcare (PR1, PR2, PR3). They also learned from other patient representatives. In working groups with two or more patient representatives, they supported each other, which increased the weight of their arguments and made them stronger (PR6, PR7, PR8). Being a patient representative in a working group together with a more experienced patient representative was experienced as boosting (PR4). They were often interconnected and had the same opinion but could also speak up if they had different thoughts on a specific matter (PR4). Healthcare professional representatives also learned from the patient representatives, for example, “to get feedback and have a dialogue with the patient representatives, what has been good, what has been less good, what can we develop further and do better. I feel that I have learned from the participants” (HPR7).
The SALAR administrative support function’s knowledge on the details in the reimbursement system was considered important (HPR2) and supporting materials, for example films that described what it is like to participate in a national working group, were helpful to provide an understanding of the role as patient representative (HPR2). Supporting materials were used especially when process leaders and chairpersons were new to their roles (HPR2). The support for patient participation could be further improved by involving professional communicators in the process at an early stage (PR7), and by, for example, improving the process of disclosing conflicts of interest (PR5). Patient representatives sought feedback and input from the administrative support function regarding the outcomes of the clinical pathways implementation and how it could improve healthcare overall. (PR7).
Influence of the patient perspective in the clinical pathways
This main category showed that both working group meetings and the clinical pathways were influenced by the input from the patient representatives and that patient participation contributed to enhancing a patient perspective .
Patient representatives thought that their experiences and views received attention and were integrated into the work, and that they had contributed to the clinical pathways both in the working process and in the final text (PR4). The ability to influence the clinical pathways and hence contribute to equal care was considered important (PR1). Patient representatives had also led to changes in decisions on the scope of clinical pathways (HPR4) and to changes in the title of the clinical pathways.
The ability to influence was initially limited in the working process but increased with time (PR1). The patient representatives’ statements and utterances sometimes had a strong and convincing effect: “When they say something, the group stops. It’s not that a nurse or a doctor doesn’t know what civil discourse is. But when a patient representative says it, it becomes truth in a different way” (HPR1). The patient representatives’ utterances were more influential, compared to the professionals’ (HPR8). Patient experiences worked as something of an eye-opener; what was obvious to the patients was not so obvious to the healthcare professionals (HPR4, HPR5). Patient representatives came up with aspects that the professionals never had considered or even thought of (PR7). Besides participating in national working groups, patient representatives contributed to national information meetings describing the clinical pathways (HPR7), but worried about the readiness for implementation in the regions (PR1). They were surprised that healthcare was performed differently in different parts of the country and therefore considered it valuable to have national clinical pathways covering all Swedish regions (PR4). However, patient representatives feared that the work invested would be wasted and that the clinical pathways would become another piece of paper that was not used or did not result in equal care (PR6).
Patient participation in the national working groups gave healthcare professional representatives a deeper understanding of the patient representatives’ work in developing clinical pathways. Their participation had worked well and including them in the working group was seen as an expression of person-centeredness. Patient representatives were considered brave, bringing forward their experiences in such a way that other participants in the working groups were impressed (HPR5). The value of patient representatives participating in producing clinical pathways was evident as these were intended as a knowledge base for healthcare meetings, in which the patient is a partner (HPR3, HPR7): “You cannot have a national working group without patient representatives, in the same way that you cannot work with person-centeredness without participation of the people to whom the clinical pathway is addressed” (HPR2). Patient participation in the national working groups contributed to healthcare personnel moving from an organisational perspective to a patient perspective (HPR8).
This study of patient participation when co-producing person-centred and cohesive clinical pathways at the national level contributes to the growing body of literature studying patient participation [ 17 , 30 ]. We identified three main categories which add to our knowledge of what to expect and consider when using patient representatives in the development of clinical pathways.
One main category shows the importance of a careful recruitment process, demanding formal requirements and informal competence of the potential patient representatives. Notably, both patient and healthcare professional representatives emphasise the importance of a clear structure for reimbursement and requirement profile for patient representatives in the national working groups. This study demonstrates the unique competence of the patient representatives. The competence to represent a dual perspective – to speak for oneself and for others – places high demands on patient representatives at the national level, which also applies to all participants in the national working group. The need for a dual perspective could benefit from being made more explicit to all participants.
The second main category shows the importance of healthcare professional representatives’ strategies for strengthening patient participation. Before and during working group meetings, they can support patient representatives in dealing with the dual perspective and balancing when one or the other perspective should be in the foreground. It is likely that their efforts to achieve a sound balance and interaction within the groups mattered. Another strategy to strengthen patient participation might also be to offer them support through the exchange of experiences with other patient representatives, for example in network meetings and through mentorship from more experienced patient representatives. It is also interesting that several of the patient representatives emphasised the advantage of being at least two in a group, indicating that they might experience subordination, perhaps a feeling of imbalance in the number of representatives and maybe also in knowledge.
The learning that takes place within the working groups is important. The organisational support for patient participation at SALAR was not developed in detail when the system first started but has evolved and improved over time. Over the years, routines for how to work with patient participation have been developed, built on the experiences of the national working groups, which strengthens the point that the system works as a “learning health organisation”. According to Elwyn et al. [ 1 ], there is a connection between co-production with the voice of the patient and practice improvement and organisational design. The idea of co-production could contribute to the idea of a learning health system [ 6 ], which is a goal of the national system for knowledge-based management.
The third main category shows that patient representatives’ experiences are expressed in the finalised clinical pathways. Their contribution to the mandatory patient pathway was necessary to achieve credibility. It also shows that it is vital to include patient participation in the national working groups to promote person-centeredness. As mentioned before, enhancing person-centred care is a goal of the national system. However, person-centred care is a debated concept that has been described as vague, multi-faceted and not well-defined, lacking a precise definition [ 31 ]. Person-centred care can be narrowed down to three aspects: (a) understanding patients’ experience of illness and their life situation, (b) the professional’s relationship with the patient, and (c) the coordination of care. An updated “definition of patient-centred care and its operationalization can make its implementation in healthcare more manageable” [ 31 ]. Patient participation in national working groups contributes to these aspects by integrating the unique knowledge of patient representatives’ lived experience, the relationships with the professionals and the encounters with the total healthcare system into the clinical pathways. With co-production, the risks of fragmented healthcare and barriers to accessing healthcare services can be identified, and awareness of the pitfalls in coordinated care can increase [ 18 ].
The study shows that the system is developing when it comes to patient participation. This study contributes to further developing how patient participation can be enhanced. It can add to the adoption of the principles of co-production in healthcare, which is still slow [ 1 ]. We also see the possibility for the system to take advantage of the results of patient participation on all levels of healthcare, in accordance with Carman et al., on micro, meso and macro levels [ 15 ].
Methodological considerations
A strength of this study is that both patient and healthcare professional representatives acting at a national level were interviewed, which seems quite rare in the literature [ 28 ]. The study uses an interactive approach where the process of joint learning is central [33]. Patient representatives included in the research group took part in every step of the research process throughout the project. Their input led to revisions of the semi-structured interview guides, thereby increasing the relevance of the questions asked. The feasibility of the data collection methods was discussed and enhanced jointly, and the patient representatives checked the coding and took part in grouping the categories under higher order headings. Working interactively contributed to learning more about patient participation throughout the process.
Using qualitative methods allowed for asking the informants probing questions that would not have been possible in questionnaires. We were able to include informants strategically, as intended, with a broad variety of informants working in a wide range of national working groups to reflect the system. This should strengthen the transferability of the results. We initially planned to include approximately ten patient and ten healthcare professional representatives, considering the extent, specificity and theoretical connection of the aim and previous experience of the research team. Theoretical saturation was reached after having included nine patient representatives and eight healthcare professional representatives, respectively. A limitation of the study is that only chairpersons and process leaders in national working groups were interviewed. Hence, an area for further research is to also include other group members.
Individual interviews allowed the informants to freely express their experiences. The interviews were led by two researchers (CP or SM). One researcher conducted. the interview, while the other researcher ensured that all questions outlined in the interview guide was covered and provided prompting questions to help clarify the participant’s descriptions [ 32 ].
An inductive approach to analysing the data was found appropriate since patient participation at system level is less explored. Digital interviews may be seen as a drawback. However, our experience as researchers and reviewers is that digital contacts have been more common since the start of the COVID-19 pandemic. Digital recordings enabled the third researcher involved in the analyses not only to listen to audio recordings and read transcripts, but also to observe mimics and body language. One of the researchers had a deeper pre-understanding of the informants due to her previous work at the national administrative support function. There is always a risk that this would cause the informants to be more cautious about expressing criticism in their feedback, however nothing in the interviews indicated that this was the case. The pre-understanding of the system can also add to a deeper understanding. Credibility further increased by having all members of the research group, including patient representatives, checking, and discussing all steps in the analysis. The link between the data and the analytical steps with authentic quotations also supported the findings to increase the reliability of the interpretation of the data.
This study shows the importance of patient representatives’ participation in the co-production of clinical pathways. Patient participation takes time to develop into co-production. To achieve an impact, a thoughtful recruitment process considering the dual perspective, that is, to represent oneself and others, should be considered. Likewise, actions to strengthen the interactions in the working groups can help the patient representatives’ competence to come to the fore.
Experiences of patient participation in the development of clinical pathways on the national level can also be helpful when the clinical pathways are implemented in the actual care, that is, at the micro level. The findings in this study provide a platform for further research, for example for observational studies of interactions in the working groups as well as studies on the interplay between the different levels of the care system when the guidelines for clinical pathways are to be used systematically at the local level.
In this study, patient representatives took part in the planning, analysis, and the final version of publication phase of the research project. This was important as the initial research questions were refined and developed, and the categories were constructed jointly.
Key learnings and practical implications
Clarifying requirements regarding patient representatives’ formal and informal competence may facilitate the recruitment process.
There is room for improvement of methods and tools to enhance patient representatives’ competence to represent others.
Patient representatives’ participation is supported by initial physical meetings.
Representation from a patient organisation enables broad perspectives for patient representatives’ participation.
More than one patient representative is recommended in each group.
The strategies and competence of process leaders and chairpersons to lead a group are important to facilitate patient participation.
Patient participation is enhanced by administrative support to coordinate patient representative meetings for learning and exchanging experiences.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
patient representative
healthcare professional representative
The Swedish Association of Local Authorities and Regions
Elwyn G, Nelson E, Hager A, Price A. Coproduction: when users define quality. BMJ Qual Saf. 2020;29(9):711–6.
Article PubMed Google Scholar
Holmes L, Cresswell K, Williams S, Parsons S, Keane A, Wilson C, et al. Innovating public engagement and patient involvement through strategic collaboration and practice. Res Involv Engagem. 2019;5:30.
Article PubMed PubMed Central Google Scholar
Lee-Foon NK, Smith M, Greene SM, Kuluski K, Reid RJ. Positioning patients to partner: exploring ways to better integrate patient involvement in the learning health systems. Res Involv Engagem. 2023;9(1):51.
Malterud K, Elvbakken KT. Patients participating as co-researchers in health research: a systematic review of outcomes and experiences. Scand J Public Health. 2020;48(6):617–28.
Batalden P. Getting more health from healthcare: quality improvement must acknowledge patient coproduction-an essay by Paul Batalden. BMJ. 2018;362(k:3617):4.
Google Scholar
Gremyr A, Andersson Gäre B, Thor J, Elwyn G, Batalden P, Andersson AC. The role of co-production in Learning Health systems. Int J Qual Health Care. 2021;33(Supplement2):ii26–32.
Batalden M, Batalden P, Margolis P, Seid M, Armstrong G, Opipari-Arrigan L, et al. Coproduction of healthcare service. BMJ Qual Saf. 2016;25(7):509–17.
Masterson D, Areskoug Josefsson K, Robert G, Nylander E, Kjellström S. Mapping definitions of co-production and co-design in health and social care: a systematic scoping review providing lessons for the future. Health Expect. 2022;25(3):902–13.
Bergerum C, Engström AK, Thor J, Wolmesjö M. Patient involvement in quality improvement - a ‘tug of war’ or a dialogue in a learning process to improve healthcare? BMC Health Serv Res. 2020;20(1):1115.
Bombard Y, Baker GR, Orlando E, Fancott C, Bhatia P, Casalino S, et al. Engaging patients to improve quality of care: a systematic review. Implement Sci. 2018;13(1):98.
Eldh AC, Holmefur M, Luhr K, Wenemark M. Assessing and reporting patient participation by means of patient preferences and experiences. BMC Health Serv Res. 2020;20(1):702.
Halabi IO, Scholtes B, Voz B, Gillain N, Durieux N, Odero A, et al. Patient participation and related concepts: a scoping review on their dimensional composition. Patient Educ Couns. 2020;103(1):5–14.
Hedberg B, Wijk H, Andersson Gäre B, Petersson C. Shared decision-making and person-centred care in Sweden: exploring coproduction of health and social care services. Z Evid Fortbild Qual Gesundhwes. 2022;171:129–34.
Arnstein S. A ladder of citizen participation. J Am Iinstitute Planners. 1969;35(4):9.
Carman KL, Dardess P, Maurer M, Sofaer S, Adams K, Bechtel C, et al. Patient and family engagement: a framework for understanding the elements and developing interventions and policies. Health Aff (Millwood). 2013;32(2):223–31.
Ocloo J, Matthews R. From tokenism to empowerment: progressing patient and public involvement in healthcare improvement. BMJ Qual Saf. 2016;25(8):626–32.
Strålin K, Linder A, Brink M, Benjaminsson-Nyberg P, Svefors J, Bengtsson-Toni M, et al. Design of a national patient-centred clinical pathway for sepsis in Sweden. Infect Dis (Lond). 2023;55(10):716–24.
Eriksson EM. Representative co-production: broadening the scope of the public service logic. Public Manage Rev. 2018;21(2):24.
Sveriges Kommuner och Regioner. Nationellt system för Kunskapsstyrning [homepage on the Internet]. https://skr.se/skr/halsasjukvard/utvecklingavverksamhet/systemforkunskapsstyrning.48276.html : Sveriges Kommuner och Regioner; 2021 [cited 2021 June 7th 2021]. Available from: https://skr.se/skr/halsasjukvard/utvecklingavverksamhet/systemforkunskapsstyrning.48276.html.
Cosgrove DM, Fisher M, Gabow P, Gottlieb G, Halvorson GC, James BC, et al. Ten strategies to lower costs, improve quality, and engage patients: the view from leading health system CEOs. Health Aff (Millwood). 2013;32(2):321–7.
Socialdepartementet. Hälso- Och sjukvårdslag. SFS. 2017;2017:30.
Gustavsson SM. Improvements in neonatal care; using experience-based co-design. Int J Health Care Qual Assur. 2014;27(5):427–38.
Jackson T, Pinnock H, Liew SM, Horne E, Ehrlich E, Fulton O, et al. Patient and public involvement in research: from tokenistic box ticking to valued team members. BMC Med. 2020;18(1):79.
Article CAS PubMed PubMed Central Google Scholar
Liang L, Cako A, Urquhart R, Straus SE, Wodchis WP, Baker GR, et al. Patient engagement in hospital health service planning and improvement: a scoping review. BMJ Open. 2018;8(1):e018263.
Pomey M-P, Hihat M, Néron PL, Dumez A. Patient partnership inequality improvement of healthcare services. Patient Experience J. 2015;2(1):14.
Article Google Scholar
Sheard L, Marsh C, O’Hara J, Armitage G, Wright J, Lawton R. The patient Feedback Response Framework - understanding why UK Hospital staff find it difficult to make improvements based on patient feedback: a qualitative study. Soc Sci Med. 2017;178:19–27.
Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62(1):107–15.
Elg M, Gremyr I. Patient involvement in quality improvement: a survey comparing naturalistic and reflective approaches. BMJ Open Qual 2023;12(2).
Robinson OC. Sampling in interview-based qualitative research: a theoretical and practical guide. Qual Res Psychol. 2014;11(1):25–41.
Lachman P, Nelson EC. Policy, accreditation and leadership: creating the conditions for effective coproduction of health, healthcare and science. Int J Qual Health Care. 2021;33(Supplement2):ii1–3.
Mitchell P, Cribb A, Entwistle V. Vagueness and variety in person-centred care. Wellcome Open Res. 2022;7:170.
Ellström P-E, Elg M, Wallo A, Berglund M, Kock H. Interactive research: concepts, contributions and challenges. J Manuf Technol Manage. 2020;31(8):20.
Download references
Acknowledgments
We would like to extend our gratitude to all contributors that have been involved to make this study possible.
Open access funding provided by Jönköping University. Language review was supported by Örebro University. Open access funding provided by Jönköping Academy for Improvement of Health and Welfare, Jönköping University. This work is supported by grants from the Research Committee in Region Örebro County, Sweden (OLL-977423). The funding body will are not involved in the study’s design, collection, analysis and interpretation of data, or writing of the manuscript.
Open access funding provided by Jönköping University.
Author information
Authors and affiliations.
Institute of Health and Care Sciences, Sahlgrenska Academy, Gothenburg University, Gothenburg, Sweden
Sylvia Määttä
Jönköping Academy for Improvement of Health and Welfare, Jönköping University, Center for Learning and Innovation at Region Jönköping County, Sweden, Sweden
Christina Petersson
Jönköping Academy for Improvement of Health and Welfare, Jönköping University, Sweden and Futurum, Region Jönköping County, Jönköping, Sweden
Boel Andersson Gäre
Yerevan State University, Strategic Advisor Region Jönköping County, Yerevan, Sweden
Göran Henriks
Qulturum – Center for Learning and Innovation, Region Jönköping County, Jönköping, Sweden
Henrik Ånfors
Region Västra Götaland, Gothenburg, Sweden
Christin Lundberg
University Healthcare Research Centre, Faculty of Medicine and Health, Örebro University, Örebro, Sweden
Ylva Nilsagård
You can also search for this author in PubMed Google Scholar
Contributions
Study design: SM, CP, YN, HÅ, GH and BAG; data collection: SM and CP; data analysis: first round (SM, CP and YN), second round (SM, CP, YN, HÅ, CL, GH and BAG) and third round (SM, CP, YN and HÅ). Manuscript drafting, main responsibility: SM, CP and YN. Interactive feedback from all in the research group. All authors approved the final draft.
Corresponding author
Correspondence to Christina Petersson .
Ethics declarations
This study is part of a project studying patient participation at a systemic level. The Swedish Ethical Review Authority approved the study (DN 2021-05899-01).
Competing interests
The authors declare no competing interests.
All authors have given their consent to the final version for publication. All participants have given their consent to participate in the present study.
SM was previously employed at the national knowledge-based management system, which included professional contact with patient representatives and healthcare professional representatives participating in the system.
YN was involved in the system 2017–2022 and represented Mid-Sweden, a larger healthcare region and had assignments at the system’s national level.
CL has been patient representative in a national working group.
HÅ has been engaged at the local level of knowledge-based management.
GH has been involved in the system and has had assignments at the national level.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Määttä, S., Petersson, C., Gäre, B.A. et al. Experiences of co-producing person-centred and cohesive clinical pathways in the national system for knowledge-based management in Swedish healthcare: a qualitative study. Res Involv Engagem 10 , 55 (2024). https://doi.org/10.1186/s40900-024-00565-3
Download citation
Received : 16 November 2023
Accepted : 18 March 2024
Published : 07 June 2024
DOI : https://doi.org/10.1186/s40900-024-00565-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Co-production
- Experiences
- Patient participation
- Healthcare system
- Clinical pathways
- Macro level
Research Involvement and Engagement
ISSN: 2056-7529
- General enquiries: [email protected]
- Open access
- Published: 25 April 2024
A qualitative evaluation of factors influencing Tumor Treating fields (TTFields) therapy decision making among brain tumor patients and physicians
- Priya Kumthekar 1 , 2 ,
- Madison Lyleroehr 3 ,
- Leilani Lacson 7 ,
- Rimas V. Lukas 1 , 2 ,
- Karan Dixit 1 , 2 ,
- Roger Stupp 1 , 2 ,
- Timothy Kruser 7 ,
- Jeff Raizer 1 , 2 ,
- Alexander Hou 6 ,
- Sean Sachdev 5 , 2 ,
- Margaret Schwartz 1 , 2 ,
- Jessica Bajas PA 1 ,
- Ray Lezon 1 , 2 ,
- Karyn Schmidt 1 ,
- Christina Amidei 4 , 2 &
- Karen Kaiser 3
BMC Cancer volume 24 , Article number: 527 ( 2024 ) Cite this article
439 Accesses
Metrics details
Tumor Treating Fields (TTFields) Therapy is an FDA-approved therapy in the first line and recurrent setting for glioblastoma. Despite Phase 3 evidence showing improved survival with TTFields, it is not uniformly utilized. We aimed to examine patient and clinician views of TTFields and factors shaping utilization of TTFields through a unique research partnership with medical neuro oncology and medical social sciences.
Adult glioblastoma patients who were offered TTFields at a tertiary care academic hospital were invited to participate in a semi-structured interview about their decision to use or not use TTFields. Clinicians who prescribe TTFields were invited to participate in a semi-structured interview about TTFields.
Interviews were completed with 40 patients with a mean age of 53 years; 92.5% were white and 60% were male. Participants who decided against TTFields stated that head shaving, appearing sick, and inconvenience of wearing/carrying the device most influenced their decision. The most influential factors for use of TTFields were the efficacy of the device and their clinician’s opinion. Clinicians ( N = 9) stated that TTFields was a good option for glioblastoma patients, but some noted that their patients should consider the burdens and benefits of TTFields as it may not be the desired choice for all patients.
Conclusions
This is the first study to examine patient decision making for TTFields. Findings suggest that clinician support and efficacy data are among the key decision-making factors. Properly understanding the path to patients’ decision making is crucial in optimizing the use of TTFields and other therapeutic decisions for glioblastoma patients.
Peer Review reports
Introduction
Glioblastoma is the most common malignant primary brain tumor in adults, accounting for over 50% of all gliomas, with an annual incidence rate of 3 to 4 cases per 100,000 people, resulting in 240,000 newly diagnosed cases worldwide each year [ 1 , 2 ]. Since 2005, the standard treatment for glioblastoma has been surgical resection followed by radiotherapy with concurrent and adjuvant temozolomide (TMZ). For newly diagnosed glioblastomas, the addition of TMZ to surgery and radiation therapy prolongs median survival from 12.1 to 14.6 months and increases the five-year survival rate from 2 to 10% [ 3 ].
In addition to the current standard of care, patients with glioblastomas can receive a more recently approved therapy called Tumor Treating Fields Therapy (TTFields) (Optune™). TTFields utilizes a portable, battery-operated device that delivers a low-intensity, alternating electric field to the tumor via surface electrodes (transducer arrays) [ 4 ]. The electric field disrupts the normal mitotic process for tumor cells and leads to cancer cell death [ 5 ]. In patients with recurrent glioblastoma brain tumors, TTFields has shown clinical efficacy comparable to that of active chemotherapies, without many of the side effects of chemotherapy [ 6 , 7 ]. TTFields was first FDA approved in the recurrent setting after it showed non-inferiority in a phase 3 trial compared to “physician’s best choice” treatment [ 8 ]. Subsequently, a first line randomized Phase 3 trial compared TTFields plus TMZ to TMZ alone among 695 glioblastoma patients who had completed radiochemotherapy. The TTFields treatment arm showed a significant improvement in both progression-free survival (median progression-free survival was 6.7 months in the TTFields plus TMZ group and 4.0 months in the TMZ alone group) and overall survival (median overall survival 20.9 months versus 16.0 months), leading to FDA approval of TTFields in the first line setting [ 9 , 10 ]. Side effects reported in the TTFields plus TMZ group were limited to mild to moderate skin toxicity under the transducer arrays [ 10 ]. Following FDA approval to use TTFields for glioblastoma and, subsequently, mesothelioma [ 11 ], the National Comprehensive Cancer Network (NCCN) added TTFields to its guidelines for evidence-based management of new or recurrent glioblastoma in 2018 [ 12 , 13 ].
Despite regulatory and national guideline support for TTFields, evidence demonstrating improved survival with TTFields, no severe side effects from the device, and limited treatments for glioblastoma, not all patients who qualify for TTFields choose to use the device. Moreover, there has been reluctance among neuro-oncologists to adopt TTFields [ 12 ]. This qualitative study aimed to grow our understanding of glioblastoma patients’ decision on whether or not to use TTFields, the role of clinicians in their decisions, and clinicians’ views of TTFields.
Materials and methods
Patient enrollment.
The study protocol was approved by the institutional review board of Northwestern University and all patients enrolled on study provided written informed consent prior to any study-related procedures. Patients with a glioblastoma receiving treatment at the Malnati Brain Tumor Institute at the Lurie Comprehensive Cancer Center of Northwestern University who had been offered treatment with TTFields and had decided whether to initiate TTFields therapy were eligible to participate in the study. Other eligibility criteria included: able to speak and understand English, age 18 or older, and cognitively able to complete a study interview. We aimed to interview up to 50 glioblastoma patients who had been offered TTFields. In 2020, 180 new glioblastoma patients were seen at the Malnati Brain Tumor Institute and 51 TTFields prescriptions were written.
Patients were enrolled consecutively between June of 2020 and February of 2021, the entirety of which occurred during Covid-19 pandemic; therefore, consenting and interviews occurred remotely. In the first month of the project, clinicians provided the names of glioblastoma patients who had been offered TTFields for study inclusion; subsequently, a study coordinator (co-author LL) identified glioblastoma patients in the electronic medical record who had been offered or who had decided to use TTFields. Clinicians then confirmed patients were physically and cognitively able to participant and the study coordinator contacted eligible patients via telephone, explained the study, and obtained informed consent electronically. The approximately 30-minute study interview was subsequently conducted via phone by the study coordinator, who had extensive experience conducting patient interviews. A semi-structured interview guide was used to gather patient input on their views of TTFields, factors that influenced their TTFields decision, and their perceptions of whether their clinician wanted them to use TTFields. Patients also completed the Control Preference Scale, which is a one-item measure of preferred role in medical decision making that has been tested and validated with cancer patients [ 14 , 15 , 16 ]. Patients received a $25 Visa gift card following participation. Interviews were audio recorded to ensure comprehensive capture of all relevant patient-reported information.
Clinician sample
Clinicians in the Malnati Brain Tumor Institute of Northwestern University who offer and prescribe TTFields therapy received an invitation via email to participate in a study interview. This included physicians (neuro-oncologists) and advanced practitioners (Advanced Practice Nurses and Physicians Assistants). All eligible physicians and advanced practitioners interviewed were specifically trained and certified to prescribe tumor treating fields by Novocure through the company-run training program. This is required to be able to prescribe this device to patients. Clinician participants provided verbal consent via telephone prior to participating in a telephone interview. As with the patient interviews, clinicians’ interviews were audio recorded. A semi-structured interview guide was used to gather their views of TTFields. Clinicians were not compensated for participating.
Data analysis
The interviewer entered detailed notes into an Excel database following each interview. The database became the basis for a preliminary analysis of each interview question. Notes for each question were reviewed by the study coordinator, an experienced qualitative analyst (co-author ML), and a qualitative researcher (co-author KK) to identify preliminary themes. Next, the three study team members reviewed the interview transcripts to finalize themes, confirm themes were comprehensive and reflected the data, and to identify supporting quotations.
Patient results
One-hundred and five glioblastoma patients were identified via physician recommendation or medical record review between June of 2020 and February of 2021. Of these, a total of 11 (10.5%) patients were deemed ineligible because they were not offered TTFields ( n = 2), had gone to another center for treatment ( n = 1), had entered hospice ( n = 6), or died prior to recruitment ( n = 2). Twenty-one patients (20.0%) were excluded per clinician recommendation. Reasons for clinician-recommended exclusion included cognitive issues, speech difficulties, and illness severity. Twenty (19.1%) patients were unresponsive to recruitment efforts, and 13 (12.4%) patients declined to participate. Individual interviews were conducted with 40 (38.1%) individuals with glioblastoma. Among the 40 participants (Table 1 ), the mean age was 53 years (range 21–77 years). Most participants were white (92.5%), married (80.0%), and male (60.0%). The study coordinator confirmed each patient’s TTFields status at the time of recruitment. Thirty-two participants (80.0%) chose to pursue TTFields therapy, while eight (20.0%) did not use TTFields. The TTFields group and the no-TTFields group were similar in age and gender. Patients who declined TTFields were less likely to use TTFields resources (Table 1 ); however, we would expect that TTFields users would be more apt to seek out information about TTFields.
Control Preference Scale results are shown in Table 2 . In both groups, patients most often preferred to make decisions for themselves after considering their doctors opinion ( n = 15, 46.9% among patients who utilized TTFields, n = 5, 62.5% among patients who declined TTFields). Six (18.8%) of the patients who chose TTFields preferred to have their doctor make their medical decisions either with consideration for the patient’s opinion ( n = 3, 9.4%) or on their own ( n = 3, 9.4%). In contrast, none of the patients who declined TTFields preferred to have their doctor make their decisions.
Participants who chose TTFields
Participants who chose TTFields noted downsides associated with the treatment. The most frequently mentioned downside of TTFields was the burden of changing the TTFields arrays, which happened frequently (every few days) and could be painful. The heat of the device on one’s head was also noted as a downside, along with the discomfort of wearing the cap and the burden on caregivers who assist them when changing their cap and arrays. Some users of TTFields experience skin reactions, such as blisters or itching. Participants also noted it could be difficult to sleep or shower with the device, and carrying the device was cumbersome.
However, many of the patients who chose TTFields came to accept the burdens of using the device. For example, some noted that shaving their head for TTFields was easy and/or worth the trouble. “The head shaving part was easy because I had lost most of my hair already.” Another participant said, “I used it (TTFields) for two years, and if they told me that I had to re-shave my head and use it longer, I would do it.” Likewise, participants who chose TTFields said that the appearance of the device could be bothersome, but they were not deterred by it. In fact, one participant had a positive experience due to the visible nature of TTFields: “Pretty much right after I was fitted for it, I think the next day, I was back at work. So, it was kind of awkward at first, but I actually had some good conversations with people about it in the days and weeks after that.”
For the patients who chose TTFields, the efficacy of TTFields was the most frequently cited reason for choosing to use the device. As shown in Table 3 , they described efficacy in several ways, including extension of life, shrinking one’s tumor, and the device being supported by clinical studies. Extension of life was cited by over a third ( n = 13, 40.6%) of those who chose TTFields (Table 3 ). One participant stated, “I don’t want to die. And I feel that if I don’t have this, that I will die.” Another participant spoke of the value of extending life even with potential negative effects: “Am I willing to be slightly inconvenienced for an additional five months of life? Yeah, I’ll go with that deal.” For others, clinical evidence supporting the efficacy of TTFields, particularly the extension of life, was pivotal in their decision to undergo TTFields. One participant stated that the biggest factor in their decision was “without question, FDA approved that this treatment does extend your life by a significant percentage.”
The second most influential factor reported by those who chose TTFields was their doctor’s opinion ( n = 9, 28.1%). As one participant stated, “We (participant and their spouse) absolutely believe in both the physicians who recommended it (TTFields). So, we really trust them a lot.” All participants who reported that their doctor’s opinion was the most influential factor in their decision to undergo TTFields also reported that their doctor recommended TTFields.
Familial considerations were cited as the most influential factor for four (12.5%) participants. Three of the four people in this group noted that they wanted to extend time with their families. Several other influences were mentioned by one person each (Table 3 ). For example, one participant said she chose TTFields after hearing about the experience of a family friend who had used TTFields and recommended it despite the inconveniences of wearing the device.
Participants who declined TTFields
For those glioblastoma patients who chose not to use TTFields, the most influential factor in their decision was the requirement to shave their head ( n = 4, 50.0%) (Table 4 ). “I know some people probably think that’s kind of silly, like, ‘You have cancer, so who cares if you have hair or not?’ But it’s just been really hard for me.” Another influential factor was the visibility of TTFields ( n = 3, 37.5%). For example, two participants did not like the idea of wearing the device at work. One of them said, “I was still working, and at that time, I did not share with them everything that was going on. So, it would have definitely exposed things, and who knows what would have happened after that.”
Other reasons for declining TTFields included the inconvenience of continuously wearing the device and carrying the battery pack. One participant expressed a personal concern about the idea of simultaneously receiving chemo and TTFields, while another reported that multiple doctors recommended against going on TTFields because of an existing surgical implant. Additional reasons for not going on TTFields included thinking it would not be needed, that it would not improve quality of life, and that the increased lifespan would not outweigh the negative impact of TTFields. As one participant explained:
Yes, there’s no negative impact, I guess, physically. However, the idea of having something attached to my head and then having to carry around the battery pack doesn’t really mesh well with my relatively physical quality of life…(TTFields) would actually have quite significant negative impacts on how I live my life.
Questions about TTFields
When asked if there was anything about TTFields that was confusing to them, most participants ( N = 33, 85.5%) said no. The aspects of TTFields reported as unclear by seven (17.5%) participants are shown in Table 5 . Participants questions centered around efficacy of the device, how the device works, and what to do if the device gets wet.
Participants views of extension of life from TTFields
We asked participants to describe their understanding of how long TTFields would extend one’s life. Of the 30 participants who answered this question (the question was added to the interview guide after 9 interviews had been completed; one participant chose to skip this question), the most common response was that they did not know how long TTFields extends life ( n = 12, 40.0%). The next most common response was that TTFields extended life several months (e.g., “2–4 months”, “3–6 months”) ( n = 8, 26.6%). Five participants (16.6%) said that they did not have a specific number in mind, but they believed that TTFields extended life. Three participants (10.0%) said TTFields extend life by years (“2 years”, “2–5 years”, “3–14 years”) and two participants (6.6%) provided an answer based on a percentage (e.g., 20–30%, 15–18%); it was unclear what those percentages meant.
Six participants who did not choose TTFields answered the question about extension of life. Of these, 4 (66.6%) said they did not know the extension of life provided by TTFields.
Impact of physician recommendations for TTFields
Among participants who chose TTFields, the majority reported that their clinician recommended TTFields ( n = 25, 78.1%) (Fig. 1 ). The remaining seven (58.3%) participants who chose TTFields said their clinician was neutral towards TTFields. Participants described their physicians’ neutrality as not “pushing” or wanting to “force” a decision on them. According to one participant, “[My doctor] didn’t want to push it, he did say, ‘It’s just another tool in the toolbox,’ and I’m one of these guys who wants to use all the tools.”
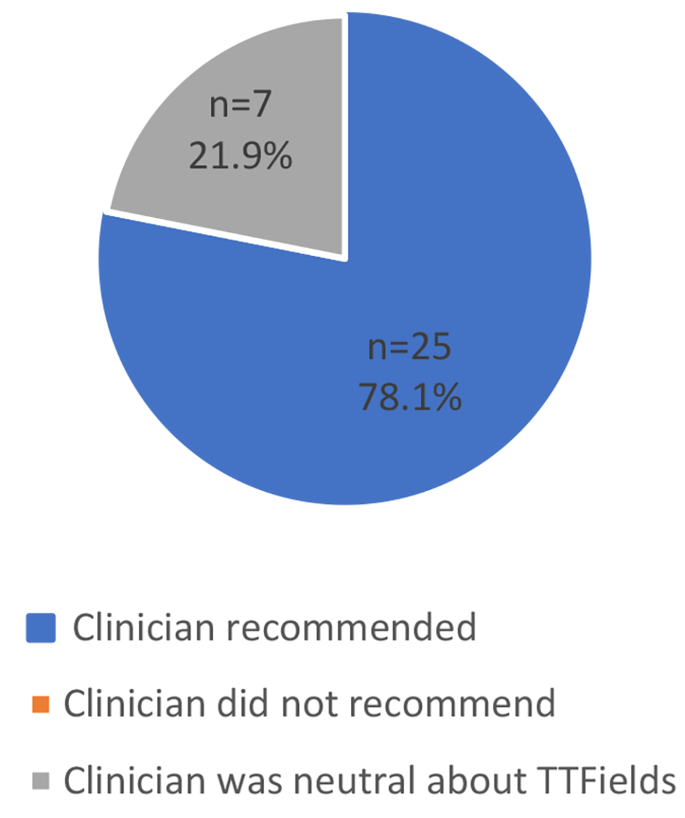
Clinician’s Recommendations for TTFields: Patients who Chose TTFields ( N = 32)
For those who did not choose TTFields, 5 (62.5%) reported that their clinician was neutral regarding the patient’s decision, 2 (25.0%) reported that their clinician advised against TTFields, and 1 (12.5%) reported that their clinician recommended TTFields (Fig. 2 ). While the 2 participants whose clinician advised against TTFields did not report their doctor’s opinion as the most influential factor in their decision, one of them stated, “I will use the Optune (TTFields) device if the doctor recommends it.”
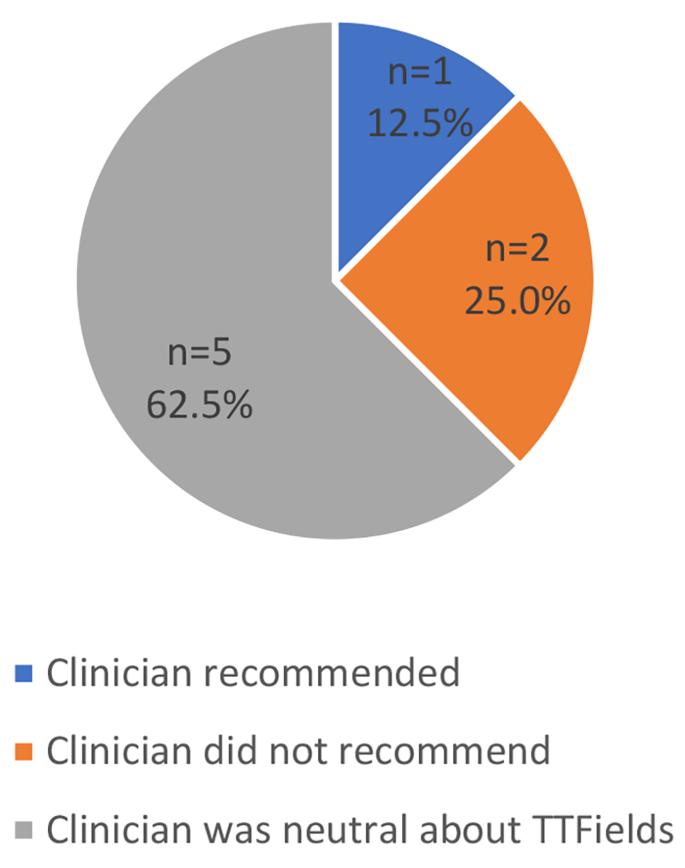
Clinician’s Recommendations for TTFields: Patients who did not Choose TTFields ( N = 8)
One participant who did not utilize TTFields described how their clinician presented the information about TTFields:
He had also said it’s the type of thing where you have to really commit to it long-term. And, he also said he likes for his patients to really feel committed to it if they want to do it, just because it’s going to be more effective if you really buy into it. And if I didn’t feel like I was there, then that was okay.
Only one participant went against their doctor’s recommendation by deciding not to undergo TTFields. This participant did not want to wear the TTFields device while working, shave their head, or wear the backpack to carry the device. The most influential factor for this participant, however, was their belief that their cancer would not come back after initial treatment. At the time of the interview, this participant was re-considering TTFields and awaiting the doctor’s recommendation based on pending test results.
Clinician results
Clinician participants ( N = 9) were predominantly male ( n = 6, 66.7%) and included five neuro-oncologists, three advanced practitioners, and a physician assistant. The clinicians had been treating glioblastoma patients for an average of 14 years (range 1–30 years) and saw an average of 38 glioblastoma patients per month (range 17–60 patients). In a typical month, they treated an average of 11 glioblastoma patients with TTFields (range 1–25 patients).
Views of TTFields: benefits and caveats
When asked if they considered TTFields to be a good treatment option for glioblastoma patients, every clinician ( N = 9, 100%) said yes, although their enthusiasm for TTFields varied. Clinicians noted that it was a good option because it has been shown to have an impact, there are few treatment options available, and it is less toxic than other treatment options. Below are example comments from clinicians regarding the benefits of TTFields:
No question (it is a good treatment option). All of the treatment options have somewhat modest efficacy but it’s better than nothing. I will tell them when I start a treatment, when all we had was radiation, I had 90% of my patients dead within less than two years. Now, I have close to 50% of patients doing well at two years. I think that’s pretty straightforward from my perspective. It’s a good treatment because it’s a treatment that’s been shown to improve progression-free survival and improve landmark survival…So, you put those points together and it seems as if it has a real impact. I try not to say in so many words that we don’t have a lot of options for them with this disease and that this is one that we know works for whatever true benefit it provides for each patient, we know that it provides a benefit, and that of the options we have, this is the least-toxic, the one that will be the least likely to cause them any ill effects, will mold into their lifestyles the easiest, and that it does work.
However, some clinicians noted caveats to their endorsement of TTFields. For example, some noted that TTFields is not feasible for certain patients, such as the elderly or patients with poor performance status. This clinician noted the best candidates are patients who have a caregiver to help them with the device or are very functional and motivated to manage the device themselves. Likewise, another clinician emphasized the need for patient motivation to use TTFields:
This (TTFields) is kind of part of you all the time, so I think people just have to kind of accept that. I think the website does a good job of showing people living their normal life with the device, so if people feel like they can be like that, then I think it’s a great treatment, but they have to be willing… and buy into shaving their head, changing the arrays, having the device on 18-plus hours a day, taking it with them when they leave the house, being connected to the plug when they’re at home.
Several clinicians described a neutral approach to advising patients about TTFields. These clinicians said that evaluating whether the burden of TTFields is worth the benefit is the patient’s decision.
I typically frame it in a way where if the patient feels that the burden outweighs the benefit, then they’re the ones in the driver’s seat and they can say, I don’t want to do it because of their perception that this has too much of a negative impact on their quality of life.
One oncologist noted that patients’ views of TTFields are influenced by how clinicians present TTFields:
I think none of us have hesitation presenting to somebody whom we meet who we suspect has a brain tumor that, “You need surgery. There’s no way around this.” Right? And so, we tell them that and we’re comfortable. We have no problem telling them, “You need radiation therapy, or we need to give you this chemotherapy.” But I think culturally, within the neuro-oncology community, there is some hesitancy to say, “Oh, you also need TTFields.” It’s strange to me that that’s the case, because all these other things that are much bigger-gun therapeutics with higher risk profiles, we have no problem recommending.
When asked why clinicians are hesitant to endorse TTFields, this oncologist noted two reasons. First, he noted that changing behavior that is ingrained in one’s work culture is difficult. Second, TTFields is foreign to the oncology world:
Clinician: I think the other aspect that makes tumor treating fields a little bit strange and odd is…it’s coming from the electrical engineering world. And almost none of us have a background in that…. Interviewer: Okay. Do you think physicians are hesitant to use TTFields because they doubt the evidence behind it, or just because it is different? Clinician: I think some people doubt the evidence and I think it’s easier to doubt the evidence when something is different. When you have an outlier idea, the body of proof that you need to and should have to present becomes much higher. So, if you’re presenting a concept that’s not that far removed from everything else that is rapidly accepted as dogma, the burden of proof doesn’t have to be huge… I think there are critics that come at it from the neuro-oncology community that it’s a treatment that didn’t have a sham control, which one could argue we had no problem accepting the lack of blinded study design for temozolomide, which everyone is comfortable administering. So, we have a precedent, but I think people sometimes forget that.
When were asked if they would recommend TTFields for a family member or use it themselves if they had glioblastoma, four of the nine (44%) clinicians said yes, citing reasons such as the minimal risks and the desire to do everything possible to extend their life. Three clinicians (33%) said maybe, noting that it would depend upon whether they would want to go to hospice or obtain treatment, upon the condition of themself or their loved one, and that they probably would not want to be attached to the device but if in that situation they may feel differently. Two clinicians (22%) said no, they would not use TTFields themselves or recommend it for a family member. Of the two who said no, one explained that they would not want to extend life in a compromised state; three months of survival without TTFields vs. 15 months of survival on TTFields was not worth the burden of the device. Similarly, the other physician noted that the added survival does not outweigh the negative quality of life impacts of TTFields.
Discussing survival benefits of TTFields
All clinicians noted that TTFields has a proven benefit for patient lifespan. When asked how they describe the lifespan benefits to patients, clinicians described TTFields benefits in general terms, as evidenced in the quotes below:
(I tell patients) it has sort of become a standard of care for patients after radiation. There’s data that says it improves overall survival and most times it is tolerated pretty well. I don’t (talk to them about benefits to their lifespan), except to say generally that it can add—that really the advantage is that it can buy them some time that is of quality. The problem is that if you talk about time, the time itself isn’t super-significant, in my opinion. And everyone is different. I don’t know what someone’s progression might be with or without Optune (TTFields)… I do tell them that it will add time to their lives, theoretically…but I can’t talk about specific times.
One clinician noted that he tells patients that TTFields can increase two-year survival. However, he felt that discussing months of life extension was not appropriate:
I usually don’t quote months because I think at that moment (the initial meeting) they’re probably too fragile…I rarely quote months at the initial meeting. So, I keep things broader. I don’t say, ‘Well data supports that using this, it improves survival by four months or something.’ I don’t say that.
Another clinician also felt that it would be detrimental to patients to tell them the number of months of extended life provided by TTFields:
It’s tough to do without deflating the patient. And the goal is to infuse the patient with a reasonable hope and not overinflate their expectations. So, keep it reasonable, but at the same time give them things that I feel hopeful about.
Clinicians noted that they typically provided specific data on life extension only if asked. As one clinician noted, “If the patient asks for specific data around the treatment, I’m happy to give that to them. But I tend to avoid talking about statistics.” According to another clinician, “I would say it’s the rare patient who wants a lot more detail than– they usually don’t want to get super-scientific about it.”
This is the first study of views of TTFields among glioblastoma patients and clinicians. Our findings indicate that TTFields is burdensome for patients who use the device, particularly due to changing the arrays and carrying the device. Because there is no cure for glioblastomas, treatment decisions involve prioritizing length of life (LOL) or quality of life (QOL). However, our participants who chose TTFields reported a willingness to accept the burden of TTFields because of its proven efficacy. These results are consistent with the phase three clinical trials of TTFields in which patients receiving TTFields did not report worse social role, social functioning, or physical functioning despite the physical burden of carrying the device and the social impact of the visibility of the device [ 17 ]. Thus, for patients motivated to use this device, the quality of life burden may not be excessive [ 18 ].
Patients who declined TTFields stated that its QOL impacts, such as shaving one’s head or the visibility of TTFields, outweighed the potential LOL benefits. Interestingly, many participants who declined TTFields reported not knowing its impact on survival. It may be that for these patients, no extension of life would outweigh the burden of TTFields. These findings are consistent with observations made by other glioblastoma research: “It appears that, for some, the inconvenience and/or possible stigma associated with the device may be easily mitigated by the potential survival benefit; however, for others, a survival benefit without the promise of a cure may not justify the need for continuous use of the device.” [ 12 ] (p.859).
When presenting TTFields to their glioblastoma patients, clinicians in this sample typically described TTFields’s lifespan advantages in general terms rather than by providing specific prognostic information. Some clinicians noted a desire to balance the fragility of patients diagnosed with a terminal illness with the need to provide information. These findings are consistent with prior work on decision making in advanced cancer wherein clinicians are hesitant to discuss survival and treatment outcomes, [ 19 , 20 , 21 ] physicians make implicit judgements about patients’ desired level of information, [ 22 ] and the central characteristics of shared decision making are often absent [ 23 ]. Although advanced cancer patients, including glioblastoma patients, often report satisfaction with treatment decision making [ 23 ], most patients with incurable cancer want information on life expectancy, including typical, best, and worst case scenarios [ 24 , 25 , 26 , 27 ]. Moreover, awareness of cancer prognosis is linked to improved patient quality of life, goal-concordant care, and lower healthcare costs [ 20 , 28 , 29 ]. Thus, glioblastoma patients may benefit from tools designed to assist them in asking questions about their prognosis [ 30 ].
Patients’ preferred decision-making roles may impact the decision to use TTFields. Patients who declined TTFields were more likely to report a preference for independent decision-making. This preliminary finding should be confirmed in future work with a larger sample of patients. Additionally, these data suggest clinicians could utilize patient decision making preferences to frame the discussion when presenting the TTFields option.
Patients’ TTFields decisions tended to align with their perception of what the physician recommended for them. Clinicians in our sample were generally supportive of using TTFields for glioblastoma patients. The level of support for TTFields among clinicians in this sample is unusual; [ 12 ] future work should consider clinician support of TTFields in other institutions and with larger samples. Our clinician sample noted that TTFields was an appropriate treatment option for glioblastoma because it was shown to be efficacious, there are few treatment options available for glioblastoma, and it is less toxic than other treatment options. While some clinicians enthusiastically endorsed TTFields for their eligible patients, others presented it as an option but noted that they want patients to consider whether the burden of TTFields is worth the benefits of the treatment and emphasized that patients needed to be motivated to commit to using the device.
Our sample consisted primarily of patients who chose to use TTFields. The large number of TTFields users in our sample is due, in part, to the fact that patients interested in trying all forms of treatment often seek out clinicians at the Malnati Brain Tumor Institute. Additionally, patients who declined TTFields may have been in poorer health and deemed ineligible for this study. Additional work is needed to confirm preliminary findings among a sample of patients who decline TTFields. Finally, future work can build upon our findings to develop decision tools for patients and clinicians considering TTFields. These tools should incorporate patients’ desired decision-making role and assess patients’ openness to receiving specific information about survival benefits.
Qualitative research within healthcare aims to uncover meaning, listen to the perspectives of key stakeholders, and build theories [ 31 ]. Without qualitative exploration, subsequent quantitative work may overlook or misrepresent key factors for a particular health problem. We sought to identify factors in the social environment or in patient beliefs that shape TTFields decisions for adult glioblastoma patients.
The decision to use TTFields is a highly personal one for glioblastoma patients. Our findings, which come from the first study of views of TTFields among glioblastoma patients and clinicians, indicate that for some patients who refuse the device, the extension of life gained from using TTFields cannot outweigh the burden of the device. However, the quality-of-life burden of the device may not be excessive for patients who are motivated to use it. Increasing provider support of TTFields may lead to increased use of the device as patients’ TTFields decisions tended to align with their perception of what the physician recommended. Future work should consider the extent to which glioblastoma patients desire more specific prognostic information.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Tumor Treating Fields
Temozolomide
National Comprehensive Cancer Network
Length of life
Quality of life
Central Brain Tumor Registry of the United States. CBTRUS Statistical Report:Primary Brain and Central Nervous System Tumors Diagnosed in the United States in 2004–2008. 2012.
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127(12):2893–917.
Article CAS PubMed Google Scholar
Stupp R, Roila F, Group EGW. Malignant glioma: ESMO clinical recommendations for diagnosis, treatment and follow-up. Ann Oncol. 2009;20(Suppl 4):126–8.
Article PubMed Google Scholar
Novocure O. Elevate Expectations. Available from: https://www.optune.com/ .
Swanson KD, Lok E, Wong ET. An overview of Alternating Electric fields Therapy (NovoTTF Therapy) for the treatment of malignant glioma. Curr Neurol Neurosci Rep. 2016;16(1):8.
Article PubMed PubMed Central Google Scholar
Jain KK. A critical overview of targeted therapies for Glioblastoma. Front Oncol. 2018;8:419.
Oldfield EH, Ram Z, Culver KW, Blaese RM, DeVroom HL, Anderson WF. Gene therapy for the treatment of brain tumors using intra-tumoral transduction with the thymidine kinase gene and intravenous ganciclovir. Hum Gene Ther. 1993;4(1):39–69.
Kanner AA, Wong ET, Villano JL, Ram Z, Investigators EF. Post Hoc analyses of intention-to-treat population in phase III comparison of NovoTTF-100A system versus best physician’s choice chemotherapy. Semin Oncol. 2014;41(Suppl 6):25–34.
Article Google Scholar
Stupp R, Taillibert S, Kanner AA, Kesari S, Steinberg DM, Toms SA, et al. Maintenance Therapy with Tumor-Treating Fields Plus Temozolomide vs Temozolomide alone for Glioblastoma: a Randomized Clinical Trial. JAMA. 2015;314(23):2535–43.
Stupp R, Taillibert S, Kanner A, Read W, Steinberg D, Lhermitte B, et al. Effect of Tumor-Treating Fields Plus maintenance temozolomide vs maintenance temozolomide alone on survival in patients with glioblastoma: a Randomized Clinical Trial. JAMA. 2017;318(23):2306–16.
Article CAS PubMed PubMed Central Google Scholar
U.S, Food. & Drug Administration. NovoTTF™-100L System - H180002 2019. Available from: https://www.fda.gov/medical-devices/recently-approved-devices/novottftm-100l-system-h180002 .
Thomas AA, Rauschkolb PK. Tumor treating fields for glioblastoma: should it or will it ever be adopted? Curr Opin Neurol. 2019;32(6):857–63.
National Comprehensive Cancer Network. NCCN Guidelines: Central Nervous System Cancers 2021. Available from: https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1425 .
Degner LF, J. KL DB, et al. Information needs and decisional preferences in women with breast cancer. JAMA. 1997;277(18):1485–92.
Degner LF, Sloan JA. Decision making during serious illness: what role do patients really want to play? J Clin Epidemiol. 1992;45(9):941–50.
Tariman JD, Berry DL, Cochrane B, Doorenbos A, Schepp K. Preferred and actual participation roles during health care decision making in persons with cancer: a systematic review. Ann Oncol. 2010;21(6):1145–51.
Taphoorn MJB, Dirven L, Kanner AA, Lavy-Shahaf G, Weinberg U, Taillibert S, et al. Influence of Treatment with Tumor-Treating fields on Health-related quality of life of patients with newly diagnosed glioblastoma: a secondary analysis of a Randomized Clinical Trial. JAMA Oncol. 2018;4(4):495–504.
Halasz LM, Mitin T. Tumor-treating fields: answering the concern about quality of life. JAMA Oncol. 2018;4(4):504–5.
Audrey S, Abel J, Blazeby JM, Falk S, Campbell R. What oncologists tell patients about survival benefits of palliative chemotherapy and implications for informed consent: qualitative study. BMJ. 2008;337:a752.
Bloom JR, Marshall DC, Rodriguez-Russo C, Martin E, Jones JA, Dharmarajan KV. Prognostic disclosure in oncology - current communication models: a scoping review. BMJ Supportive Palliat Care. 2022;12(2):167.
Liu PH, Landrum MB, Weeks JC, Huskamp HA, Kahn KL, He Y, et al. Physicians’ propensity to discuss prognosis is associated with patients’ awareness of prognosis for metastatic cancers. J Palliat Med. 2014;17(6):673–82.
De Snoo-Trimp JC, Brom L, Pasman HR, Onwuteaka-Philipsen BD, Widdershoven GA. Perspectives of medical specialists on sharing decisions in Cancer Care: a qualitative study concerning chemotherapy decisions with patients with recurrent glioblastoma. Oncologist. 2015;20(10):1182–8.
Brom L, De Snoo-Trimp JC, Onwuteaka-Philipsen BD, Widdershoven GA, Stiggelbout AM, Pasman HR. Challenges in shared decision making in advanced cancer care: a qualitative longitudinal observational and interview study. Health Expect. 2017;20(1):69–84.
Kiely BE, Stockler MR, Tattersall MH. Thinking and talking about life expectancy in incurable cancer. Semin Oncol. 2011;38(3):380–5.
Hagerty RG, Butow PN, Ellis PA, Lobb EA, Pendlebury S, Leighl N, et al. Cancer patient preferences for communication of prognosis in the metastatic setting. J Clin Oncol. 2004;22(9):1721–30.
Greisinger AJ, Lorimor RJ, Aday LA, Winn RJ, Baile WF. Terminally ill cancer patients. Their most important concerns. Cancer Pract. 1997;5(3):147–54.
CAS PubMed Google Scholar
Parker SM, Clayton JM, Hancock K, Walder S, Butow PN, Carrick S, et al. A systematic review of prognostic/end-of-life communication with adults in the advanced stages of a life-limiting illness: patient/caregiver preferences for the content, style, and timing of information. J Pain Symptom Manage. 2007;34(1):81–93.
Epstein AS, Prigerson HG, O’Reilly EM, Maciejewski PK. Discussions of life expectancy and changes in illness understanding in patients with Advanced Cancer. J Clin Oncol. 2016;34(20):2398–403.
Mack JW, Cronin A, Keating NL, Taback N, Huskamp HA, Malin JL, et al. Associations between End-of-life discussion characteristics and Care received Near Death: a prospective cohort study. J Clin Oncol. 2012;30(35):4387–95.
Clayton JM, Butow PN, Tattersall MHN, Devine RJ, Simpson JM, Aggarwal G, et al. Randomized Controlled Trial of a prompt list to help Advanced Cancer patients and their caregivers to ask questions about prognosis and end-of-Life Care. J Clin Oncol. 2007;25(6):715–23.
Renjith V, Yesodharan R, Noronha JA, Ladd E, George A. Qualitative methods in Health Care Research. Int J Prev Med. 2021;12:20.
PubMed PubMed Central Google Scholar
Download references
Acknowledgements
We are grateful to the patients and physicians from the Lou and Jean Malnati Brain Tumor Institute Cancer Institute of Northwestern University who generously gave their time to participate in this study.
Funding was obtained via an investigator-initiated grant funded by Novocure.
Author information
Authors and affiliations.
Department of Neurology, Northwestern University Feinberg School of Medicine, Abbott Hall Suite 1122 710 N Lake Shore Drive, Chicago, IL, 60611, USA
Priya Kumthekar, Rimas V. Lukas, Karan Dixit, Roger Stupp, Jeff Raizer, Margaret Schwartz, Jessica Bajas PA, Ray Lezon & Karyn Schmidt
Lou and Jean Malnati Brain Tumor Institute, Robert H. Lurie Comprehensive Cancer Center of Northwestern University, Chicago, United States
Priya Kumthekar, Rimas V. Lukas, Karan Dixit, Roger Stupp, Jeff Raizer, Sean Sachdev, Margaret Schwartz, Ray Lezon & Christina Amidei
Department of Neurological Surgery, Northwestern University Feinberg School of Medicine, 676 N. St. Clair Street, Suite 2210, Chicago, IL, 60611, USA
Madison Lyleroehr & Karen Kaiser
Department of Radiation Oncology, Northwestern University Feinberg School of Medicine, 676 N. St. Clair Street, Suite 1820, Chicago, IL, 60611, USA
Christina Amidei
Northwestern University Feinberg School of Medicine, 420 E. Superior St, Chicago, IL, 60611, USA
Sean Sachdev
Department of Human Oncology, University of Wisconsin Carbone Cancer Center, 600 Highland Ave, Madison, WI, 53705, USA
Alexander Hou
Equal Hope, 300 South Ashland Avenue, Chicago, IL, 60607, USA
Leilani Lacson & Timothy Kruser
You can also search for this author in PubMed Google Scholar
Contributions
PK was instrumental to the project and was involved in all aspects: designing the project, drafting the manuscript, acquisition/patient accrual and analysis and interpretation of data. ML analyzed and interpreted patient interview data and wrote parts of the manuscript. LL conducted execution of the study and analysis of the data. RVL, KD, RS, JR, SS, MS, JB, RL, KS all supported the acquisition of data through patient accrual. TK, AH, and CA contributed to the study design while CA was also involved in data acquisition. KK was involved in the study design, acquisition, analysis and interpretation of data, and drafting the manuscript.
Corresponding author
Correspondence to Karen Kaiser .
Ethics declarations
Ethics approval and consent to participate.
The study protocol was approved by the institutional review board of Northwestern University (STU00210799) and all patients enrolled on study provided written informed consent prior to any study-related procedures.
Consent for publication
Not applicable.
Competing interests
PK has received research and grant support from Genentech, Novocure, DNAtrix and Orbus Therapeutics. PK has served on medical advisory boards for Biocept, Sintetica, Novocure, Janssen, Affinia, Celularity, and SDP Oncology. PK has provided consulting to Bliss Bio, Biocept, Enclear Therapies, Angiochem, Affinia Therapeutics. TK serves on an advisory board and speakers bureau for AstraZeneca, and a consultant for Radialogica LLC, none of which relate to this work. MS is in the Novocure speakers bureau. RVL serves on the speakers’ bureaus for Novocure and Merck. RVL has received research support (drug only) from BMS. RVL has received honoraria for medical editing for EBSCO Publishing, and Medlink Neurology. RVL also serves on advisory boards for Novocure, AstraZeneca, Cardinal Health, Servier, and Merck. SS has served on advisory boards for Lantheus, Astellas, and Pfizer. KK has served as a consultant for PTC Therapeutics. All other authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kumthekar, P., Lyleroehr, M., Lacson, L. et al. A qualitative evaluation of factors influencing Tumor Treating fields (TTFields) therapy decision making among brain tumor patients and physicians. BMC Cancer 24 , 527 (2024). https://doi.org/10.1186/s12885-024-12042-x
Download citation
Received : 29 September 2023
Accepted : 22 February 2024
Published : 25 April 2024
DOI : https://doi.org/10.1186/s12885-024-12042-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Glioblastoma
- Tumor treating fields
- Decision-making
ISSN: 1471-2407
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Learn / Blog / Article
Back to blog
Psychographics and personas: how to get to the truth about why people buy
What do you know about your customers? Do you know what actually makes them buy or why they choose you?
Conventional wisdom says you can perform audience segmentation by studying demographics such as age, ethnicity, and education of your target audience.
Some marketers go beyond demographics by taking psychographic data into consideration, such as attitudes, values, and desires.
But if you want to create marketing campaigns that truly engage your target audience, you need to understand a third type of data: buyer behavior psychographics.

Last updated
Reading time.

My name is Adele Revella, and I’m the CEO of the Buyer Persona Institute and author of Buyer Personas (a Fortune Magazine top 5 business book). In this article, I’m going to show you how to combine demographics and psychographics with a special focus on understanding why people buy, how they buy, and how to use these insights to make an impact with your marketing.
Psychographic data is the studying of consumers based on psychological characteristics like values, social status, desires, and goals.
Demographic data differs and typically studies consumers based on characteristics like age, gender, and education.
Five psychographic characteristics to know for your audience are their personalities, lifestyles, interests, opinions, and values.
Five buyer behavior characteristics to know for your audience are their priority initiatives, success factors, perceived barriers, decision criteria, and buyer’s journey.
Four ways to collect psychographic data include non-scripted customer interviews, surveys, focus groups, and brainstorm sessions with internal stakeholders.
Use psychographic research by:
Reviewing the data with internal subject matter experts
Identifying your top selling points
Training your sales team
Focusing on what really matters
Review these examples of psychographics to see how other companies use psychographics in marketing.
What is psychographic data?
Psychographics is the qualitative methodology of studying consumers based on psychological characteristics and traits such as values, social status, desires, goals, interests, and lifestyle choices.
Psychographics in marketing focus on understanding the consumer’s emotions and values, so you can market more accurately and better understand consumer behavior.
Psychographic data vs demographic data
Demographic data focuses on insight like age, gender, education, income, and geographic location.
Demographics tend to be quantitative whereas psychographics tend to be qualitative.
Ideally, you should use psychographics, demographics, and buyer behavior data (which we’ll go over next) to build buyer personas that will guide your marketing strategy.

10 psychographic characteristics
Two types of psychographics to consider are:
Psychographics characteristics : data that tells you about people’s attitudes and beliefs.
Buyer behavior psychographics : data that describes how someone turns into a buyer of your product/services based on the Buyer Persona Institute’s 5 Rings of Buying Insight .
You need both for a strong buyer persona.
For example: a standard buyer persona might introduce you to 'Madison, a 35-year-old project manager who loves cats and yoga.'
This buyer persona contains demographic and psychographic characteristics.
But what does this actually mean for your business? Does her love of cats or approach to exercise help you influence her choice to try out your project management software?
You’ll know the answers to questions like these when you pair the two types of psychographic characteristics together: traditional psychographics and buyer behavior psychographics.
5 psychographic characteristics

1. Personalities
Personality describes the collection of traits that someone consistently exhibits over time, as commonly assessed through a five-factor model .
The five-factor model personality traits are:
Openness : this trait reflects whether someone is open to new experiences or if they’re resistant to change
Conscientiousness : this trait indicates whether someone prefers structure, organization, and dependability, or is more spontaneous and less disciplined
Extroversion : this trait describes whether someone is outgoing, energetic, and sociable, or more reserved, reflective, and solitary
Agreeableness : this trait shows whether someone prioritizes harmony, cooperation, and empathy, or is more competitive, critical, and less concerned with others' feelings
Neuroticism : this trait measures whether someone is generally anxious, prone to negative emotions, and easily stressed, or calm, emotionally stable, and resilient
Example : a company that sells fishing gear online discovers their average customers are men who score low in extraversion (meaning they’re mostly introverted). So, they might want to include images of men enjoying solitude and fishing alone on their landing pages and social media accounts.
2. Lifestyles
Lifestyle is the collection of someone’s day-to-day activities and includes things like their associations, where they live, and where they spend their time.
Example : a company that owns a meditation app finds that many of their users are single individuals who like to spend their weekends partying. With this information, the marketing team might create advertising campaigns that speak to the need to disconnect from the hectic pace of urban life.
3. Interests
Interests include hobbies, pastimes, media consumption habits, and what occupies someone’s time.
Example : an online poker website discovers that a substantial proportion of its users also enjoy watching football/soccer. This might prompt the company to use sporting analogies in their ad campaigns (e.g., referring to a big tournament as the ‘World Cup’ of online poker).
4. Opinions, attitudes, and beliefs
Opinions, attitudes, and beliefs are distinct psychographic categories, but I’ve grouped them together because they tend to be strongly correlated. It’s not a black-and-white science, but in general religious beliefs (or lack thereof) can often predict political opinions and general worldview, and vice versa.
Example : a women’s clothing retailer discovers that much of their target market consists of deeply religious women from the southern U.S. They might consider displaying modest dresses in their Facebook ads.
Someone’s values describe their sense of right and wrong.
Example : a food delivery service finds that their customers care deeply about the environment and sustainability. They might benefit from delivering meals in biodegradable containers.
5 buyer behavior psychographic characteristics
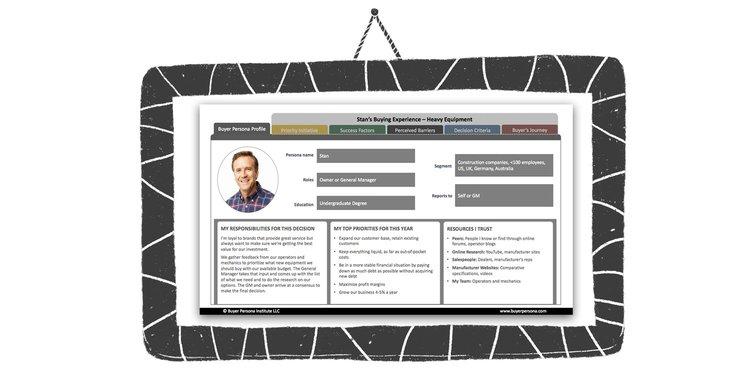
1. Priority initiatives
Priority initiatives explain why some buyers are willing to invest in a solution like yours and what separates them from those who are fine with the status quo.
Priority initiatives aren’t just pain points that your features are designed to reverse. You want to understand the precise circumstances that lead people to pursue a solution like yours.
Example : what makes a project manager seek out new software to organize their team? How do their current solutions fall short and what would inspire them to implement a new system, even though it might result in unhappy employees and critical managers who resist change?
2. Success factors
Success factors are similar to benefits, but they are more specific and defined. What results do they expect to achieve by purchasing your solution?
Example : if a young urbanite wants to buy a new computer, you might assume that speed and computing power matters. But what if speed and computer power aren’t important to them? What if the prestige that comes with owning a MacBook Pro, and the feeling its sleek design gives them, matters more than tech specs in the end?
3. Perceived barriers
What could make a potential customer worry that they’re making the wrong choice? When interviewing people who recently evaluated a solution like yours, expect to discover plenty of misconceptions—including issues you’ve already solved and some that never existed in the first place. The resistance may come from buyers themselves, but it could also come from peers, friends, family, or colleagues.
Example : does a mobile phone carrier have a reputation for dropped calls in a major city, despite the fact that they have a better-than-average record? If a sales manager wants to purchase a cell phone service for their entire sales team, their supervisors or employees might plant seeds of doubt based on a popular misconception.
4. Decision criteria
Which features of competing companies, products, or services do your customers consider essential to make a purchase? What are their expectations for each feature? What makes them leave a website , and what makes them stay?
This insight will shape your marketing strategy, and it usually has nothing to do with what’s new or what makes your product truly unique.
Example : when looking for scheduling software to book appointments, does a busy sales professional care how much it costs if the company is willing to pay for it? They may be more concerned with a particular aspect of ease of use (for both themselves and anyone who books a meeting with them).
5. Buyer’s journey
This is where you aggregate everything you learn about the steps your buyers take, the resources they trust, and the influencers involved, from beginning to the end.
Example : when someone considers buying a luxury watch, they might shop online, visit a few stores, and be influenced by articles they’ve read or their peers’ recommendations. With that in mind, it makes sense to study:
What did they do first when they decided to shop for a new watch?
How did they hear about the different brands they’re considering?
Who/what resources influenced their decision?
How to collect data for psychographic segmentation
The easiest way to collect data for market segmentation is to hear directly from your target audience.
Even better, you don’t need a huge budget to collect reliable and useful insight.
Method 1: non-scripted customer interviews
Non-scripted customer interviews open up two-way communication where you can speak with your audience one-on-one.
The questions you ask depend on what information you want from your interview. But a good question to include is this:
“What happened on the day you first decided you needed to solve this kind of problem or achieve this goal? Not to buy my product, that’s not the day. We want to go back to the day when you thought it was urgent and compelling to spend money to solve a particular problem or achieve a goal. Just tell me what happened.”

After the interviewee answers the question, ask them to clarify, elaborate, and dive deeper. Get them to walk you through every step of their buying journey.
(You might spend five or ten minutes learning about their motivations for their decision to buy.)
After, ask them to talk about what they did first to learn about the companies they were considering to buy from.
Finally, ask them to discuss how they narrowed their options, who was involved, and what they learned about the solutions they evaluated.
Your customers’ answers will clue you into the subtle motivations that made them choose you over the competition and the barriers that prevented them from buying from your competitors.
💡 Pro tip: Hotjar Engage lets you easily schedule and conduct customer interviews. Plus, you can use our pool of 200,000+ participants to find interviewees outside of our customer base to gather more diverse insight.
Engage automatically transcribes your interviews in over 20 languages, so you can share interview insight with other team members and build your buyer personas faster.
Host your first customer interview with Hotjar Engage
Use Hotjar Engage to hear directly from customers and collect valuable psychographic data.
Method 2: surveys

Surveys are a great way to hear directly from your target audience, gain confidence in the results of your interviews, and get a deeper insight into what is most or least important to buyers.
With Hotjar’s Surveys , you can add surveys to your website or send survey links to potential participants. Our free user persona survey template asks questions that will tell you:
Who your users are and how they describe themselves
What their main goal is
The barriers users face
How they use your product today

And Hotjar’s AI for Surveys instantly creates surveys that ask useful questions, so you get the insight you need, faster.
Just use caution as you create a customer survey, because you could end up merely reinforcing your existing perceptions and biases. It’s best to do the interviews first to discover the psychographics of the buying decision, and then use the survey to test your insights and learn how different markets or audiences think about the decision itself.
Method 3: focus groups
A focus group brings together a carefully selected, demographically diverse set of potential clients for a guided discussion about a product or service.
Focus groups are great when you want to expose your product or campaign to a target group of customers and see/hear their reactions. The group dynamic is ideal for this purpose, but isn't ideal for capturing individual stories and experiences (also, you need a strong facilitator to avoid the discussion being led astray by strong personalities within the group).
Focus groups can also be expensive and run anywhere from $4,000 to $12,000 . Their hefty expense may make them unattainable for those who want to collect psychographic data on a budget.
Method 4: brainstorm with internal stakeholders

Many people within your company will have information about your target customers (like your sales team or customer support team).
Speak with these people and ask them questions to uncover psychographic characteristics about your audience.
However, keep in mind that internal stakeholders’ opinions are shaped by their own biases and interactions.
For example, buyers often withhold critical information from salespeople and relate price as a critical aspect of their decision as a negotiation tactic. So, your sales team may think that price holds more weight in the buyer’s process than it actually does.
You can try to counteract these biases by speaking with a range of teams to gather diverse opinions on your buyers.
How to use psychographic research
Once you’ve gathered enough data, it’s time to put that information to good use.
Here’s how:
1. Review data with internal Subject Matter Experts (SMEs)
Organize workshops and go through all your customer data with internal SMEs who understand your product (especially product managers and salespeople).
Use these workshops to match your data with customer quotes.
For example, say your data highlights that people often use their mobile devices to access your product’s dashboard.
Find user quotes (from your surveys, interviews, etc) that support this insight.
2. Identify your top selling points
You’ll come up with many insights, but you can’t address them all, so focus on that sweet spot where your product meets what your customers want.
Review your data and customer quotes (from the previous step) to find your top selling points. These might be the points that had the most customer quotes (indicating that people brought it up the most). Or the points that had passionate language (i.e., rather than someone saying they “like” a certain feature, they might say they “can’t live without it.”).
This means you may have to stop pushing some of your favorite features and benefits. Do you love the fact that your product comes in different colors? If your ideal customers don’t love it, you’ve got to drop that selling point and focus on the messaging that works.
3. Train your sales team
As a career business-to-business (B2B) marketer, one thing I’ve noticed is that companies struggle to align their sales and marketing messages.
If you look at what sales is trained to do, the messaging in the product demos hardly ever matches up with the marketing message. After you’ve done the market research , however, you’ll know what your customers want (and you’ll have direct quotes to back your conclusions up). Then you’ve got to get marketing and sales on the same page.
4. Focus on what really matters
You’ll be tempted to do a million different things based on what you learn, but time and budget are always limiting factors. Here’s what you should focus on:
Optimize your website : perfect the buying experience to deliver exactly what your ideal customers want.
Update your product roadmap to address buying needs : product usage criteria and product buying criteria are two different things. Product managers focus on making products that customers love once they start using them, but they also need to consider what features will make someone buy the product in the first place. After all, if customers don’t buy a product, they’ll never get a chance to experience it.
Refine your messaging : make sure your messaging (on your website, in marketing communications, and in sales talking points) pulls those psychological levers that make people buy. Use what works and discard what doesn’t.
Examples of psychographics in action
Here’s an example of a real organization we helped with this technique. We used this method to bust assumptions and help them better serve a key customer segment.
The product : our client creates software that automatically calculates sales tax for e-commerce businesses. Companies doing business in the United States are sometimes required to collect sales tax at the point-of-sale, and different states have different tax rates.
The assumption : like most companies, our client segmented their customers based on organizational size (i.e. a demographic criterion), and the marketing team crafted the messaging accordingly.
What they learned through interviews : that they needed to segment based on entirely different criteria!
Segment #1 : mid-size and large companies with in-house accounting departments that kept them in compliance (or had the money to outsource it)
Segment #2 : small companies that did everything on their own
What’s the difference? Small companies knew they could be doing it wrong, and if they messed up, they might end up in jail (i.e. a psychographic criterion). Pretty valuable insight, wouldn’t you say?
With this psychographic data, they were able to adjust their website, product, and messaging to address that concern, and they increased sales based on this segment.
Collect psychographic information to guide your marketing campaigns
Creating fully fleshed-out buyer personas built with psychographics, demographics, and buyer behavior, can take your marketing campaigns, messaging and conversion rates to the next level.
But to create one, you need a way to hear from your buyers.
Hotjar puts you in direct contact with your target audience through surveys and interviews, so you can create buyer personas based on data rather than guesswork.
Ready to learn more about your audience? Try Hotjar for free, today!
Learn more about your customers with Hotjar!
Collect powerful psychographic data and figure out what drives customers to buy with tools like Hotjar’s Surveys and Engage.
Related articles

User research
5 tips to recruit user research participants that represent the real world
Whether you’re running focus groups for your pricing strategy or conducting usability testing for a new product, user interviews are one of the most effective research methods to get the needle-moving insights you need. But to discover meaningful data that helps you reach your goals, you need to connect with high-quality participants. This article shares five tips to help you optimize your recruiting efforts and find the right people for any type of research study.
Hotjar team

How to instantly transcribe user interviews—and swiftly unlock actionable insights
After the thrill of a successful user interview, the chore of transcribing dialogue can feel like the ultimate anticlimax. Putting spoken words in writing takes several precious hours—time better invested in sharing your findings with your team or boss.
But the fact remains: you need a clear and accurate user interview transcript to analyze and report data effectively. Enter automatic transcription. This process instantly transcribes recorded dialogue in real time without human help. It ensures data integrity (and preserves your sanity), enabling you to unlock valuable insights in your research.

Shadz Loresco

An 8-step guide to conducting empathetic (and insightful) customer interviews in mid-market companies
Customer interviews uncover your ideal users’ challenges and needs in their own words, providing in-depth customer experience insights that inform product development, new features, and decision-making. But to get the most out of your interviews, you need to approach them with empathy. This article explains how to conduct accessible, inclusive, and—above all—insightful interviews to create a smooth (and enjoyable!) process for you and your participants.

IMAGES
VIDEO
COMMENTS
An interview is a qualitative research method that relies on asking questions in order to collect data. Interviews involve two or more people, one of whom is the interviewer asking the questions. There are several types of interviews, often differentiated by their level of structure.
Interviewing people is at the heart of qualitative research. It is not merely a way to collect data but an intrinsically rewarding activity—an interaction between two people that holds the potential for greater understanding and interpersonal development. Unlike many of our daily interactions with others that are fairly shallow and mundane ...
Qualitative research method-interviewing and observation. Buckley and Chiang define research methodology as "a strategy or architectural design by which the researcher maps out an approach to problem-finding or problem-solving.". [ 1] According to Crotty, research methodology is a comprehensive strategy 'that silhouettes our choice and ...
This paper aims to provide an overview of the use and assessment of qualitative research methods in the health sciences. Qualitative research can be defined as the study of the nature of phenomena and is especially appropriate for answering questions of why something is (not) observed, assessing complex multi-component interventions, and focussing on intervention improvement.
On the other hand, Frances, et al., (2009) defined qualitative research interviews as the most commonly used method in data collection particularly in the fields of health and social research ...
What is a qualitative research interview? Qualitative research interviews are a mainstay among qualitative research techniques, and have been in use for decades either as a primary data collection method or as an adjunct to a wider research process. A qualitative research interview is a one-to-one data collection session between a researcher and a participant.
InterViews by Steinar Kvale Interviewing is an essential tool in qualitative research and this introduction to interviewing outlines both the theoretical underpinnings and the practical aspects of the process. After examining the role of the interview in the research process, Steinar Kvale considers some of the key philosophical issues relating ...
Interviews are one of the most promising ways of collecting qualitative data through establishment of a communication between researcher and the interviewee.
Summary. The qualitative research interview is a powerful data-collection tool which affords researchers in medical education opportunities to explore unknown areas of education and practice within medicine. This paper articulates 12 tips for consideration when conducting qualitative research interviews, and outlines the qualitative research ...
In-depth interviews are a versatile form of qualitative data collection used by researchers across the social sciences. They allow individuals to explain, in their own words, how they understand ...
Qualitative interviewing is a foundational method in qualitative research and is widely used in health research and the social sciences. Both qualitative semi-structured and in-depth unstructured interviews use verbal communication, mostly in face-to-face interactions, to collect data about the attitudes, beliefs, and experiences of participants.
Undertaking interviews is potentially the most important step in the qualitative research process. If you don't collect useful, useable data in your interviews, you'll struggle through the rest of your dissertation or thesis.
Interviews are most effective for qualitative research: They help you explain, better understand, and explore research subjects' opinions, behavior, experiences, phenomenon, etc. Interview questions are usually open-ended questions so that in-depth information will be collected.
The most common methods of data collection used in qualitative research are interviews and focus groups. While these are primarily conducted face-to-face, the ongoing evolution of digital ...
Qualitative research is the naturalistic study of social meanings and processes, using interviews, observations, and the analysis of texts and images. In contrast to quantitative researchers, whose statistical methods enable broad generalizations about populations (for example, comparisons of the percentages of U.S. demographic groups who vote in particular ways), qualitative researchers use ...
It is the most widely used method in qualitative research. It is flexible, inexpensive, and does not inter-fere with the researcher's life the way that ethnography does. This chapter looks at qualitative interviewing and how it compares to other types of collect-ing evidence in research, particularly structured interviewing and ethnography.
In an ongoing debate about using interview material in research, ethnomethodologists point to the fact that meaning is co-constructed in interview interactions and therefore interpretation of interview data should focus on processes of jointly generating meanings.
Following from this, the challenge for research using qualitative interview methodology is to move away from conceiving of interviews as a kind of 'tool' that permits a gaze into the interior lifeworlds of participants.
Abstract. Qualitative interviews are widely used in qualitative and mixed methods research designs in applied linguistics, including case studies, ethnographies, interview studies, and narrative research. This entry discusses commonly used forms of interviews and provides examples to show how researchers use interview accounts to generate ...
What is a qualitative research interview? Qualitative research interviews are a mainstay among qualitative research techniques, and have been in use for decades either as a primary data collection method or as an adjunct to a wider research process. A qualitative research interview is a one-to-one data collection session between a researcher and a participant.
Interviews are a common method of data collection in nursing research. They are frequently used alone in a qualitative study or combined with other data collection methods in mixed or multi-method research. Semi-structured interviews, where the researcher has some predefined questions or topics but then probes further as the participant ...
Observation in qualitative research "is one of the oldest and most fundamental research methods approaches. This approach involves collecting data using one's senses, especially looking and listening in a systematic and meaningful way" (McKechnie, 2008, p. 573).Similarly, Adler and Adler (1994) characterized observations as the "fundamental base of all research methods" in the social ...
Text-based vignettes are widely used within qualitative social work research yet there is little guidance on how to construct and integrate them into the research process. This article discusses th...
Aim(s) To conceptualise and identify characteristics of clinical leadership in the nursing home setting. Design A qualitative study using semi-structured focus group interviews and a thematic anal...
Interview Questions/Guide: The interview guide (Additional File 1) ... Interviews: Two women researchers, with PhD and Master's level training and expertise in qualitative research (CBJ, AA) conducted phone and video interviews (Zoom, Zoom Video Communications, San Jose, USA); Site A and B interviews were collected August to September 2021 ...
For this study, we used a subset of interview questions focused on evidence-use in the decision-making process, and the organizational structures or actors involved, in BC's early COVID-19 pandemic response (March-August 2020). Questions were adapted to be relevant to a respondent's expertise and particular involvement in the response.
A strategic sample of nine PRs and eight HPRs were interviewed individually between August 2022 and January 2023 using a semi-structured interview guide. We analysed data using an inductive content analysis. ... Sampling in interview-based qualitative research: a theoretical and practical guide. Qual Res Psychol. 2014;11(1):25-41.
Qualitative research within healthcare aims to uncover meaning, listen to the perspectives of key stakeholders, and build theories . Without qualitative exploration, subsequent quantitative work may overlook or misrepresent key factors for a particular health problem.
Four ways to collect psychographic data include non-scripted customer interviews, surveys, focus groups, and brainstorm sessions with internal stakeholders. Use psychographic research by: Reviewing the data with internal subject matter experts. Identifying your top selling points.