- Open access
- Published: 24 January 2023

Integrating case management for patients with complex needs in the ground practice: the importance of context in evaluative designs
- Catherine Hudon ORCID: orcid.org/0000-0001-6140-9916 1 &
- Rodger Kessler 2
Health Research Policy and Systems volume 21 , Article number: 9 ( 2023 ) Cite this article
4707 Accesses
1 Citations
3 Altmetric
Metrics details
Responding to complex needs calls for integrating care across providers, settings and sectors. Among models to improve integrated care, case management demonstrates a good evidence base of facilitating the appropriate delivery of healthcare services. Since case management is a complex, multi component intervention, with its component parts interacting in a non-linear manner, effectiveness is largely influenced by the context in which the intervention is implemented. This paper discusses how to respond to implementation challenges to evaluating complex interventions for patients with complex needs. Building on the example of case management, we suggest that documenting innovation effectiveness remains important, but that evaluation needs to include theory-based and systems perspectives. We also suggest that implementation science needs to be part of intervention design while engaging stakeholders to define the most relevant research questions and implementation effectiveness, to optimize successful implementation and sustainability.
Peer Review reports
Contributions to the literature
This paper suggests that evaluation of effectiveness by randomized controlled trials for complex interventions has structural limitations and discusses the pros and cons of such designs.
We propose examples of designs to evaluate the theory of the intervention, using the example of case management for people with complex needs.
It invites researchers and stakeholders to start implementation science early in intervention design to optimize adoption and sustainability.
Eighteen per cent of patients in primary healthcare face multiple interacting challenges among the physical, mental and social dimensions of health [ 1 ], having the most complex health needs (referred to, hereafter, as “complex needs”). These proportions increase with age, race, and ethnicity [ 2 ]. Per the inverse care law [ 3 ], with increased complexity of patient’s needs, comes decreased care availability and health equity, and thus decreased quality of life, and increased disability and mortality risk [ 4 ]. The COVID-19 pandemic has shone a light on the health inequities experienced by patients with complex needs [ 5 ]. Improving care and health equity for this population is a priority for healthcare systems worldwide [ 6 ].
Responding to complex needs calls for integrating care across providers, settings, and sectors. The World Health Organization suggests the following patient-led definition of integrated care: ‘My care is planned with people who work together to understand me and my carer(s), put me in control, coordinate and deliver services to achieve my best outcomes’ [ 7 ]. Reviews demonstrated the impact of integrated care on access and quality of care, patient satisfaction, and reduction of hospitalization [ 8 ].
Among models to improve integrated care, evidence supported case management [ 9 , 10 , 11 ] facilitates the appropriate delivery of healthcare services for patients with complex needs [ 7 ]. Case management is a highly variable, collaborative approach used to assess, plan, facilitate, and coordinate care to meet patient and family healthcare needs, through communication and coordination of available resources across all levels of health care as well as sectors outside of the health system [ 12 ].
When focusing on the care of patients with multiple clinical, behavioral and social dimensions that impact on functioning and health, interventions involve many partners and are often complex [ 13 ]. This requires interacting and collaborating with underlying organizational systems and subsystems and adaptive learning for rapid cycle changes. Multiple contextual issues such as the setting of implementation, providers involved, and organizational culture, need to be considered as part of implementation and generate issues requiring operational and clinical adaptation. Since case management is a non linear complex multi component intervention [ 14 ], effectiveness is largely influenced by the context in which the intervention is implemented [ 15 ].
To support the development and evaluation of complex interventions, the United Kingdom Medical Research Council (MRC) proposed an adapted phased approach [ 13 , 16 ]. Their four phases Framework, building on qualitative and quantitative evidence and includes development, feasibility/piloting, evaluation, and implementation [ 16 ]. It was recently updated to incorporate developments in complex intervention research [ 17 ]. This revised Framework introduces more emphases on the importance of context and the need of understanding interventions as events in systems that produce effects through interactions including contextual factors associated with implementation.
Successful implementation of interventions that respond to complex care needs is critical to improving healthcare systems- and outcomes [ 17 ]. This paper discusses how to respond to implementation challenges to evaluating complex interventions for patients with complex needs, building on the example of case management.
Evaluation and implementation science
Intervention effectiveness remains important.
Pragmatic randomized controlled trials [ 18 ] (RCTs) remain indispensable to develop the foundation of evidence about a new intervention and are essential to document internal validity [ 18 ]. Reviews of RCTs on case management, for example, documented reduction of emergency department costs and improvement of social and clinical outcomes (e.g. alcohol or drug use and social problems) for patients who frequently used the healthcare services [ 9 , 10 , 11 ].
However, there are multiple challenges in conducting RCTs of complex multi-level interventions in the ground practices with patients having complex needs. RCT designs have mainly focused on internal validity minimizing inherent organizational and clinical contextual variation and restrict patient populations [ 19 , 20 ]. In addition, the time, expense and need for controlled research environments limit the generalizability and utility of findings and often do not respond to the immediate need of the providers [ 21 ]. Partially because of this disconnect, limited biobehavioural research makes its way into practice [ 22 ]. Many reviews of RCTs conclude that the inability to translate RCT data into clinical care may limit their utility [ 18 , 20 ], and therefore many authors have proposed alternative designs to traditional RCTs [ 23 ]. Cluster randomization [ 24 ] at the practice level, acknowledges organizational and contextual variation and tests whether there are effects across practices, despite variation. At the patient level, stepped wedge [ 25 ] designs allow patients to serve as their own controls over time, with changes after intervention serving as key outcome indicators. Rather than controlling variation, it is expected and documented when reporting results. Contextual variation also helps to understand why it is so difficult to conduct meta-analysis of complex interventions with patients with complex needs. These meta-analyses of RCTs, very supportive when available, are not always feasible and cannot be the unique strategy of evaluation.
Many good RCTs concluding that an intervention is not effective are a strong argument against this intervention which will have to be significantly improved and re-evaluated. On the other hand, having almost all RCT findings documenting effectiveness of complex interventions targeting patients with complex needs remain unlikely because of variations in key ingredients of the intervention, populations recruited in the study or local contexts. Researchers and decision-makers will often have to contend with a situation between those ends.
Should we conduct a new RCT in each new context?
Some might argue we should conduct a new RCT in each new context that interventions will be implemented. A more pressing question is whether RCTs always the best designs in multi level interventions of complex patients. We suggest that there must be a balance between the internal validity RCT focus and the crucial external validity necessary for data to be taken seriously on the ground, keeping in mind that evidence is usually not the main issue when translating research into practice [ 26 ]. Translation of research into practice is challenging if local context is not well considered in replication. In addition to evidence, in real world, many feasibility aspects have to be considered in implementation design, such as budget, human resources, work-flows for intervention and monitoring, and contextual adaptation. Given limited resources and limited uptake of RCT data, investing resources into additional RCTs should be questioned, and perhaps may be unethical, if RCTs demonstrated the effectiveness in controlled settings and populations but have limited practice uptake. In that case, alternative less expensive and resource consuming designs may be more suitable to better understand contextual facilitators to increase on the ground uptake [ 27 ].
But evaluation goes beyond effectiveness
The revised MRC Framework outlines the importance of considering strategies to maximise the usefulness of research results to inform decision-making [ 17 ], in contrast to focusing exclusively on obtaining unbiased estimates of effectiveness [ 28 ]. Research questions should be developed in partnership with stakeholders, utilizing study designs that rapidly answer questions of stakeholder interest and promote adoption of findings. Beyond effectiveness, evaluation should inform the theory-based and the systems perspectives [ 17 ].
Many designs may help identifying key ingredients of complex interventions [ 29 ]. For example, different kinds of synthesis were conducted for case management with frequent users of healthcare services. A mixed systematic review [ 30 ] identified characteristics of case management that yield positive outcomes among frequent users with chronic disease in primary care. Sufficient and necessary characteristics were identified using configurational comparative methods (CCM) [ 31 , 32 , 33 ]. This review documented that it is necessary to identify patients most likely to benefit from the intervention for case management to produce positive outcomes. By definition, patient complexity is heterogeneous in clinical presentation, effect on quality of life, and available support resources. High-intensity intervention or the presence of a multidisciplinary/interorganizational care plan was also associated with positive outcomes.
The realist approaches offer an opportunity for complex interventions to be treated as complex systems [ 34 ]. Realist approaches focus not only on the outcomes, but also on the causal mechanisms that explain ‘how’ the outcomes were reached, and how context influenced outcomes [ 35 ]. Such a focus is particularly appropriate when seeking to better understand novel interventions with little information available on their effectiveness, those that have demonstrated mixed patterns and outcomes, and interventions that will be brought to broader scale [ 36 ]. For example, a realist synthesis [ 37 ] examined how and under what circumstances primary care case management improves outcomes among frequent users with chronic conditions [ 34 ]. This realist synthesis documented that the trusting relationship fostering patient and clinician engagement in the case management intervention was a key ingredient of the intervention [ 37 ].
Complex interventions are often embedded in changing organizations and systems including many parts interconnected that produce its own pattern of behavior over time [ 38 ]. ‘A systems perspective suggests that interventions can be better understood with an examination of the system(s) in which they are embedded or the systems that they set out to change’ [ 17 ]. Consideration of the relationships between the intervention and its multiple contextual factors is key [ 39 ]. Network analysis, for example, is an approach which can be used with other study designs to understand changing relationships among structures within a system of individuals or organizations [ 17 ]. Case management research for people with complex needs could benefit from this kind of analysis.
Implementation effectiveness starts with intervention design
An effective intervention needs to be designed to be useful, identifying important implementation considerations as the first phases of evaluation [ 17 ]. Identification of factors influencing implementation and effectiveness become a core element of research design [ 29 , 40 ]. Without being exhaustive, a few models can support research teams and stakeholders to consider implementation early in evaluation. The PRISM Practical, Robust Implementation and Sustainability Model—[ 41 ] proposes identifiable and measurable elements to assess context [ 42 ]. It evaluates how the healthcare program or intervention interacts with the recipients to influence program adoption, implementation, maintenance, reach, and effectiveness. Such application broadens identification of contextual factors and enriches our dynamic understanding of multi-layer interventions. Implementation questions should be asked concomitantly with effectiveness and other evaluation questions. Curran et al. [ 43 ] propose three hybrid designs to assess effectiveness and implementation: (1) testing effects of a clinical intervention on relevant outcomes while observing and gathering information on implementation; (2) dual testing of clinical and implementation interventions/strategies; and (3) testing of an implementation strategy while observing and gathering information on the clinical intervention’s impact on relevant outcomes [ 43 ]. Chambers et al. [ 44 ] propose the Dynamic Sustainability Framework involving continued learning and problem solving, and ongoing adaptation of complex interventions with a primary focus on fit between interventions and multi-level contexts, and expectations for ongoing improvement instead of implementation of fixed interventions at-risk of losing effectiveness over time [ 44 ]. A large part of implementation science research [ 45 ], therefore, ‘involves the development and evaluation of complex interventions to maximize effective implementation in practice and/or the policy of interventions that have already demonstrated effectiveness’ [ 17 ].
Barriers to and facilitators of effective implementation and contextual adaptation must be a core of evaluation strategy [ 17 ]. For example, a multiple embedded case study with a mixed-methods design identified characteristics and context of case management programs to help to improve patient self-management, experience of integrated care, and healthcare services use [ 46 ]. This study underscored the necessity of an experienced, knowledgeable and well-trained case manager with strong interpersonal skills to optimize case management programs implementation such that patients are more proactive in their care and their outcomes improve.
Early consideration of implementation implies involving stakeholders in all phases of development and evaluation of a complex intervention from the beginning, to ensure asking the most relevant research questions and increasing the potential an intervention be widely adopted [ 17 ]. Collaboration between researchers and knowledge users throughout a study or a research program is a strong predictor that findings will be used [ 47 ]. This collaboration may take different forms going from a consultation at certain phases of the study/research program to full engagement in all phases of the study [ 47 ].
Conclusions
RCTs remain indispensable to develop the foundation of evidence about a new intervention and are important to document effectiveness, but evaluation should go beyond effectiveness to include theory-based and systems perspectives, choosing the appropriate designs to answer research questions. Moreover, implementation effectiveness evaluation should start with intervention design. While conducting evaluation studies, engaging stakeholders to contribute defining the most relevant research questions and designs optimizes chances of adoption and sustainability.
Availability of data and materials
Not applicable.
Abbreviations
Randomized controlled trials
Coronavirus disease 2019
Medical Research Council
Configurational comparative methods
The Practical, Robust Implementation and Sustainability Model
de Oliveira CA, Weber B, Dos Santos JLF, et al. Health complexity assessment in primary care: a validity and feasibility study of the INTERMED tool. PLoS ONE. 2022;17: e0263702.
Article CAS Google Scholar
Buttorff C, Ruder T, Bauman M. Multiple chronic conditions in the United States. Santa Monica, CA: Rand. 2017. https://www.rand.org/pubs/tools/TL221.html . Accessed 12 Dec 2022.
Marmot M. An inverse care law for our time. BMJ. 2018;362: k3216.
Article Google Scholar
Schoen C, Osborn R, Squires D, Doty M, Pierson R, Applebaum S. New 2011 survey of patients with complex care needs in eleven countries finds that care is often poorly coordinated. Health Aff. 2011;30:2437–48.
Government of Canada. Reducing COVID-19 risk in community settings: A tool for operators. https://www.canada.ca/en/public-health/services/publications/diseases-conditions/vulnerable-populations-covid-19.html . (2020). Accessed 30 May 2022.
Blumenthal D, Chernof B, Fulmer T, Lumpkin J, Selberg J. Caring for high-need, high-cost patients: an urgent priority. N Engl J Med. 2016;375:909–11.
World Health Organization. Integrated care models: an overview. https://www.euro.who.int/__data/assets/pdf_file/0005/322475/Integrated-care-models-overview.pdf . (2016). Accessed 30 May 2022.
Baxter S, Johnson M, Chambers D, Sutton A, Goyder E, Booth A. The effects of integrated care: a systematic review of UK and international evidence. BMC Health Serv Res. 2018;18:350.
Althaus F, Paroz S, Hugli O, et al. Effectiveness of interventions targeting frequent users of emergency departments: a systematic review. Ann Emerg. 2011;58:41–52.
Kumar GS, Klein R. Effectiveness of case management strategies in reducing emergency department visits in frequent user patient populations: a systematic review. J Emerg Med. 2013;44:717–29.
Soril L, Legget L, Lorenzetti D, Noseworthy T. Reducing frequent visits to the emergency department: a systematic review of intervention. PLOS One. 2015;10.
What is a case manager? http://cmsa.org/who-we-are/what-is-a-case-manager/ . Accessed 30 May 2022.
Campbell M, Fitzpatrick R, Haines A, et al. Framework for design and evaluation of complex interventions to improve health. BMJ. 2000;321:694–6.
Nurjono M, Yoong J, Yap P, Wee SL, Vrijhoef HJM. Implementation of integrated care in Singapore: a complex adaptive system perspective. Int J Integr Care. 2018;18:4.
Dopson S, Fitzgerald L, Ferlie E. Understanding change and innovation in healthcare settings: reconceptualizing the active role of context. J Change Manag. 2008;8:213–31.
Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ. 2008;337: a1655.
Skivington K, Matthews L, Simpson SA, et al. Framework for the development and evaluation of complex interventions: gap analysis, workshop and consultation-informed update. HTA. 2021;25:1–132.
Google Scholar
Ford I, Norrie J. Pragmatic trials. N Engl J Med. 2016;375:454–63.
Khorsan R, Crawford C. How to assess the external validity and model validity of therapeutic trials: a conceptual approach to systematic review methodology. Evid Based Complement Alternat Med. 2014;2014:694804.
Kessler R, Glasgow RE. A proposal to speed translation of healthcare research into practice: dramatic change is needed. Am J Prev Med. 2011;40:637–44.
Peek CJ, Glasgow RE, Stange KC, Klesges LM, Purcell EP, Kessler RS. The 5 R’s: an emerging bold standard for conducting relevant research in a changing world. Ann Fam Med. 2014;12:447–55.
Green LW. Making research relevant: if it is an evidence-based practice, where’s the practice-based evidence? Fam Pract. 2008;25(Suppl 1):i20–4.
Sanson-Fisher RW, Bonevski B, Green LW, D’Este C. Limitations of the randomized controlled trial in evaluating population-based health interventions. Am J Prev Med. 2007;33:155–61.
Dickinson LM, Beaty B, Fox C, et al. Pragmatic cluster randomized trials using covariate constrained randomization: a method for practice-based research networks (PBRNs). J Am Board Fam Med. 2015;28:663–72.
Hughes JP, Granston TS, Heagerty PJ. Current issues in the design and analysis of stepped wedge trials. Contemp Clin. 2015;45:55–60.
Umscheid CA, Williams K, Brennan PJ. Hospital-based comparative effectiveness centers: translating research into practice to improve the quality, safety and value of patient care. J Gen Intern. 2010;25:1352–5.
Hanley P, Chambers B, Haslam J. Reassessing RCTs as the ‘gold standard’: synergy not separatism in evaluation designs. Int J Res Method Educ. 2016;39:287–98.
Deaton A, Cartwright N. Understanding and misunderstanding randomized controlled trials. Soc Sci Med. 2018;210:2–21.
Petticrew M, Rehfuess E, Noyes J, et al. Synthesizing evidence on complex interventions: how meta-analytical, qualitative, and mixed-method approaches can contribute. J Clin Epidemiol. 2013;66:1230–43.
Hudon C, Chouinard MC, Pluye P, et al. Characteristics of case management in primary care associated with positive outcomes for frequent users of healthcare: a systematic review. Ann Fam Med. 2019;17:448–58.
Dy SM, Garg P, Nyberg D, et al. Critical pathway effectiveness: assessing the impact of patient, hospital care, and pathway characteristics using qualitative comparative analysis. Health Serv Res. 2005;40:499–516.
Berg-Schlosser D, Meur G, le D, Rihoux B, Ragin CC. Configurational comparative methods: qualitative comparative analysis (QCA) and related techniques. Thousand Oaks, California: SAGE Publications, Inc. 2009. https://methods.sagepub.com/book/configurational-comparative-methods . Accessed 12 Dec 2022.
Hong QN, Pluye P, Bujold M, Wassef M. Convergent and sequential synthesis designs: implications for conducting and reporting systematic reviews of qualitative and quantitative evidence. Syst Rev. 2017;6:61.
Pawson R, Tilley N. Realistic evaluation. London: Sage; 1997.
Wong G, Westhorp G, Manzano A, Greenhalgh J, Jagosh J, Greenhalgh T. RAMESES II reporting standards for realist evaluations. BMC Med. 2016;14:96.
Wong G, Greenhalgh T, Westhorp G, Pawson R. Realist methods in medical education research: what are they and what can they contribute? Med Educ. 2012;46:89–96.
Hudon C, Chouinard MC, Aubrey-Bassler K, et al. Case management in primary care for frequent users of health care services: a realist synthesis. Ann Fam Med. 2020;18:218–26.
Meadows DH, Wright D, Wright D. Thinking in systems : a primer. White River Junction, Vermont: Chelsea Green Publishing; 2008.
Williams B. Prosaic or profound? The adoption of systems ideas by impact evaluation. Inst Develop Stud. 2015;46:7–16.
Hudon C, Chouinard M-C, Lambert M, Diadiou F, Bouliane D, Beaudin J. Key factors of case management interventions for frequent users of healthcare services: a thematic analysis review. BMJ Open. 2017;7: e017762.
Feldstein AC, Glasgow RE. A practical, robust implementation and sustainability model (PRISM) for integrating research findings into practice. Jt Comm J Qual Patient Saf. 2008;34:228–43.
McCreight MS, Rabin BA, Glasgow RE, et al. Using the Practical, Robust Implementation and Sustainability Model (PRISM) to qualitatively assess multilevel contextual factors to help plan, implement, evaluate, and disseminate health services programs. Transl Behav Med. 2019;9:1002–11.
Curran GM, Bauer M, Mittman B, Pyne JM, Stetler C. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care. 2012;50:217–26.
Chambers DA, Glasgow RE, Stange KC. The dynamic sustainability framework: addressing the paradox of sustainment amid ongoing change. Implement Sci. 2013;8:117.
Eccles MP, Mittman BS. Welcome to implementation science. Implement Sci. 2006;1.
Hudon C, Chouinard MC, Bisson M, et al. Case management programs for improving integrated care for frequent users of healthcare services: an implementation analysis. Int J Integr Care. 2022;22:11.
Canadian Institutes of Health Research. Knowledge user engagement. http://www.cihr-irsc.gc.ca/e/49505.html . (2016). Accessed Dec 12 2022.
Download references
Acknowledgements
Author information, authors and affiliations.
Department of Family and Emergency Medicine, Université de Sherbrooke, Pavillon Z7-local 3007, 3001, 12eAvenue Nord, Sherbrooke, QC, J1H 5N4, Canada
Catherine Hudon
Department of Family Medicine, University of Colorado School of Medecine, Aurora, CO, United States of America
Rodger Kessler
You can also search for this author in PubMed Google Scholar
Contributions
C.H. wrote a first draft of the manuscript which was reviewed and improved by R.K. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Catherine Hudon .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Hudon, C., Kessler, R. Integrating case management for patients with complex needs in the ground practice: the importance of context in evaluative designs. Health Res Policy Sys 21 , 9 (2023). https://doi.org/10.1186/s12961-023-00960-4
Download citation
Received : 08 August 2022
Accepted : 09 January 2023
Published : 24 January 2023
DOI : https://doi.org/10.1186/s12961-023-00960-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Complex interventions
- Implementation science
- Integrated care
- Case management
Health Research Policy and Systems
ISSN: 1478-4505
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Health Services Management: A Case Study Approach, Eleventh Edition
Ann scheck mcalearney, scd anthony r. kovner, phd.
- Member Price: $63.00
- Non Member Price: $90.00
- Delivery of Care
- Service Line Management
Book Description
Instructor Resources: Instructor’s Manual NEW EDITION COMING AUGUST 2023! Today’s healthcare managers face increasingly complex challenges and often must make decisions quickly. When a difficult situation arises, managers can no longer simply “look it up” online or in the management literature. Properly “looking it up” involves knowing where and how to look, appropriately framing a research question, weighing valid evidence, and understanding what is required to make proposed solutions work. Health Services Management: A Case Study Approach offers a diverse collection of case studies to help readers learn and apply key concepts of management, with an emphasis on the use of evidence in management practice. The case study authors, many of whom are practitioners or academics who work closely with practitioners, present realistic management challenges across a variety of settings. They examine potential responses to those challenges by health services managers and other stakeholders, and they provide a platform for meaningful discussion of opportunities and constraints for management decision makers attempting to implement change. This edition includes 60 case studies—32 of which are brand new—arranged thematically into six sections: The Role of the Manager, Control, Organizational Design, Professional Integration, Adaptation, and Accountability. The new cases include the following: • Better Metrics for Financial Management • What Makes a Patient-Centered Medical Home? • Doing the Right Thing When the Financials Do Not Support Palliative Care • Hearing the Patient Voice: Working with Patient and Family Advisers to Improve the Patient Experience • Managed Care Cautionary Tale: A Case Study in Risk Adjustment and Patient Dumping Learning by example is one of the oldest forms of learning, and the case study approach offers a time-tested way for students and healthcare professionals to develop practical skills that are not easily acquired through lectures. Health Services Management has been used in classrooms since 1978, and this eleventh edition offers a fresh take on a classic text.
- Table of Contents (PDF)
- Preface (PDF)
- Book Excerpt (PDF)
- Transition Guide
- Instructor Resource Sample
- PURCHASE EBOOK FROM VITALSOURCE (INGRAM)
- PURCHASE EBOOK FROM REDSHELF
- PURCHASE EBOOK FROM CHEGG

Evidence-Based Management in Healthcare: Principles, Cases, and Perspectives, Second Edition
The United States Healthcare System: Overview, Driving Forces, and Outlook for the Future
The Middleboro Casebook: Healthcare Strategy and Operations, Second Edition
WebwBorder-36256d52.jpg?w=160)
The Best Patient Experience: Helping Physicians Improve Care, Satisfaction, and Scores
Readmission Prevention: Solutions Across the Provider Continuum
The Core Elements of Value in Healthcare
Risk Management and the Emergency Department: Executive Leadership for Protecting Patients and Hospitals
Dimensions of Long-Term Care Management: An Introduction, Second Edition
Fundamentals of Medical Practice Management
A Physician Guidebook to The Best Patient Experience
World Health Systems: Challenges and Perspectives, Second Edition
The Middleboro Casebook: Healthcare Strategy and Operations, Third Edition
Evaluating the Healthcare System: Effectiveness, Efficiency, and Equity, Fourth Edition
Health Services Management: A Case Study Approach, Twelfth Edition
Dimensions of Long-Term Care Management: An Introduction, Third Edition
Fundamentals of Medical Practice Management, Second Edition
Healthcare in the United States: Clinical, Financial, and Operational Dimensions
Inspired to Change: Improving Patient Care One Story at a Time

Accountable Care Organizations: Your Guide to Strategy, Design, and Implementation
Healthcare in the United States: Clinical, Financial, and Operational Dimensions, Second Edition
- Utility Menu
harvardchan_logo.png

Harvard T.H. Chan School of Public Health Case-Based Teaching & Learning Initiative
Teaching cases & active learning resources for public health education, case library.
The Harvard Chan Case Library is a collection of teaching cases with a public health focus, written by Harvard Chan faculty, case writers, and students, or in collaboration with other institutions and initiatives.
Use the filters at right to search the case library by subject, geography, health condition, and representation of diversity and identity to find cases to fit your teaching needs. Or browse the case collections below for our newest cases, cases available for free download, or cases with a focus on diversity.
Using our case library
Access to cases.
Many of our cases are available for sale through Harvard Business Publishing in the Harvard T.H. Chan case collection . Others are free to download through this website .
Cases in this collection may be used free of charge by Harvard Chan course instructors in their teaching. Contact Allison Bodznick , Harvard Chan Case Library administrator, for access.
Access to teaching notes
Teaching notes are available as supporting material to many of the cases in the Harvard Chan Case Library. Teaching notes provide an overview of the case and suggested discussion questions, as well as a roadmap for using the case in the classroom.
Access to teaching notes is limited to course instructors only.
- Teaching notes for cases available through Harvard Business Publishing may be downloaded after registering for an Educator account .
- To request teaching notes for cases that are available for free through this website, look for the "Teaching note available for faculty/instructors " link accompanying the abstract for the case you are interested in; you'll be asked to complete a brief survey verifying your affiliation as an instructor.
Using the Harvard Business Publishing site
Faculty and instructors with university affiliations can register for Educator access on the Harvard Business Publishing website, where many of our cases are available . An Educator account provides access to teaching notes, full-text review copies of cases, articles, simulations, course planning tools, and discounted pricing for your students.

What's New
Atkinson, M.K. , 2023. Organizational Resilience and Change at UMass Memorial , Harvard Business Publishing: Harvard T.H. Chan School of Public Health. Available from Harvard Business Publishing Abstract The UMass Memorial Health Care (UMMHC or UMass) case is an examination of the impact of crisis or high uncertainty events on organizations. As a global pandemic unfolds, the case examines the ways in which UMMHC manages crisis and poses questions around organizational change and opportunity for growth after such major events. The case begins with a background of UMMHC, including problems the organization was up against before the pandemic, then transitions to the impact of crisis on UMMHC operations and its subsequent response, and concludes with challenges that the organization must grapple with in the months and years ahead. A crisis event can occur at any time for any organization. Organizational leaders must learn to manage stakeholders both inside and outside the organization throughout the duration of crisis and beyond. Additionally, organizational decision-makers must learn how to deal with existing weaknesses and problems the organization had before crisis took center stage, balancing those challenges with the need to respond to an emergency all the while not neglecting major existing problem points. This case is well-suited for courses on strategy determination and implementation, organizational behavior, and leadership.
The case describes the challenges facing Shlomit Schaal, MD, PhD, the newly appointed Chair of UMass Memorial Health Care’s Department of Ophthalmology. Dr. Schaal had come to UMass in Worcester, Massachusetts, in the summer of 2016 from the University of Louisville (KY) where she had a thriving clinical practice and active research lab, and was Director of the Retina Service. Before applying for the Chair position at UMass she had some initial concerns about the position but became fascinated by the opportunities it offered to grow a service that had historically been among the smallest and weakest programs in the UMass system and had experienced a rapid turnover in Chairs over the past few years. She also was excited to become one of a very small number of female Chairs of ophthalmology programs in the country.
Dr. Schaal began her new position with ambitious plans and her usual high level of energy, but immediately ran into resistance from the faculty and staff of the department. The case explores the steps she took, including implementing a LEAN approach in the department, and the leadership approaches she used to overcome that resistance and build support for the changes needed to grow and improve ophthalmology services at the medical center.
This case describes efforts to promote racial equity in healthcare financing from the perspective of one public health organization, Community Care Cooperative (C3). C3 is a Medicaid Accountable Care Organization–i.e., an organization set up to manage payment from Medicaid, a public health insurance option for low-income people. The case describes C3’s approach to addressing racial equity from two vantage points: first, its programmatic efforts to channel financing into community health centers that serve large proportions of Black, Indigenous, People of Color (BIPOC), and second, its efforts to address racial equity within its own internal operations (e.g., through altering hiring and promotion processes). The case can be used to help students understand structural issues pertaining to race in healthcare delivery and financing, to introduce students to the basics of payment systems in healthcare, and/or to highlight how organizations can work internally to address racial equity.
Kerrissey, M.J. & Kuznetsova, M. , 2022. Killing the Pager at ZSFG , Harvard Business Publishing: Harvard T.H. Chan School of Public Health case collection. Available from Harvard Business Publishing Abstract This case is about organizational change and technology. It follows the efforts of one physician as they try to move their department past using the pager, a device that persisted in American medicine despite having long been outdated by superior communication technology. The case reveals the complex organizational factors that have made this persistence possible, such as differing interdepartmental priorities, the perceived benefits of simple technology, and the potential drawbacks of applying typical continuous improvement approaches to technology change. Ultimately the physician in the case is not able to rid their department of the pager, despite pursuing a thorough continuous improvement effort and piloting a viable alternative; the case ends with the physician having an opportunity to try again and asks students to assess whether doing so is wise. The case can be used in class to help students apply the general concepts of organizational change to the particular context of technology, discuss the forces of stasis and change in medicine, and to familiarize students with the uses and limits of continuous improvement methods.
Yatsko, P. & Koh, H. , 2021. Dr. Joan Reede and the Embedding of Diversity, Equity, and Inclusion at Harvard Medical School , Harvard T.H. Chan School of Public Health case collection. Available from Harvard Business Publishing Abstract For more than 30 years, Dr. Joan Reede worked to increase the diversity of voices and viewpoints heard at Harvard Medical School (HMS) and at its affiliate teaching hospitals and institutes. Reede, HMS’s inaugural dean for Diversity and Community Partnership, as well as a professor and physician, conceived and launched more than 20 programs to improve the recruitment, retention, and promotion of individuals from racial and ethnic groups historically underrepresented in medicine (UiMs). These efforts have substantially diversified physician faculty at HMS and built pipelines for UiM talent into academic medicine and biosciences. Reede helped embed the promotion of diversity, equity, and inclusion (DEI) not only into Harvard Medical School’s mission and community values, but also into the DEI agenda in academic medicine nationally. To do so, she found allies and formed enduring coalitions based on shared ownership. She bootstrapped and hustled for resources when few readily existed. And she persuaded skeptics by building programs using data-driven approaches. She also overcame discriminatory behaviors and other obstacles synonymous with being Black and female in American society. Strong core values and sense of purpose were keys to her resilience, as well as to her leadership in the ongoing effort to give historically marginalized groups greater voice in medicine and science.
Cases Available for Free Download
Weinberger, E. , 2014. The Governor Is Very Interested, or, Cost-Effectiveness Analysis for School Health Screenings , Harvard T.H. Chan School of Public Health: Strategic Training Initiative for the Prevention of Eating Disorders (STRIPED). Download free of charge Abstract Nefertiti Nelson, a senior official at the Columbia Department of Public Health (CDPH) in the fictitious U.S. state of Columbia, has been asked by the governor’s office to examine the cost-effectiveness of administering BMI and eating disorders screenings in schools. To carry out the project, Nefertiti and her team of CDPH colleagues join forces with the consulting firm, Datamon; yet, as the analysis begins questions quickly arise about the logistics and costliness of implementing the screenings, potential outcome measures, and the interests and concerns of respective stakeholders. Teaching note available for faculty/instructors .
Weinberger, E. , 2017. Coloring the Narrative: How to Use Storytelling to Create Social Change in Skin Tone Ideals , Harvard T.H. Chan School of Public Health: Strategic Training Initiative for the Prevention of Eating Disorders (STRIPED). Download free of charge Abstract Many millions of people around the world experience the pervasive, and often painful, societal messages of colorism, where lighter skin tones are asserted to be more attractive and to reflect greater affluence, power, education, and social status. Even in places where the destructive effects of colorism are fairly well understood, far less is known about the problem of skin-lightening (really, it’s “skin bleaching”) creams and lotions, and the health risks that consumers assume with these products. In this teaching case, the protagonists are two women who have recently immigrated to the United States from Nigeria and Thailand, both with a life-time of experience with these products like many of the women of their home countries. As the story unfolds, they struggle along with the rest of the characters to copy with the push and pull of community norms vs. commercial influences and the challenge of promoting community health in the face of many societal and corporate obstacles. How can the deeply ingrained messages of colorism be effectively confronted and transformed to advance social change without alienating the community members we may most want to reach? Teaching note and supplemental slides available for faculty/instructors .
Gordon, R., Rottingen, J.-A. & Hoffman, S. , 2014. The Meningitis Vaccine Project , Harvard University: Global Health Education and Learning Incubator. Access online Abstract This case follows the vaccine development for Meningitis A, a disease that routinely caused deadly epidemics in Sub-Saharan Africa. The case explores why such a vaccine had not been developed previously and how the creation of the Meningitis Vaccine Project (MVP) - a partnership between the World Health Organization (WHO) and PATH, a non-governmental organization - enabled the vaccine to be successfully developed over 10 years by creating a novel product development partnership. Students examine why the public/private partnership was successful and how such a model could be applied to the development of other vaccines and health technologies. Additionally, the case explores the strategies applied by Marc LaForce, the MVP’s director and veteran public health advocate, to make the MVP a success. In particular, the case examines the management skills LaForce exercised during his tenure to develop a vaccine that affected African countries could afford through their own health budgets.
Alidina, S., Paulus, J. & Kane, N.M. , 2009. Malaria and DDT in Uganda , Harvard Business Publishing: Harvard T.H. Chan School of Public Health case collection. Download free of charge Abstract In October 2008, Dr. Richard Mgaga, Head of the Malaria Control Programme in Uganda reviewed the monthly malaria statistics report for the district of Apac, which in April of 2008 had undergone a pilot indoor residual spraying (IRS) program using DDT in a campaign to prevent mosquitoes from biting and spreading malaria. The campaign was halted by a court injunction requested by organic farmers, exporters and environmentalists in May 2008, and the injunction was upheld by the High Court in June. In early August, the Uganda Health Ministry began spraying a pyrethroid insecticide in place of DDT. Meanwhile the Ugandan Attorney General was challenging the High Court’s decision. Dr. Mugaga was under pressure by the Presidential Malaria Initiative (PMI) to undertake a full program of IRS in 300,000 households in the northern districts of Uganda, including Apac. However, he was unsure whether to proceed, given the opposition and apparent problems that surfaced when the Apac pilot was implemented. Teaching note available for faculty/instructors .
Weinberger, E. , 2015. Retweet Does Not Imply Endorsement: The Logic of Cyberbullying in Schools , Harvard T.H. Chan School of Public Health: Strategic Training Initiative for the Prevention of Eating Disorders (STRIPED). Download free of charge Abstract School nurse Hazel O’Leary and her supportive principal, Jamal Morden-Jones, strive to effectively respond to weight-related cyberbullying at their middle school. While there is a district-wide bullying prevention and intervention program guide that supposedly has all the necessary guidance on the subject, the duo still find themselves scrambling to implement the plan in the school, highlighting the gap between policy and practice. As the case study ends, Hazel prepares to initiate her school’s first foray into the world of logic models for public health program planning. Teaching note available for faculty/instructors .
Focus on Diversity, Equity, and Inclusion
Guerra, I., et al. , 2019. SALUDos: Healthcare for Migrant Seasonal Farm Workers , Harvard University: Social Medicine Consortium. Download free of charge Abstract The SALUDos program began in 2008 as a response to an influx of migrant seasonal farm workers (MSFWs) at a mobile medical unit serving homeless persons in Santa Clara County in Northern California. The program offered patients free and low-cost primary care services, linkage to resources, and advocacy. As the farm workers involved in this program became more involved in their primary care, they advocated for evening hours, transportation, linkage to coverage programs, and health education resources to better understand their medical and psychological conditions. During continual modifications of the SALUDos program, the team sought to understand and address large-scale social forces affecting migrant health through interventions to mitigate health inequities. Teaching note available for faculty/instructors.
This module will present two unfolding case studies based on real-world, actual events. The cases will require participants to review videos embedded into three modules and a summary module: Introduction to Concepts of Social Determinant of Health and Seeking Racial Equity Case Study on Health and Healthcare Context - Greensboro Health Disparities Collaborative (GHDC) Case Study on Social and Community Context - Renaissance Community Cooperative (RCC) Summary (Optional)
The learning objectives for the modules are related to achieving the Healthy People 2020 Social Determinants of Health Objectives – specifically the (1) Health and Healthcare Context, and (2) Social and Community Context.
On February 1, 2020, Jessie Gaeta, the chief medical officer for Boston Health Care for the Homeless Program (BHCHP), received news that a student in Boston had tested positive for the novel coronavirus virus that causes COVID-19 disease. Since mid-January, Gaeta had been following reports of the mysterious virus that had been sickening people in China. Gaeta was concerned. Having worked for BHCHP for 18 years, she understood how vulnerable people experiencing homelessness were to infectious diseases. She knew that the nonprofit program, as the primary medical provider for Boston’s homeless population, would have to lead the city’s response for that marginalized community. She also knew that BHCHP, as the homeless community’s key medical advocate, not only needed to alert local government, shelters, hospitals, and other partners in the city’s homeless support network, but do so in a way that spurred action in time to prevent illness and death.
The case study details how BHCHP’s nine-person incident command team quickly reorganized the program and built a detailed response, including drastically reducing traditional primary care services, ramping up telehealth, and redeploying and managing staff. It describes how the team worked with partners and quickly designed, staffed, and made operational three small alternative sites for homeless patients, despite numerous challenges. The case then ends with an unwelcome discovery: BHCHP’s first universal testing event at a large city shelter revealed that one-third of nearly 400 people there had contracted COVID-19, that most of the infected individuals did not report symptoms, and that other large city shelters were likely experiencing similar outbreaks. To understand how BHCHP and its partners subsequently popped up within a few days a 500-bed field hospital, which BHCHP managed and staffed for the next two months, see Boston Health Care for the Homeless (B): Disaster Medicine and the COVID-19 Pandemic.
Al Kasir, A., Coles, E. & Siegrist, R. , 2019. Anchoring Health beyond Clinical Care: UMass Memorial Health Care’s Anchor Mission Project , Harvard Business Publishing: Harvard T.H. Chan School of Public Health case collection. Available from Harvard Business Publishing Abstract As the Chief Administrative Officer of UMass Memorial Health Care (UMMHC) and president of UMass Memorial (UMM) Community Hospitals, Douglas Brown had just received unanimous and enthusiastic approval to pursue his "Anchor Mission" project at UMMHC in Worcester, Massachusetts. He was extremely excited by the board's support, but also quite apprehensive about how to make the Anchor Mission a reality. Doug had spearheaded the Anchor Mission from its earliest exploratory efforts. The goal of the health system's Anchor Mission-an idea developed by the Democracy Collaborative, an economic think tank-was to address the social determinants of health in its community beyond the traditional approach of providing excellent clinical care. He had argued that UMMHC had an obligation as the largest employer and economic force in Central Massachusetts to consider the broader development of the community and to address non-clinical factors, like homelessness and social inequality that made people unhealthy. To achieve this goal, UMMHC's Anchor Mission would undertake three types of interventions: local hiring, local sourcing/purchasing, and place-based community investment projects. While the board's enthusiasm was palpable and inspiring, Doug knew that sustaining it would require concrete accomplishments and a positive return on any investments the health system made in the project. The approval was just the first step. Innovation and new ways of thinking would be necessary. The bureaucracy behind a multi-billion-dollar healthcare organization would need to change. Even the doctors and nurses would need to change! He knew that the project had enormous potential but would become even more daunting from here.
Filter cases
Author affiliation.
- Harvard T.H. Chan School of Public Health (98) Apply Harvard T.H. Chan School of Public Health filter
- Harvard Business School (22) Apply Harvard Business School filter
- Global Health Education and Learning Incubator at Harvard University (12) Apply Global Health Education and Learning Incubator at Harvard University filter
- Strategic Training Initiative for the Prevention of Eating Disorders (STRIPED) (11) Apply Strategic Training Initiative for the Prevention of Eating Disorders (STRIPED) filter
- Social Medicine Consortium (8) Apply Social Medicine Consortium filter
- Harvard Kennedy School of Government (1) Apply Harvard Kennedy School of Government filter
- Harvard Malaria Initiative (1) Apply Harvard Malaria Initiative filter
- Women, Gender, and Health interdisciplinary concentration (1) Apply Women, Gender, and Health interdisciplinary concentration filter
Geographic focus
- United States (63) Apply United States filter
- Massachusetts (14) Apply Massachusetts filter
- International/multiple countries (11) Apply International/multiple countries filter
- California (6) Apply California filter
- Mexico (4) Apply Mexico filter
- India (3) Apply India filter
- Israel (3) Apply Israel filter
- New York (3) Apply New York filter
- Bangladesh (2) Apply Bangladesh filter
- Colorado (2) Apply Colorado filter
- Guatemala (2) Apply Guatemala filter
- Haiti (2) Apply Haiti filter
- Japan (2) Apply Japan filter
- Kenya (2) Apply Kenya filter
- South Africa (2) Apply South Africa filter
- Uganda (2) Apply Uganda filter
- United Kingdom (2) Apply United Kingdom filter
- Washington state (2) Apply Washington state filter
- Australia (1) Apply Australia filter
- Cambodia (1) Apply Cambodia filter
- China (1) Apply China filter
- Connecticut (1) Apply Connecticut filter
- Egypt (1) Apply Egypt filter
- El Salvador (1) Apply El Salvador filter
- Honduras (1) Apply Honduras filter
- Liberia (1) Apply Liberia filter
- Louisiana (1) Apply Louisiana filter
- Maine (1) Apply Maine filter
- Michigan (1) Apply Michigan filter
- Minnesota (1) Apply Minnesota filter
- New Jersey (1) Apply New Jersey filter
- Nigeria (1) Apply Nigeria filter
- Pakistan (1) Apply Pakistan filter
- Philippines (1) Apply Philippines filter
- Rhode Island (1) Apply Rhode Island filter
- Turkey (1) Apply Turkey filter
- Washington DC (1) Apply Washington DC filter
- Zambia (1) Apply Zambia filter
Case availability & pricing
- Available for purchase from Harvard Business Publishing (73) Apply Available for purchase from Harvard Business Publishing filter
- Download free of charge (50) Apply Download free of charge filter
- Request from author (4) Apply Request from author filter
Case discipline/subject
- Healthcare management (55) Apply Healthcare management filter
- Social & behavioral sciences (41) Apply Social & behavioral sciences filter
- Health policy (35) Apply Health policy filter
- Global health (28) Apply Global health filter
- Multidisciplinary (16) Apply Multidisciplinary filter
- Child & adolescent health (15) Apply Child & adolescent health filter
- Marketing (15) Apply Marketing filter
- Environmental health (12) Apply Environmental health filter
- Human rights & health (11) Apply Human rights & health filter
- Social innovation & entrepreneurship (11) Apply Social innovation & entrepreneurship filter
- Women, gender, & health (11) Apply Women, gender, & health filter
- Finance & accounting (10) Apply Finance & accounting filter
- Population health (8) Apply Population health filter
- Social medicine (7) Apply Social medicine filter
- Epidemiology (6) Apply Epidemiology filter
- Nutrition (6) Apply Nutrition filter
- Technology (6) Apply Technology filter
- Ethics (5) Apply Ethics filter
- Life sciences (5) Apply Life sciences filter
- Quality improvement (4) Apply Quality improvement filter
- Quantative methods (3) Apply Quantative methods filter
- Maternal & child health (1) Apply Maternal & child health filter
Health condition
- Cancer (3) Apply Cancer filter
- COVID-19 (3) Apply COVID-19 filter
- Obesity (3) Apply Obesity filter
- Breast cancer (2) Apply Breast cancer filter
- Disordered eating (2) Apply Disordered eating filter
- Ebola (2) Apply Ebola filter
- Influenza (2) Apply Influenza filter
- Injury (2) Apply Injury filter
- Malaria (2) Apply Malaria filter
- Alcohol & drug use (1) Apply Alcohol & drug use filter
- Asthma (1) Apply Asthma filter
- Breast implants (1) Apply Breast implants filter
- Cardiovascular disease (1) Apply Cardiovascular disease filter
- Cervical cancer (1) Apply Cervical cancer filter
- Cholera (1) Apply Cholera filter
- Food poisoning (1) Apply Food poisoning filter
- HPV (1) Apply HPV filter
- Malnutrition (1) Apply Malnutrition filter
- Meningitis (1) Apply Meningitis filter
- Opioids (1) Apply Opioids filter
- Psychological trauma (1) Apply Psychological trauma filter
- Road traffic injury (1) Apply Road traffic injury filter
- Sharps injury (1) Apply Sharps injury filter
- Skin bleaching (1) Apply Skin bleaching filter
Diversity and Identity
- Female protagonist (13) Apply Female protagonist filter
- Health of diverse communities (11) Apply Health of diverse communities filter
- Protagonist of color (5) Apply Protagonist of color filter
Supplemental teaching material
- Teaching note available (70) Apply Teaching note available filter
- Multi-part case (18) Apply Multi-part case filter
- Additional teaching materials available (12) Apply Additional teaching materials available filter
- Simulation (2) Apply Simulation filter
- Teaching pack (2) Apply Teaching pack filter
- Teaching example (1) Apply Teaching example filter
Browse our case library
Weinberger, E. , 2014. Beauty and the Breast: Mobilizing Community Action to Take on the Beauty Industry , Harvard T.H. Chan School of Public Health: Strategic Training Initiative for the Prevention of Eating Disorders (STRIPED). Download free of charge Abstract How does one learn to become an effective advocate? “Beauty and the Breast: Mobilizing Community Action to Take on the Beauty Industry” tells the story of protagonist Joe Wendell, known as Wendell, an emergency room nurse and widower raising a teenage daughter in Franklin, a largely working class town in the fictional US state of Columbia. One day his daughter announces she would like to have breast implants. The distressing news prompts Wendell into new, unforeseen directions as he learns all he can about implants and surgery, the “beauty culture” permeating society especially in his community, and the psychological development of teenagers. Though relieved to find out that as long as she is a minor she cannot legally obtain the surgery without his consent (and, no doubt, without his cash), Wendell starts to believe that greater protections for teen girls in Columbia are needed. In this effort he is guided by the confident figure of Anna Pinto, director of a community center in an East Franklin neighborhood with a vibrant Brazilian-American community where cosmetic surgery, especially for girls and young women, is something she perceives to be a particular problem and has some ideas about how to address. Teaching note available for faculty/instructors .
Madden, S.L. , 2015. The Merger of UCSF Medical Center and Stanford Health Services , Harvard Business Publishing: Harvard T.H. Chan School of Public Health case collection. Available from Harvard Business Publishing Abstract On November 15, 1996, Stanford’s Board of Trustees and the University of California (UC) Board of Regents voted to merge their two academic medical centers; on November 1, 1997, the merger became official. However, less than two years later, in October 1999, the merger came to an abrupt end. Was the merger an ill-conceived “snakebit venture” or a reasonable response to the environmental and economic pressures of the time that fell apart in its execution? Would the same ills have befallen Stanford and UCSF regardless of the merger?
Yatsko, P. & Koh, H. , 2017. Dr. Jim O'Connell, Managing Crisis, and Advocating for Boston's Chronically Homeless Community , Harvard Business Publishing: Harvard T.H. Chan School of Public Health case collection. Available from Harvard Business Publishing Abstract A deep sense of foreboding filled Dr. James O'Connell and his team at Boston Health Care for the Homeless (BHCHP) in October 2014. The Boston mayor's office had just condemned the 64-year-old bridge that provided the only passage to the island in Boston Harbor housing the city's largest homeless shelter. It did not have a long-term contingency shelter plan in place and the city's other shelters were full. With winter fast approaching, O'Connell, who had been serving Boston's homeless population for over a quarter century, feared some of the city's dispossessed would die on the streets from cold. BHCHP would be hard pressed to provide them the medical care they needed. To implement his solution-reopening the Boston Night Center-O'Connell had to overcome the disinterest of BHCHP's traditional allies in the homeless service provider community, who for a number of years had been channeling their energies away from sheltering toward permanent housing solutions. The Boston Night Center's reopening helped achieve an unprecedented feat for the City of Boston: Not a single homeless person died from the elements that winter, the harshest in the city's recorded history. O'Connell parlayed this achievement into city and state financial support for the Boston Night Center for the next several years. How did O'Connell work with stakeholders to accomplish his goal? What could he do to maintain financial support for the Boston Night Center and shelter programs in Boston more generally?
Chai, J., Gordon, R. & Johnson, P. , 2013. Malala Yousafzai: A Young Female Activist , Harvard University: Global Health Education and Learning Incubator. Access online Abstract This case traces the story of Malala Yousafzai who has advocated passionately for girls’ right to education. In October 2012, a militant group with ties to the Taliban shot 14-year-old Yousafzai in the head as she was riding the school bus home after a day of classes. Yousafzai recovered and became the youngest recipient of the Nobel Peace Prize in 2014. This case explores the social factors that made such an attack possible and why there continue to be such barriers to educational opportunities for girls. "Malala Yousafzai: A Young Female Activist" is a part of a case series on violence against women that illustrate the critical role for leadership through an examination of how factors within a society influence women’s health. Students analyze the situations described by considering the circumstances that placed each protagonist in vulnerable positions. Participants examined the commonalities and differences of these situations in an effort to understand the circumstances that affect women’s well-being. Additionally, using the cases as a framework, students analyzed the connections between collective outrage, reactive action, and leadership.
When Dr. Marwan started as director of Ramses Hospital in Cairo in 2008, charged by the Minister of Health with improving performance, he found the hospital had been neglected for decades. A Ministry of Health quality audit had recently given the hospital the worst score of the five hospitals designated as critical to the greater Cairo area.
Dr. Marwan vowed that Ramses Hospital would come in first in the next round of quality audits. Without improving its quality scores, the hospital would be unable to pass the accreditation process required for hospital participation in a new universal social health insurance scheme. In addition—and just as critically—Dr. Marwan needed to develop a longer-term strategy for obtaining the considerable additional resources required to upgrade the long-neglected facility.
"The foundation of Integrated Health Services is the relentless pursuit of value. Our fundamental purpose is to help IBM win in the marketplace through the health and productivity of our workforce." ---Martín Sepúlveda
Martín Sepúlveda, Vice President of Integrated Health Services at IBM, had played a central role in establishing IHS as a vital and ongoing contributor to the corporation's success. IBM's IHS organization, as it had come to be known in 2008, was a global team of approximately 250 occupational medicine, industrial hygiene, safety, health benefits and wellness professionals responsible for ensuring the health and well-being of IBM's over 400,000 employees worldwide. This case, set in 2011, highlights the many challenges and his team faced in developing strategies and approaches to creating a culture of health within IBM, and maintain its commitment to the well-being of every employee.
Wang, M. , 2017. Sugary Drink Legislation in Massachusetts , Harvard Business Publishing: Harvard T.H. Chan School of Public Health case collection. Available from Harvard Business Publishing Abstract In the fall of 2016, with the January 2017 deadline to file bills fast approaching, State Senator Jason Lewis was contemplating the details of a sugary drink legislative proposal in the Commonwealth of Massachusetts. Senator Lewis had a particular interest in legislative efforts to contain healthcare costs and prevent chronic disease through prevention and wellness approaches. He was particularly concerned about the rising levels of sugary drink consumption and associated conditions of obesity, diabetes, and dental caries, considering such drinks “a uniquely toxic food.” As an experienced legislator he knew he was facing a tough battle and wanted to take an approach that would give the bill the best chance of succeeding. Senator Lewis explained, “Massachusetts should be leading the legislative effort to reduce sugary drink consumption in the Northeast. Significant opposition from the beverage industry is expected, but we have a real chance of making progress at the local and state levels.”
Case Studies

“Case Studies in Healthcare: Success Stories and Lessons Learned”

Table of Contents
The healthcare industry is an ever-evolving field with innovations and improvements happening daily. As healthcare providers strive to deliver the best care possible, case studies have become a valuable resource for learning and growth. In this article, we will explore various case studies in healthcare, highlighting both success stories and the lessons learned along the way. By analyzing what works and why, we can gain insight into the practices that lead to triumphs in healthcare and potentially replicate these successes in our own organizations.
Case Studies in Healthcare: A Closer Look at Triumphs and Takeaways
Healthcare case studies provide a unique opportunity to dissect real-world scenarios, understand the decisions made, and measure the outcomes of those choices. One notable success story is the implementation of telemedicine in rural areas. By leveraging technology, healthcare providers have successfully expanded access to care for patients who would otherwise have to travel long distances for treatment. Lessons learned include the importance of investing in reliable technology and training staff to effectively use telemedicine platforms.
Another critical case study involves the management of electronic health records (EHRs). When a large hospital system transitioned to a new EHR system, they faced significant resistance from physicians who were accustomed to the old way of doing things. However, by involving physicians in the planning and implementation process, the hospital successfully integrated the new system, leading to improved efficiency and patient care. This case study highlights the value of stakeholder engagement and effective change management.
In the fight against infectious diseases, case studies have shown the significance of swift and coordinated responses. An example of this is the containment of Ebola in West Africa. Through international collaboration and the rapid deployment of healthcare resources, the spread of the virus was effectively limited. This case study underscores the importance of preparedness, communication, and teamwork in tackling healthcare crises.
Success Stories in Healthcare: Analyzing What Works and Why
Understanding why certain strategies succeed is crucial for replicating positive results in the healthcare industry. For instance, one hospital’s initiative to reduce patient readmissions focused on comprehensive discharge planning and follow-up care. By ensuring patients had clear instructions and support after leaving the hospital, readmission rates dropped significantly. This case study emphasizes the role of thorough patient education and post-discharge care in improving outcomes.
In the realm of preventive care, a primary care clinic introduced a program to increase vaccination rates among its patient population. By actively reaching out to patients due for immunizations and offering flexible scheduling options, the clinic saw a dramatic increase in vaccination rates. The takeaway from this case study is the impact of proactive patient engagement and removing barriers to care.
Lastly, a healthcare organization’s embrace of continuous quality improvement (CQI) led to enhanced patient safety and satisfaction. By fostering a culture of open communication and ongoing learning, the organization identified areas for improvement and systematically implemented changes. This case study demonstrates the power of a commitment to CQI as a driver for excellence in healthcare.
The healthcare industry is rich with case studies that provide valuable insights and lessons learned. By analyzing and understanding these success stories, healthcare providers can apply similar strategies to achieve positive outcomes in their own organizations. Whether it’s through technology, stakeholder engagement, or quality improvement initiatives, these case studies offer a blueprint for triumph and provide a roadmap for future success in the ever-changing landscape of healthcare.
Why are case studies valuable in the healthcare industry, and how do they provide insights into successful decision-making and problem-solving within healthcare organizations?
Case studies are valuable as they offer real-world examples of challenges and solutions in healthcare. They provide insights into successful decision-making, problem-solving, and strategies that can be applied by healthcare professionals and organizations facing similar scenarios.
How does the article select and present case studies, and what criteria are considered to ensure the relevance and applicability of the showcased success stories to a diverse audience?
The article discusses the criteria for selecting case studies, such as their impact on healthcare outcomes, innovation, or overcoming significant challenges. It highlights the diversity of cases to ensure relevance to a broad audience, considering different healthcare settings, specialties, and contexts.
Can you provide examples of healthcare case studies featured in the article, and how do these stories illustrate successful decision-making or lessons learned that can benefit readers in the healthcare field?
Certainly! Examples may include cases where innovative technologies improved patient outcomes, or instances where strategic decisions enhanced operational efficiency. The article presents these stories to illustrate valuable lessons learned and best practices that readers can apply in their own healthcare settings.
In what ways do case studies contribute to professional development and learning opportunities for healthcare professionals, and how can organizations leverage these stories for continuous improvement and staff training?
The article explores how case studies offer learning opportunities, allowing healthcare professionals to gain insights from others’ experiences. Organizations can leverage these stories for staff training, fostering a culture of continuous improvement and encouraging employees to apply lessons learned to their daily practices.
For healthcare leaders seeking to implement successful strategies within their organizations, what recommendations and actionable insights does the article provide based on the analysis of the showcased case studies?
The article offers recommendations based on the case studies, such as the importance of collaboration, data-driven decision-making, and embracing innovation. It provides actionable insights that healthcare leaders can use to inform their decision-making processes and drive positive outcomes within their organizations.
Leave a comment Cancel reply
You must be logged in to post a comment.
+1 (800) 782 1768
Health Case Studies
(29 reviews)
Glynda Rees, British Columbia Institute of Technology
Rob Kruger, British Columbia Institute of Technology
Janet Morrison, British Columbia Institute of Technology
Copyright Year: 2017
Publisher: BCcampus
Language: English
Formats Available
Conditions of use.
Learn more about reviews.
Reviewed by Jessica Sellars, Medical assistant office instructor, Blue Mountain Community College on 10/11/23
This is a book of compiled and very well organized patient case studies. The author has broken it up by disease patient was experiencing and even the healthcare roles that took place in this patients care. There is a well thought out direction and... read more
Comprehensiveness rating: 5 see less
This is a book of compiled and very well organized patient case studies. The author has broken it up by disease patient was experiencing and even the healthcare roles that took place in this patients care. There is a well thought out direction and plan. There is an appendix to refer to as well if you are needing to find something specific quickly. I have been looking for something like this to help my students have a base to do their project on. This is the most comprehensive version I have found on the subject.
Content Accuracy rating: 5
This is a book compiled of medical case studies. It is very accurate and can be used to learn from great care and mistakes.
Relevance/Longevity rating: 5
This material is very relevant in this context. It also has plenty of individual case studies to utilize in many ways in all sorts of medical courses. This is a very useful textbook and it will continue to be useful for a very long time as you can still learn from each study even if medicine changes through out the years.
Clarity rating: 5
The author put a lot of thought into the ease of accessibility and reading level of the target audience. There is even a "how to use this resource" section which could be extremely useful to students.
Consistency rating: 5
The text follows a very consistent format throughout the book.
Modularity rating: 5
Each case study is individual broken up and in a group of similar case studies. This makes it extremely easy to utilize.
Organization/Structure/Flow rating: 5
The book is very organized and the appendix is through. It flows seamlessly through each case study.
Interface rating: 5
I had no issues navigating this book, It was clearly labeled and very easy to move around in.
Grammatical Errors rating: 5
I did not catch any grammar errors as I was going through the book
Cultural Relevance rating: 5
This is a challenging question for any medical textbook. It is very culturally relevant to those in medical or medical office degrees.
I have been looking for something like this for years. I am so happy to have finally found it.
Reviewed by Cindy Sun, Assistant Professor, Marshall University on 1/7/23
Interestingly, this is not a case of ‘you get what you pay for’. Instead, not only are the case studies organized in a fashion for ease of use through a detailed table of contents, the authors have included more support for both faculty and... read more
Interestingly, this is not a case of ‘you get what you pay for’. Instead, not only are the case studies organized in a fashion for ease of use through a detailed table of contents, the authors have included more support for both faculty and students. For faculty, the introduction section titled ‘How to use this resource’ and individual notes to educators before each case study contain application tips. An appendix overview lists key elements as issues / concepts, scenario context, and healthcare roles for each case study. For students, learning objectives are presented at the beginning of each case study to provide a framework of expectations.
The content is presented accurately and realistic.
The case studies read similar to ‘A Day In the Life of…’ with detailed intraprofessional communications similar to what would be overheard in patient care areas. The authors present not only the view of the patient care nurse, but also weave interprofessional vantage points through each case study by including patient interaction with individual professionals such as radiology, physician, etc.
In addition to objective assessment findings, the authors integrate standard orders for each diagnosis including medications, treatments, and tests allowing the student to incorporate pathophysiology components to their assessments.
Each case study is arranged in the same framework for consistency and ease of use.
This compilation of eight healthcare case studies focusing on new onset and exacerbation of prevalent diagnoses, such as heart failure, deep vein thrombosis, cancer, and chronic obstructive pulmonary disease advancing to pneumonia.
Each case study has a photo of the ‘patient’. Simple as this may seem, it gives an immediate mental image for the student to focus.
Interface rating: 4
As noted by previous reviewers, most of the links do not connect active web pages. This may be due to the multiple options for accessing this resource (pdf download, pdf electronic, web view, etc.).
Grammatical Errors rating: 4
A minor weakness that faculty will probably need to address prior to use is regarding specific term usages differences between Commonwealth countries and United States, such as lung sound descriptors as ‘quiet’ in place of ‘diminished’ and ‘puffers’ in place of ‘inhalers’.
The authors have provided a multicultural, multigenerational approach in selection of patient characteristics representing a snapshot of today’s patient population. Additionally, one case study focusing on heart failure is about a middle-aged adult, contrasting to the average aged patient the students would normally see during clinical rotations. This option provides opportunities for students to expand their knowledge on risk factors extending beyond age.
This resource is applicable to nursing students learning to care for patients with the specific disease processes presented in each case study or for the leadership students focusing on intraprofessional communication. Educators can assign as a supplement to clinical experiences or as an in-class application of knowledge.
Reviewed by Stephanie Sideras, Assistant Professor, University of Portland on 8/15/22
The eight case studies included in this text addressed high frequency health alterations that all nurses need to be able to manage competently. While diabetes was not highlighted directly, it was included as a potential comorbidity. The five... read more
The eight case studies included in this text addressed high frequency health alterations that all nurses need to be able to manage competently. While diabetes was not highlighted directly, it was included as a potential comorbidity. The five overarching learning objectives pulled from the Institute of Medicine core competencies will clearly resonate with any faculty familiar with Quality and Safety Education for Nurses curriculum.
The presentation of symptoms, treatments and management of the health alterations was accurate. Dialogue between the the interprofessional team was realistic. At times the formatting of lab results was confusing as they reflected reference ranges specific to the Canadian healthcare system but these occurrences were minimal and could be easily adapted.
The focus for learning from these case studies was communication - patient centered communication and interprofessional team communication. Specific details, such as drug dosing, was minimized, which increases longevity and allows for easy individualization of the case data.
While some vocabulary was specific to the Canadian healthcare system, overall the narrative was extremely engaging and easy to follow. Subjective case data from patient or provider were formatted in italics and identified as 'thoughts'. Objective and behavioral case data were smoothly integrated into the narrative.
The consistency of formatting across the eight cases was remarkable. Specific learning objectives are identified for each case and these remain consistent across the range of cases, varying only in the focus for the goals for each different health alterations. Each case begins with presentation of essential patient background and the progress across the trajectory of illness as the patient moves from location to location encountering different healthcare professionals. Many of the characters (the triage nurse in the Emergency Department, the phlebotomist) are consistent across the case situations. These consistencies facilitate both application of a variety of teaching methods and student engagement with the situated learning approach.
Case data is presented by location and begins with the patient's first encounter with the healthcare system. This allows for an examination of how specific trajectories of illness are manifested and how care management needs to be prioritized at different stages. This approach supports discussions of care transitions and the complexity of the associated interprofessional communication.
The text is well organized. The case that has two levels of complexity is clearly identified
The internal links between the table of contents and case specific locations work consistently. In the EPUB and the Digital PDF the external hyperlinks are inconsistently valid.
The grammatical errors were minimal and did not detract from readability
Cultural diversity is present across the cases in factors including race, ethnicity, socioeconomic status, family dynamics and sexual orientation.
The level of detail included in these cases supports a teaching approach to address all three spectrums of learning - knowledge, skills and attitudes - necessary for the development of competent practice. I also appreciate the inclusion of specific assessment instruments that would facilitate a discussion of evidence based practice. I will enjoy using these case to promote clinical reasoning discussions of data that is noticed and interpreted with the resulting prioritizes that are set followed by reflections that result from learner choices.
Reviewed by Chris Roman, Associate Professor, Butler University on 5/19/22
It would be extremely difficult for a book of clinical cases to comprehensively cover all of medicine, and this text does not try. Rather, it provides cases related to common medical problems and introduces them in a way that allows for various... read more
Comprehensiveness rating: 4 see less
It would be extremely difficult for a book of clinical cases to comprehensively cover all of medicine, and this text does not try. Rather, it provides cases related to common medical problems and introduces them in a way that allows for various learning strategies to be employed to leverage the cases for deeper student learning and application.
The narrative form of the cases is less subject to issues of accuracy than a more content-based book would be. That said, the cases are realistic and reasonable, avoiding being too mundane or too extreme.
These cases are narrative and do not include many specific mentions of drugs, dosages, or other aspects of clinical care that may grow/evolve as guidelines change. For this reason, the cases should be “evergreen” and can be modified to suit different types of learners.
Clarity rating: 4
The text is written in very accessible language and avoids heavy use of technical language. Depending on the level of learner, this might even be too simplistic and omit some details that would be needed for physicians, pharmacists, and others to make nuanced care decisions.
The format is very consistent with clear labeling at transition points.
The authors point out in the introductory materials that this text is designed to be used in a modular fashion. Further, they have built in opportunities to customize each cases, such as giving dates of birth at “19xx” to allow for adjustments based on instructional objectives, etc.
The organization is very easy to follow.
I did not identify any issues in navigating the text.
The text contains no grammatical errors, though the language is a little stiff/unrealistic in some cases.
Cases involve patients and members of the care team that are of varying ages, genders, and racial/ethnic backgrounds
Reviewed by Trina Larery, Assistant Professor, Pittsburg State University on 4/5/22
The book covers common scenarios, providing allied health students insight into common health issues. The information in the book is thorough and easily modified if needed to include other scenarios not listed. The material was easy to understand... read more
The book covers common scenarios, providing allied health students insight into common health issues. The information in the book is thorough and easily modified if needed to include other scenarios not listed. The material was easy to understand and apply to the classroom. The E-reader format included hyperlinks that bring the students to subsequent clinical studies.
Content Accuracy rating: 4
The treatments were explained and rationales were given, which can be very helpful to facilitate effective learning for a nursing student or novice nurse. The case studies were accurate in explanation. The DVT case study incorrectly identifies the location of the clot in the popliteal artery instead of in the vein.
The content is relevant to a variety of different types of health care providers and due to the general nature of the cases, will remain relevant over time. Updates should be made annually to the hyperlinks and to assure current standard of practice is still being met.
Clear, simple and easy to read.
Consistent with healthcare terminology and framework throughout all eight case studies.
The text is modular. Cases can be used individually within a unit on the given disease process or relevant sections of a case could be used to illustrate a specific point providing great flexibility. The appendix is helpful in locating content specific to a certain diagnosis or a certain type of health care provider.
The book is well organized, presenting in a logical clear fashion. The appendix allows the student to move about the case study without difficulty.
The interface is easy and simple to navigate. Some links to external sources might need to be updated regularly since those links are subject to change based on current guidelines. A few hyperlinks had "page not found".
Few grammatical errors were noted in text.
The case studies include people of different ethnicities, socioeconomic status, ages, and genders to make this a very useful book.
I enjoyed reading the text. It was interesting and relevant to today's nursing student. There are roughly 25 broken online links or "pages not found", care needs to be taken to update at least annually and assure links are valid and utilizing the most up to date information.
Reviewed by Benjamin Silverberg, Associate Professor/Clinician, West Virginia University on 3/24/22
The appendix reviews the "key roles" and medical venues found in all 8 cases, but is fairly spartan on medical content. The table of contents at the beginning only lists the cases and locations of care. It can be a little tricky to figure out what... read more
Comprehensiveness rating: 3 see less
The appendix reviews the "key roles" and medical venues found in all 8 cases, but is fairly spartan on medical content. The table of contents at the beginning only lists the cases and locations of care. It can be a little tricky to figure out what is going on where, especially since each case is largely conversation-based. Since this presents 8 cases (really 7 with one being expanded upon), there are many medical topics (and venues) that are not included. It's impossible to include every kind of situation, but I'd love to see inclusion of sexual health, renal pathology, substance abuse, etc.
Though there are differences in how care can be delivered based on personal style, changing guidelines, available supplies, etc, the medical accuracy seems to be high. I did not detect bias or industry influence.
Relevance/Longevity rating: 4
Medications are generally listed as generics, with at least current dosing recommendations. The text gives a picture of what care looks like currently, but will be a little challenging to update based on new guidelines (ie, it can be hard to find the exact page in which a medication is dosed/prescribed). Even if the text were to be a little out of date, an instructor can use that to point out what has changed (and why).
Clear text, usually with definitions of medical slang or higher-tier vocabulary. Minimal jargon and there are instances where the "characters" are sorting out the meaning as well, making it accessible for new learners, too.
Overall, the style is consistent between cases - largely broken up into scenes and driven by conversation rather than descriptions of what is happening.
There are 8 (well, again, 7) cases which can be reviewed in any order. Case #2 builds upon #1, which is intentional and a good idea, though personally I would have preferred one case to have different possible outcomes or even a recurrence of illness. Each scene within a case is reasonably short.
Organization/Structure/Flow rating: 4
These cases are modular and don't really build on concepts throughout. As previously stated, case #2 builds upon #1, but beyond that, there is no progression. (To be sure, the authors suggest using case #1 for newer learners and #2 for more advanced ones.) The text would benefit from thematic grouping, a longer introduction and debriefing for each case (there are learning objectives but no real context in medical education nor questions to reflect on what was just read), and progressively-increasing difficulty in medical complexity, ethics, etc.
I used the PDF version and had no interface issues. There are minimal photographs and charts. Some words are marked in blue but those did not seem to be hyperlinked anywhere.
No noticeable errors in grammar, spelling, or formatting were noted.
I appreciate that some diversity of age and ethnicity were offered, but this could be improved. There were Canadian Indian and First Nations patients, for example, as well as other characters with implied diversity, but there didn't seem to be any mention of gender diverse or non-heterosexual people, or disabilities. The cases tried to paint family scenes (the first patient's dog was fairly prominently mentioned) to humanize them. Including more cases would allow for more opportunities to include sex/gender minorities, (hidden) disabilities, etc.
The text (originally from 2017) could use an update. It could be used in conjunction with other Open Texts, as a compliment to other coursework, or purely by itself. The focus is meant to be on improving communication, but there are only 3 short pages at the beginning of the text considering those issues (which are really just learning objectives). In addition to adding more cases and further diversity, I personally would love to see more discussion before and after the case to guide readers (and/or instructors). I also wonder if some of the ambiguity could be improved by suggesting possible health outcomes - this kind of counterfactual comparison isn't possible in real life and could be really interesting in a text. Addition of comprehension/discussion questions would also be worthwhile.
Reviewed by Danielle Peterson, Assistant Professor, University of Saint Francis on 12/31/21
This text provides readers with 8 case studies which include both chronic and acute healthcare issues. Although not comprehensive in regard to types of healthcare conditions, it provides a thorough look at the communication between healthcare... read more
This text provides readers with 8 case studies which include both chronic and acute healthcare issues. Although not comprehensive in regard to types of healthcare conditions, it provides a thorough look at the communication between healthcare workers in acute hospital settings. The cases are primarily set in the inpatient hospital setting, so the bulk of the clinical information is basic emergency care and inpatient protocol: vitals, breathing, medication management, etc. The text provides a table of contents at opening of the text and a handy appendix at the conclusion of the text that outlines each case’s issue(s), scenario, and healthcare roles. No index or glossary present.
Although easy to update, it should be noted that the cases are taking place in a Canadian healthcare system. Terms may be unfamiliar to some students including “province,” “operating theatre,” “physio/physiotherapy,” and “porter.” Units of measurement used include Celsius and meters. Also, the issue of managed care, health insurance coverage, and length of stay is missing for American students. These are primary issues that dictate much of the healthcare system in the US and a primary job function of social workers, nurse case managers, and medical professionals in general. However, instructors that wish to add this to the case studies could do so easily.
The focus of this text is on healthcare communication which makes it less likely to become obsolete. Much of the clinical information is stable healthcare practice that has been standard of care for quite some time. Nevertheless, given the nature of text, updates would be easy to make. Hyperlinks should be updated to the most relevant and trustworthy sources and checked frequently for effectiveness.
The spacing that was used to note change of speaker made for ease of reading. Although unembellished and plain, I expect students to find this format easy to digest and interesting, especially since the script is appropriately balanced with ‘human’ qualities like the current TV shows and songs, the use of humor, and nonverbal cues.
A welcome characteristic of this text is its consistency. Each case is presented in a similar fashion and the roles of the healthcare team are ‘played’ by the same character in each of the scenarios. This allows students to see how healthcare providers prioritize cases and juggle the needs of multiple patients at once. Across scenarios, there was inconsistency in when clinical terms were hyperlinked.
The text is easily divisible into smaller reading sections. However, since the nature of the text is script-narrative format, if significant reorganization occurs, one will need to make sure that the communication of the script still makes sense.
The text is straightforward and presented in a consistent fashion: learning objectives, case history, a script of what happened before the patient enters the healthcare setting, and a script of what happens once the patient arrives at the healthcare setting. The authors use the term, “ideal interactions,” and I would agree that these cases are in large part, ‘best case scenarios.’ Due to this, the case studies are well organized, clear, logical, and predictable. However, depending on the level of student, instructors may want to introduce complications that are typical in the hospital setting.
The interface is pleasing and straightforward. With exception to the case summary and learning objectives, the cases are in narrative, script format. Each case study supplies a photo of the ‘patient’ and one of the case studies includes a link to a 3-minute video that introduces the reader to the patient/case. One of the highlights of this text is the use of hyperlinks to various clinical practices (ABG, vital signs, transfer of patient). Unfortunately, a majority of the links are broken. However, since this is an open text, instructors can update the links to their preference.
Although not free from grammatical errors, those that were noticed were minimal and did not detract from reading.
Cultural Relevance rating: 4
Cultural diversity is visible throughout the patients used in the case studies and includes factors such as age, race, socioeconomic status, family dynamics, and sexual orientation. A moderate level of diversity is noted in the healthcare team with some stereotypes: social workers being female, doctors primarily male.
As a social work instructor, I was grateful to find a text that incorporates this important healthcare role. I would have liked to have seen more content related to advance directives, mediating decision making between the patient and care team, emotional and practical support related to initial diagnosis and discharge planning, and provision of support to colleagues, all typical roles of a medical social worker. I also found it interesting that even though social work was included in multiple scenarios, the role was only introduced on the learning objectives page for the oncology case.
Reviewed by Crystal Wynn, Associate Professor, Virginia State University on 7/21/21
The text covers a variety of chronic diseases within the cases; however, not all of the common disease states were included within the text. More chronic diseases need to be included such as diabetes, cancer, and renal failure. Not all allied... read more
The text covers a variety of chronic diseases within the cases; however, not all of the common disease states were included within the text. More chronic diseases need to be included such as diabetes, cancer, and renal failure. Not all allied health care team members are represented within the case study. Key terms appear throughout the case study textbook and readers are able to click on a hyperlink which directs them to the definition and an explanation of the key term.
Content is accurate, error-free and unbiased.
The content is up-to-date, but not in a way that will quickly make the text obsolete within a short period of time. The text is written and/or arranged in such a way that necessary updates will be relatively easy and straightforward to implement.
The text is written in lucid, accessible prose, and provides adequate context for any jargon/technical terminology used
The text is internally consistent in terms of terminology and framework.
The text is easily and readily divisible into smaller reading sections that can be assigned at different points within the course. Each case can be divided into a chronic disease state unit, which will allow the reader to focus on one section at a time.
Organization/Structure/Flow rating: 3
The topics in the text are presented in a logical manner. Each case provides an excessive amount of language that provides a description of the case. The cases in this text reads more like a novel versus a clinical textbook. The learning objectives listed within each case should be in the form of questions or activities that could be provided as resources for instructors and teachers.
Interface rating: 3
There are several hyperlinks embedded within the textbook that are not functional.
The text contains no grammatical errors.
Cultural Relevance rating: 3
The text is not culturally insensitive or offensive in any way. More examples of cultural inclusiveness is needed throughout the textbook. The cases should be indicative of individuals from a variety of races and ethnicities.
Reviewed by Rebecca Hillary, Biology Instructor, Portland Community College on 6/15/21
This textbook consists of a collection of clinical case studies that can be applicable to a wide range of learning environments from supplementing an undergraduate Anatomy and Physiology Course, to including as part of a Medical or other health... read more
This textbook consists of a collection of clinical case studies that can be applicable to a wide range of learning environments from supplementing an undergraduate Anatomy and Physiology Course, to including as part of a Medical or other health care program. I read the textbook in E-reader format and this includes hyperlinks that bring the students to subsequent clinical study if the book is being used in a clinical classroom. This book is significantly more comprehensive in its approach from other case studies I have read because it provides a bird’s eye view of the many clinicians, technicians, and hospital staff working with one patient. The book also provides real time measurements for patients that change as they travel throughout the hospital until time of discharge.
Each case gave an accurate sense of the chaos that would be present in an emergency situation and show how the conditions affect the practitioners as well as the patients. The reader gets an accurate big picture--a feel for each practitioner’s point of view as well as the point of view of the patient and the patient’s family as the clock ticks down and the patients are subjected to a number of procedures. The clinical information contained in this textbook is all in hyperlinks containing references to clinical skills open text sources or medical websites. I did find one broken link on an external medical resource.
The diseases presented are relevant and will remain so. Some of the links are directly related to the Canadian Medical system so they may not be applicable to those living in other regions. Clinical links may change over time but the text itself will remain relevant.
Each case study clearly presents clinical data as is it recorded in real time.
Each case study provides the point of view of several practitioners and the patient over several days. While each of the case studies covers different pathology they all follow this same format, several points of view and data points, over a number of days.
The case studies are divided by days and this was easy to navigate as a reader. It would be easy to assign one case study per body system in an Anatomy and Physiology course, or to divide them up into small segments for small in class teaching moments.
The topics are presented in an organized way showing clinical data over time and each case presents a large number of view points. For example, in the first case study, the patient is experiencing difficulty breathing. We follow her through several days from her entrance to the emergency room. We meet her X Ray Technicians, Doctor, Nurses, Medical Assistant, Porter, Physiotherapist, Respiratory therapist, and the Lab Technicians running her tests during her stay. Each practitioner paints the overall clinical picture to the reader.
I found the text easy to navigate. There were not any figures included in the text, only clinical data organized in charts. The figures were all accessible via hyperlink. Some figures within the textbook illustrating patient scans could have been helpful but I did not have trouble navigating the links to visualize the scans.
I did not see any grammatical errors in the text.
The patients in the text are a variety of ages and have a variety of family arrangements but there is not much diversity among the patients. Our seven patients in the eight case studies are mostly white and all cis gendered.
Some of the case studies, for example the heart failure study, show clinical data before and after drug treatments so the students can get a feel for mechanism in physiological action. I also liked that the case studies included diet and lifestyle advice for the patients rather than solely emphasizing these pharmacological interventions. Overall, I enjoyed reading through these case studies and I plan to utilize them in my Anatomy and Physiology courses.
Reviewed by Richard Tarpey, Assistant Professor, Middle Tennessee State University on 5/11/21
As a case study book, there is no index or glossary. However, medical and technical terms provide a useful link to definitions and explanations that will prove useful to students unfamiliar with the terms. The information provided is appropriate... read more
As a case study book, there is no index or glossary. However, medical and technical terms provide a useful link to definitions and explanations that will prove useful to students unfamiliar with the terms. The information provided is appropriate for entry-level health care students. The book includes important health problems, but I would like to see coverage of at least one more chronic/lifestyle issue such as diabetes. The book covers adult issues only.
Content is accurate without bias
The content of the book is relevant and up-to-date. It addresses conditions that are prevalent in today's population among adults. There are no pediatric cases, but this does not significantly detract from the usefulness of the text. The format of the book lends to easy updating of data or information.
The book is written with clarity and is easy to read. The writing style is accessible and technical terminology is explained with links to more information.
Consistency is present. Lack of consistency is typically a problem with case study texts, but this book is consistent with presentation, format, and terminology throughout each of the eight cases.
The book has high modularity. Each of the case studies can be used independently from the others providing flexibility. Additionally, each case study can be partitioned for specific learning objectives based on the learning objectives of the course or module.
The book is well organized, presenting students conceptually with differing patient flow patterns through a hospital. The patient information provided at the beginning of each case is a wonderful mechanism for providing personal context for the students as they consider the issues. Many case studies focus on the problem and the organization without students getting a patient's perspective. The patient perspective is well represented in these cases.
The navigation through the cases is good. There are some terminology and procedure hyperlinks within the cases that do not work when accessed. This is troubling if you intend to use the text for entry-level health care students since many of these links are critical for a full understanding of the case.
There are some non-US variants of spelling and a few grammatical errors, but these do not detract from the content of the messages of each case.
The book is inclusive of differing backgrounds and perspectives. No insensitive or offensive references were found.
I like this text for its application flexibility. The book is useful for non-clinical healthcare management students to introduce various healthcare-related concepts and terminology. The content is also helpful for the identification of healthcare administration managerial issues for students to consider. The book has many applications.
Reviewed by Paula Baldwin, Associate Professor/Communication Studies, Western Oregon University on 5/10/21
The different case studies fall on a range, from crisis care to chronic illness care. read more
The different case studies fall on a range, from crisis care to chronic illness care.
The contents seems to be written as they occurred to represent the most complete picture of each medical event's occurence.
These case studies are from the Canadian medical system, but that does not interfere with it's applicability.
It is written for a medical audience, so the terminology is mostly formal and technical.
Some cases are shorter than others and some go in more depth, but it is not problematic.
The eight separate case studies is the perfect size for a class in the quarter system. You could combine this with other texts, videos or learning modalities, or use it alone.
As this is a case studies book, there is not a need for a logical progression in presentation of topics.
No problems in terms of interface.
I have not seen any grammatical errors.
I did not see anything that was culturally insensitive.
I used this in a Health Communication class and it has been extraordinarily successful. My studies are analyzing the messaging for the good, the bad, and the questionable. The case studies are widely varied and it gives the class insights into hospital experiences, both front and back stage, that they would not normally be able to examine. I believe that because it is based real-life medical incidents, my students are finding the material highly engaging.
Reviewed by Marlena Isaac, Instructor, Aiken Technical College on 4/23/21
This text is great to walk through patient care with entry level healthcare students. The students are able to take in the information, digest it, then provide suggestions to how they would facilitate patient healing. Then when they are faced with... read more
This text is great to walk through patient care with entry level healthcare students. The students are able to take in the information, digest it, then provide suggestions to how they would facilitate patient healing. Then when they are faced with a situation in clinical they are not surprised and now how to move through it effectively.
The case studies provided accurate information that relates to the named disease.
It is relevant to health care studies and the development of critical thinking.
Cases are straightforward with great clinical information.
Clinical information is provided concisely.
Appropriate for clinical case study.
Presented to facilitate information gathering.
Takes a while to navigate in the browser.
Cultural Relevance rating: 1
Text lacks adequate representation of minorities.
Reviewed by Kim Garcia, Lecturer III, University of Texas Rio Grande Valley on 11/16/20
The book has 8 case studies, so obviously does not cover the whole of medicine, but the cases provided are descriptive and well developed. Cases are presented at different levels of difficulty, making the cases appropriate for students at... read more
The book has 8 case studies, so obviously does not cover the whole of medicine, but the cases provided are descriptive and well developed. Cases are presented at different levels of difficulty, making the cases appropriate for students at different levels of clinical knowledge. The human element of both patient and health care provider is well captured. The cases are presented with a focus on interprofessional interaction and collaboration, more so than teaching medical content.
Content is accurate and un-biased. No errors noted. Most diagnostic and treatment information is general so it will remain relevant over time. The content of these cases is more appropriate for teaching interprofessional collaboration and less so for teaching the medical care for each diagnosis.
The content is relevant to a variety of different types of health care providers (nurses, radiologic technicians, medical laboratory personnel, etc) and due to the general nature of the cases, will remain relevant over time.
Easy to read. Clear headings are provided for sections of each case study and these section headings clearly tell when time has passed or setting has changed. Enough description is provided to help set the scene for each part of the case. Much of the text is written in the form of dialogue involving patient, family and health care providers, making it easy to adapt for role play. Medical jargon is limited and links for medical terms are provided to other resources that expound on medical terms used.
The text is consistent in structure of each case. Learning objectives are provided. Cases generally start with the patient at home and move with the patient through admission, testing and treatment, using a variety of healthcare services and encountering a variety of personnel.
The text is modular. Cases could be used individually within a unit on the given disease process or relevant sections of a case could be used to illustrate a specific point. The appendix is helpful in locating content specific to a certain diagnosis or a certain type of health care provider.
Each case follows a patient in a logical, chronologic fashion. A clear table of contents and appendix are provided which allows the user to quickly locate desired content. It would be helpful if the items in the table of contents and appendix were linked to the corresponding section of the text.
The hyperlinks to content outside this book work, however using the back arrow on your browser returns you to the front page of the book instead of to the point at which you left the text. I would prefer it if the hyperlinks opened in a new window or tab so closing that window or tab would leave you back where you left the text.
No grammatical errors were noted.
The text is culturally inclusive and appropriate. Characters, both patients and care givers are of a variety of races, ethnicities, ages and backgrounds.
I enjoyed reading the cases and reviewing this text. I can think of several ways in which I will use this content.
Reviewed by Raihan Khan, Instructor/Assistant Professor, James Madison University on 11/3/20
The book contains several important health issues, however still missing some chronic health issues that the students should learn before they join the workforce, such as diabetes-related health issues suffered by the patients. read more
The book contains several important health issues, however still missing some chronic health issues that the students should learn before they join the workforce, such as diabetes-related health issues suffered by the patients.
The health information contained in the textbook is mostly accurate.
I think the book is written focusing on the current culture and health issues faced by the patients. To keep the book relevant in the future, the contexts especially the culture/lifestyle/health care modalities, etc. would need to be updated regularly.
The language is pretty simple, clear, and easy to read.
There is no complaint about consistency. One of the main issues of writing a book, consistency was well managed by the authors.
The book is easy to explore based on how easy the setup is. Students can browse to the specific section that they want to read without much hassle of finding the correct information.
The organization is simple but effective. The authors organized the book based on what can happen in a patient's life and what possible scenarios students should learn about the disease. From that perspective, the book does a good job.
The interface is easy and simple to navigate. Some links to external sources might need to be updated regularly since those links are subject to change that is beyond the author's control. It's frustrating for the reader when the external link shows no information.
The book is free of any major language and grammatical errors.
The book might do a little better in cultural competency. e.g. Last name Singh is mainly for Sikh people. In the text Harj and Priya Singh are Muslim. the authors can consult colleagues who are more familiar with those cultures and revise some cultural aspects of the cases mentioned in the book.
The book is a nice addition to the open textbook world. Hope to see more health issues covered by the book.
Reviewed by Ryan Sheryl, Assistant Professor, California State University, Dominguez Hills on 7/16/20
This text contains 8 medical case studies that reflect best practices at the time of publication. The text identifies 5 overarching learning objectives: interprofessional collaboration, client centered care, evidence-based practice, quality... read more
This text contains 8 medical case studies that reflect best practices at the time of publication. The text identifies 5 overarching learning objectives: interprofessional collaboration, client centered care, evidence-based practice, quality improvement, and informatics. While the case studies do not cover all medical conditions or bodily systems, the book is thorough in conveying details of various patients and medical team members in a hospital environment. Rather than an index or glossary at the end of the text, it contains links to outside websites for more information on medical tests and terms referenced in the cases.
The content provided is reflective of best practices in patient care, interdisciplinary collaboration, and communication at the time of publication. It is specifically accurate for the context of hospitals in Canada. The links provided throughout the text have the potential to supplement with up-to-date descriptions and definitions, however, many of them are broken (see notes in Interface section).
The content of the case studies reflects the increasingly complex landscape of healthcare, including a variety of conditions, ages, and personal situations of the clients and care providers. The text will require frequent updating due to the rapidly changing landscape of society and best practices in client care. For example, a future version may include inclusive practices with transgender clients, or address ways medical racism implicitly impacts client care (see notes in Cultural Relevance section).
The text is written clearly and presents thorough, realistic details about working and being treated in an acute hospital context.
The text is very straightforward. It is consistent in its structure and flow. It uses consistent terminology and follows a structured framework throughout.
Being a series of 8 separate case studies, this text is easily and readily divisible into smaller sections. The text was designed to be taken apart and used piece by piece in order to serve various learning contexts. The parts of each case study can also be used independently of each other to facilitate problem solving.
The topics in the case studies are presented clearly. The structure of each of the case studies proceeds in a similar fashion. All of the cases are set within the same hospital so the hospital personnel and service providers reappear across the cases, giving a textured portrayal of the experiences of the various service providers. The cases can be used individually, or one service provider can be studied across the various studies.
The text is very straightforward, without complex charts or images that could become distorted. Many of the embedded links are broken and require updating. The links that do work are a very useful way to define and expand upon medical terms used in the case studies.
Grammatical errors are minimal and do not distract from the flow of the text. In one instance the last name Singh is spelled Sing, and one patient named Fred in the text is referred to as Frank in the appendix.
The cases all show examples of health care personnel providing compassionate, client-centered care, and there is no overt discrimination portrayed. Two of the clients are in same-sex marriages and these are shown positively. It is notable, however, that the two cases presenting people of color contain more negative characteristics than the other six cases portraying Caucasian people. The people of color are the only two examples of clients who smoke regularly. In addition, the Indian client drinks and is overweight, while the First Nations client is the only one in the text to have a terminal diagnosis. The Indian client is identified as being Punjabi and attending a mosque, although there are only 2% Muslims in the Punjab province of India. Also, the last name Singh generally indicates a person who is a Hindu or Sikh, not Muslim.
Reviewed by Monica LeJeune, RN Instructor, LSUE on 4/24/20
Has comprehensive unfolding case studies that guide the reader to recognize and manage the scenario presented. Assists in critical thinking process. read more
Has comprehensive unfolding case studies that guide the reader to recognize and manage the scenario presented. Assists in critical thinking process.
Accurately presents health scenarios with real life assessment techniques and patient outcomes.
Relevant to nursing practice.
Clearly written and easily understood.
Consistent with healthcare terminology and framework
Has a good reading flow.
Topics presented in logical fashion
Easy to read.
No grammatical errors noted.
Text is not culturally insensitive or offensive.
Good book to have to teach nursing students.
Reviewed by april jarrell, associate professor, J. Sargeant Reynolds Community College on 1/7/20
The text is a great case study tool that is appropriate for nursing school instructors to use in aiding students to learn the nursing process. read more
The text is a great case study tool that is appropriate for nursing school instructors to use in aiding students to learn the nursing process.
The content is accurate and evidence based. There is no bias noted
The content in the text is relevant, up to date for nursing students. It will be easy to update content as needed because the framework allows for addition to the content.
The text is clear and easy to understand.
Framework and terminology is consistent throughout the text; the case study is a continual and takes the student on a journey with the patient. Great for learning!
The case studies can be easily divided into smaller sections to allow for discussions, and weekly studies.
The text and content progress in a logical, clear fashion allowing for progression of learning.
No interface issues noted with this text.
No grammatical errors noted in the text.
No racial or culture insensitivity were noted in the text.
I would recommend this text be used in nursing schools. The use of case studies are helpful for students to learn and practice the nursing process.
Reviewed by Lisa Underwood, Practical Nursing Instructor, NTCC on 12/3/19
The text provides eight comprehensive case studies that showcase the different viewpoints of the many roles involved in patient care. It encompasses the most common seen diagnoses seen across healthcare today. Each case study comes with its own... read more
The text provides eight comprehensive case studies that showcase the different viewpoints of the many roles involved in patient care. It encompasses the most common seen diagnoses seen across healthcare today. Each case study comes with its own set of learning objectives that can be tweaked to fit several allied health courses. Although the case studies are designed around the Canadian Healthcare System, they are quite easily adaptable to fit most any modern, developed healthcare system.
Content Accuracy rating: 3
Overall, the text is quite accurate. There is one significant error that needs to be addressed. It is located in the DVT case study. In the study, a popliteal artery clot is mislabeled as a DVT. DVTs are located in veins, not in arteries. That said, the case study on the whole is quite good. This case study could be used as a learning tool in the classroom for discussion purposes or as a way to test student understanding of DVTs, on example might be, "Can they spot the error?"
At this time, all of the case studies within the text are current. Healthcare is an ever evolving field that rests on the best evidence based practice. Keeping that in mind, educators can easily adapt the studies as the newest evidence emerges and changes practice in healthcare.
All of the case studies are well written and easy to understand. The text includes several hyperlinks and it also highlights certain medical terminology to prompt readers as a way to enhance their learning experience.
Across the text, the language, style, and format of the case studies are completely consistent.
The text is divided into eight separate case studies. Each case study may be used independently of the others. All case studies are further broken down as the focus patient passes through each aspect of their healthcare system. The text's modularity makes it possible to use a case study as individual work, group projects, class discussions, homework or in a simulation lab.
The case studies and the diagnoses that they cover are presented in such a way that educators and allied health students can easily follow and comprehend.
The book in itself is free of any image distortion and it prints nicely. The text is offered in a variety of digital formats. As noted in the above reviews, some of the hyperlinks have navigational issues. When the reader attempts to access them, a "page not found" message is received.
There were minimal grammatical errors. Some of which may be traced back to the differences in our spelling.
The text is culturally relevant in that it includes patients from many different backgrounds and ethnicities. This allows educators and students to explore cultural relevance and sensitivity needs across all areas in healthcare. I do not believe that the text was in any way insensitive or offensive to the reader.
By using the case studies, it may be possible to have an open dialogue about the differences noted in healthcare systems. Students will have the ability to compare and contrast the Canadian healthcare system with their own. I also firmly believe that by using these case studies, students can improve their critical thinking skills. These case studies help them to "put it all together".
Reviewed by Melanie McGrath, Associate Professor, TRAILS on 11/29/19
The text covered some of the most common conditions seen by healthcare providers in a hospital setting, which forms a solid general base for the discussions based on each case. read more
The text covered some of the most common conditions seen by healthcare providers in a hospital setting, which forms a solid general base for the discussions based on each case.
I saw no areas of inaccuracy
As in all healthcare texts, treatments and/or tests will change frequently. However, everything is currently up-to-date thus it should be a good reference for several years.
Each case is written so that any level of healthcare student would understand. Hyperlinks in the text is also very helpful.
All of the cases are written in a similar fashion.
Although not structured as a typical text, each case is easily assigned as a stand-alone.
Each case is organized clearly in an appropriate manner.
I did not see any issues.
I did not see any grammatical errors
The text seemed appropriately inclusive. There are no pediatric cases and no cases of intellectually-impaired patients, but those types of cases introduce more advanced problem-solving which perhaps exceed the scope of the text. May be a good addition to the text.
I found this text to be an excellent resource for healthcare students in a variety of fields. It would be best utilized in inter professional courses to help guide discussion.
Reviewed by Lynne Umbarger, Clinical Assistant Professor, Occupational Therapy, Emory and Henry College on 11/26/19
While the book does not cover every scenario, the ones in the book are quite common and troublesome for inexperienced allied health students. The information in the book is thorough enough, and I have found the cases easy to modify for educational... read more
While the book does not cover every scenario, the ones in the book are quite common and troublesome for inexperienced allied health students. The information in the book is thorough enough, and I have found the cases easy to modify for educational purposes. The material was easily understood by the students but challenging enough for classroom discussion. There are no mentions in the book about occupational therapy, but it is easy enough to add a couple words and make inclusion simple.
Very nice lab values are provided in the case study, making it more realistic for students.
These case studies focus on commonly encountered diagnoses for allied health and nursing students. They are comprehensive, realistic, and easily understood. The only difference is that the hospital in one case allows the patient's dog to visit in the room (highly unusual in US hospitals).
The material is easily understood by allied health students. The cases have links to additional learning materials for concepts that may be less familiar or should be explored further in a particular health field.
The language used in the book is consistent between cases. The framework is the same with each case which makes it easier to locate areas that would be of interest to a particular allied health profession.
The case studies are comprehensive but well-organized. They are short enough to be useful for class discussion or a full-blown assignment. The students seem to understand the material and have not expressed that any concepts or details were missing.
Each case is set up like the other cases. There are learning objectives at the beginning of each case to facilitate using the case, and it is easy enough to pull out material to develop useful activities and assignments.
There is a quick chart in the Appendix to allow the reader to determine the professions involved in each case as well as the pertinent settings and diagnoses for each case study. The contents are easy to access even while reading the book.
As a person who attends carefully to grammar, I found no errors in all of the material I read in this book.
There are a greater number of people of different ethnicities, socioeconomic status, ages, and genders to make this a very useful book. With each case, I could easily picture the person in the case. This book appears to be Canadian and more inclusive than most American books.
I was able to use this book the first time I accessed it to develop a classroom activity for first-year occupational therapy students and a more comprehensive activity for second-year students. I really appreciate the links to a multitude of terminology and medical lab values/issues for each case. I will keep using this book.
Reviewed by Cindy Krentz, Assistant Professor, Metropolitan State University of Denver on 6/15/19
The book covers eight case studies of common inpatient or emergency department scenarios. I appreciated that they had written out the learning objectives. I liked that the patient was described before the case was started, giving some... read more
The book covers eight case studies of common inpatient or emergency department scenarios. I appreciated that they had written out the learning objectives. I liked that the patient was described before the case was started, giving some understanding of the patient's background. I think it could benefit from having a glossary. I liked how the authors included the vital signs in an easily readable bar. I would have liked to see the labs also highlighted like this. I also felt that it would have been good written in a 'what would you do next?' type of case study.
The book is very accurate in language, what tests would be prudent to run and in the day in the life of the hospital in all cases. One inaccuracy is that the authors called a popliteal artery clot a DVT. The rest of the DVT case study was great, though, but the one mistake should be changed.
The book is up to date for now, but as tests become obsolete and new equipment is routinely used, the book ( like any other health textbook) will need to be updated. It would be easy to change, however. All that would have to happen is that the authors go in and change out the test to whatever newer, evidence-based test is being utilized.
The text is written clearly and easy to understand from a student's perspective. There is not too much technical jargon, and it is pretty universal when used- for example DVT for Deep Vein Thrombosis.
The book is consistent in language and how it is broken down into case studies. The same format is used for highlighting vital signs throughout the different case studies. It's great that the reader does not have to read the book in a linear fashion. Each case study can be read without needing to read the others.
The text is broken down into eight case studies, and within the case studies is broken down into days. It is consistent and shows how the patient can pass through the different hospital departments (from the ER to the unit, to surgery, to home) in a realistic manner. The instructor could use one or more of the case studies as (s)he sees fit.
The topics are eight different case studies- and are presented very clearly and organized well. Each one is broken down into how the patient goes through the system. The text is easy to follow and logical.
The interface has some problems with the highlighted blue links. Some of them did not work and I got a 'page not found' message. That can be frustrating for the reader. I'm wondering if a glossary could be utilized (instead of the links) to explain what some of these links are supposed to explain.
I found two or three typos, I don't think they were grammatical errors. In one case I think the Canadian spelling and the United States spelling of the word are just different.
This is a very culturally competent book. In today's world, however, one more type of background that would merit delving into is the trans-gender, GLBTQI person. I was glad that there were no stereotypes.
I enjoyed reading the text. It was interesting and relevant to today's nursing student. Since we are becoming more interprofessional, I liked that we saw what the phlebotomist and other ancillary personnel (mostly different technicians) did. I think that it could become even more interdisciplinary so colleges and universities could have more interprofessional education- courses or simulations- with the addition of the nurse using social work, nutrition, or other professional health care majors.
Reviewed by Catherine J. Grott, Interim Director, Health Administration Program, TRAILS on 5/5/19
The book is comprehensive but is specifically written for healthcare workers practicing in Canada. The title of the book should reflect this. read more
The book is comprehensive but is specifically written for healthcare workers practicing in Canada. The title of the book should reflect this.
The book is accurate, however it has numerous broken online links.
Relevance/Longevity rating: 3
The content is very relevant, but some links are out-dated. For example, WHO Guidelines for Safe Surgery 2009 (p. 186) should be updated.
The book is written in clear and concise language. The side stories about the healthcare workers make the text interesting.
The book is consistent in terms of terminology and framework. Some terms that are emphasized in one case study are not emphasized (with online links) in the other case studies. All of the case studies should have the same words linked to online definitions.
Modularity rating: 3
The book can easily be parsed out if necessary. However, the way the case studies have been written, it's evident that different authors contributed singularly to each case study.
The organization and flow are good.
Interface rating: 1
There are numerous broken online links and "pages not found."
The grammar and punctuation are correct. There are two errors detected: p. 120 a space between the word "heart" and the comma; also a period is needed after Dr (p. 113).
I'm not quite sure that the social worker (p. 119) should comment that the patient and partner are "very normal people."
There are roughly 25 broken online links or "pages not found." The BC & Canadian Guidelines (p. 198) could also include a link to US guidelines to make the text more universal . The basilar crackles (p. 166) is very good. Text could be used compare US and Canadian healthcare. Text could be enhanced to teach "soft skills" and interdepartmental communication skills in healthcare.
Reviewed by Lindsey Henry, Practical Nursing Instructor, Fletcher on 5/1/19
I really appreciated how in the introduction, five learning objectives were identified for students. These objectives are paramount in nursing care and they are each spelled out for the learner. Each Case study also has its own learning... read more
I really appreciated how in the introduction, five learning objectives were identified for students. These objectives are paramount in nursing care and they are each spelled out for the learner. Each Case study also has its own learning objectives, which were effectively met in the readings.
As a seasoned nurse, I believe that the content regarding pathophysiology and treatments used in the case studies were accurate. I really appreciated how many of the treatments were also explained and rationales were given, which can be very helpful to facilitate effective learning for a nursing student or novice nurse.
The case studies are up to date and correlate with the current time period. They are easily understood.
I really loved how several important medical terms, including specific treatments were highlighted to alert the reader. Many interventions performed were also explained further, which is great to enhance learning for the nursing student or novice nurse. Also, with each scenario, a background and history of the patient is depicted, as well as the perspectives of the patient, patients family member, and the primary nurse. This really helps to give the reader a full picture of the day in the life of a nurse or a patient, and also better facilitates the learning process of the reader.
These case studies are consistent. They begin with report, the patient background or updates on subsequent days, and follow the patients all the way through discharge. Once again, I really appreciate how this book describes most if not all aspects of patient care on a day to day basis.
Each case study is separated into days. While they can be divided to be assigned at different points within the course, they also build on each other. They show trends in vital signs, what happens when a patient deteriorates, what happens when they get better and go home. Showing the entire process from ER admit to discharge is really helpful to enhance the students learning experience.
The topics are all presented very similarly and very clearly. The way that the scenarios are explained could even be understood by a non-nursing student as well. The case studies are very clear and very thorough.
The book is very easy to navigate, prints well on paper, and is not distorted or confusing.
I did not see any grammatical errors.
Each case study involves a different type of patient. These differences include race, gender, sexual orientation and medical backgrounds. I do not feel the text was offensive to the reader.
I teach practical nursing students and after reading this book, I am looking forward to implementing it in my classroom. Great read for nursing students!
Reviewed by Leah Jolly, Instructor, Clinical Coordinator, Oregon Institute of Technology on 4/10/19
Good variety of cases and pathologies covered. read more
Good variety of cases and pathologies covered.
Content Accuracy rating: 2
Some examples and scenarios are not completely accurate. For example in the DVT case, the sonographer found thrombus in the "popliteal artery", which according to the book indicated presence of DVT. However in DVT, thrombus is located in the vein, not the artery. The patient would also have much different symptoms if located in the artery. Perhaps some of these inaccuracies are just typos, but in real-life situations this simple mistake can make a world of difference in the patient's course of treatment and outcomes.
Good examples of interprofessional collaboration. If only it worked this way on an every day basis!
Clear and easy to read for those with knowledge of medical terminology.
Good consistency overall.
Broken up well.
Topics are clear and logical.
Would be nice to simply click through to the next page, rather than going through the table of contents each time.
Minor typos/grammatical errors.
No offensive or insensitive materials observed.
Reviewed by Alex Sargsyan, Doctor of Nursing Practice/Assistant Professor , East Tennessee State University on 10/8/18
Because of the case study character of the book it does not have index or glossary. However it has summary for each health case study outlining key elements discussed in each case study. read more
Because of the case study character of the book it does not have index or glossary. However it has summary for each health case study outlining key elements discussed in each case study.
Overall the book is accurately depicting the clinical environment. There are numerous references to external sites. While most of them are correct, some of them are not working. For example Homan’s test link is not working "404 error"
Book is relevant in its current version and can be used in undergraduate and graduate classes. That said, the longevity of the book may be limited because of the character of the clinical education. Clinical guidelines change constantly and it may require a major update of the content.
Cases are written very clearly and have realistic description of an inpatient setting.
The book is easy to read and consistent in the language in all eight cases.
The cases are very well written. Each case is subdivided into logical segments. The segments reflect different setting where the patient is being seen. There is a flow and transition between the settings.
Book has eight distinct cases. This is a great format for a book that presents distinct clinical issues. This will allow the students to have immersive experiences and gain better understanding of the healthcare environment.
Book is offered in many different formats. Besides the issues with the links mentioned above, overall navigation of the book content is very smooth.
Book is very well written and has no grammatical errors.
Book is culturally relevant. Patients in the case studies come different cultures and represent diverse ethnicities.
Reviewed by Justin Berry, Physical Therapist Assistant Program Director, Northland Community and Technical College, East Grand Forks, MN on 8/2/18
This text provides eight patient case studies from a variety of diagnoses, which can be utilized by healthcare students from multiple disciplines. The cases are comprehensive and can be helpful for students to determine professional roles,... read more
This text provides eight patient case studies from a variety of diagnoses, which can be utilized by healthcare students from multiple disciplines. The cases are comprehensive and can be helpful for students to determine professional roles, interprofessional roles, when to initiate communication with other healthcare practitioners due to a change in patient status, and treatment ideas. Some additional patient information, such as lab values, would have been beneficial to include.
Case study information is accurate and unbiased.
Content is up to date. The case studies are written in a way so that they will not be obsolete soon, even with changes in healthcare.
The case studies are well written, and can be utilized for a variety of classroom assignments, discussions, and projects. Some additional lab value information for each patient would have been a nice addition.
The case studies are consistently organized to make it easy for the reader to determine the framework.
The text is broken up into eight different case studies for various patient diagnoses. This design makes it highly modular, and would be easy to assign at different points of a course.
The flow of the topics are presented consistently in a logical manner. Each case study follows a patient chronologically, making it easy to determine changes in patient status and treatment options.
The text is free of interface issues, with no distortion of images or charts.
The text is not culturally insensitive or offensive in any way. Patients are represented from a variety of races, ethnicities, and backgrounds
This book would be a good addition for many different health programs.
Reviewed by Ann Bell-Pfeifer, Instructor/Program Director, Minnesota State Community and Technical College on 5/21/18
The book gives a comprehensive overview of many types of cases for patient conditions. Emergency Room patients may arrive with COPD, heart failure, sepsis, pneumonia, or as motor vehicle accident victims. It is directed towards nurses, medical... read more
The book gives a comprehensive overview of many types of cases for patient conditions. Emergency Room patients may arrive with COPD, heart failure, sepsis, pneumonia, or as motor vehicle accident victims. It is directed towards nurses, medical laboratory technologists, medical radiology technologists, and respiratory therapists and their roles in caring for patients. Most of the overview is accurate. One suggestion is to provide an embedded radiologist interpretation of the exams which are performed which lead to the patients diagnosis.
Overall the book is accurate. Would like to see updates related to the addition of direct radiography technology which is commonly used in the hospital setting.
Many aspects of medicine will remain constant. The case studies seem fairly accurate and may be relevant for up to 3 years. Since technology changes so quickly in medicine, the CT and x-ray components may need minor updates within a few years.
The book clarity is excellent.
The case stories are consistent with each scenario. It is easy to follow the structure and learn from the content.
The book is quite modular. It is easy to break it up into cases and utilize them individually and sequentially.
The cases are listed by disease process and follow a logical flow through each condition. They are easy to follow as they have the same format from the beginning to the end of each case.
The interface seems seamless. Hyperlinks are inserted which provide descriptions and references to medical procedures and in depth definitions.
The book is free of most grammatical errors. There is a place where a few words do not fit the sentence structure and could be a typo.
The book included all types of relationships and ethnic backgrounds. One type which could be added is a transgender patient.
I think the book was quite useful for a variety of health care professionals. The authors did an excellent job of integrating patient cases which could be applied to the health care setting. The stories seemed real and relevant. This book could be used to teach health care professionals about integrated care within the emergency department.
Reviewed by Shelley Wolfe, Assistant Professor, Winona State University on 5/21/18
This text is comprised of comprehensive, detailed case studies that provide the reader with multiple character views throughout a patient’s encounter with the health care system. The Table of Contents accurately reflected the content. It should... read more
This text is comprised of comprehensive, detailed case studies that provide the reader with multiple character views throughout a patient’s encounter with the health care system. The Table of Contents accurately reflected the content. It should be noted that the authors include a statement that conveys that this text is not like traditional textbooks and is not meant to be read in a linear fashion. This allows the educator more flexibility to use the text as a supplement to enhance learning opportunities.
The content of the text appears accurate and unbiased. The “five overarching learning objectives” provide a clear aim of the text and the educator is able to glean how these objectives are captured into each of the case studies. While written for the Canadian healthcare system, this text is easily adaptable to the American healthcare system.
Overall, the content is up-to-date and the case studies provide a variety of uses that promote longevity of the text. However, not all of the blue font links (if using the digital PDF version) were still in working order. I encountered links that led to error pages or outdated “page not found” websites. While the links can be helpful, continued maintenance of these links could prove time-consuming.
I found the text easy to read and understand. I enjoyed that the viewpoints of all the different roles (patient, nurse, lab personnel, etc.) were articulated well and allowed the reader to connect and gain appreciation of the entire healthcare team. Medical jargon was noted to be appropriate for the intended audience of this text.
The terminology and organization of this text is consistent.
The text is divided into 8 case studies that follow a similar organizational structure. The case studies can further be divided to focus on individual learning objectives. For example, the case studies could be looked at as a whole for discussing communication or could be broken down into segments to focus on disease risk factors.
The case studies in this text follow a similar organizational structure and are consistent in their presentation. The flow of individual case studies is excellent and sets the reader on a clear path. As noted previously, this text is not meant to be read in a linear fashion.
This text is available in many different forms. I chose to review the text in the digital PDF version in order to use the embedded links. I did not encounter significant interface issues and did not find any images or features that would distract or confuse a reader.
No significant grammatical errors were noted.
The case studies in this text included patients and healthcare workers from a variety of backgrounds. Educators and students will benefit from expanding the case studies to include discussions and other learning opportunities to help develop culturally-sensitive healthcare providers.
I found the case studies to be very detailed, yet written in a way in which they could be used in various manners. The authors note a variety of ways in which the case studies could be employed with students; however, I feel the authors could also include that the case studies could be used as a basis for simulated clinical experiences. The case studies in this text would be an excellent tool for developing interprofessional communication and collaboration skills in a variety healthcare students.
Reviewed by Darline Foltz, Assistant Professor, University of Cincinnati - Clermont College on 3/27/18
This book covers all areas listed in the Table of Contents. In addition to the detailed patient case studies, there is a helpful section of "How to Use this Resource". I would like to note that this resource "aligns with the open textbooks... read more
This book covers all areas listed in the Table of Contents. In addition to the detailed patient case studies, there is a helpful section of "How to Use this Resource". I would like to note that this resource "aligns with the open textbooks Clinical Procedures for Safer Patient Care and Anatomy and Physiology: OpenStax" as noted by the authors.
The book appears to be accurate. Although one of the learning outcomes is as follows: "Demonstrate an understanding of the Canadian healthcare delivery system.", I did not find anything that is ONLY specific to the Canadian healthcare delivery system other than some of the terminology, i.e. "porter" instead of "transporter" and a few french words. I found this to make the book more interesting for students rather than deter from it. These are patient case studies that are relevant in any country.
The content is up-to-date. Changes in medical science may occur, i.e. a different test, to treat a diagnosis that is included in one or more of the case studies, however, it would be easy and straightforward to implement these changes.
This book is written in lucid, accessible prose. The technical/medical terminology that is used is appropriate for medical and allied health professionals. Something that would improve this text would to provide a glossary of terms for the terms in blue font.
This book is consistent with current medical terminology
This text is easily divided into each of the 6 case studies. The case studies can be used singly according to the body system being addressed or studied.
Because this text is a collection of case studies, flow doesn't pertain, however the organization and structure of the case studies are excellent as they are clear and easy to read.
There are no distractions in this text that would distract or confuse the reader.
I did not identify any grammatical errors.
This text is not culturally insensitive or offensive in any way and uses patients and healthcare workers that are of a variety of races, ethnicities and backgrounds.
I believe that this text would not only be useful to students enrolled in healthcare professions involved in direct patient care but would also be useful to students in supporting healthcare disciplines such as health information technology and management, medical billing and coding, etc.
Table of Contents
- Introduction
Case Study #1: Chronic Obstructive Pulmonary Disease (COPD)
- Learning Objectives
- Patient: Erin Johns
- Emergency Room
Case Study #2: Pneumonia
- Day 0: Emergency Room
- Day 1: Emergency Room
- Day 1: Medical Ward
- Day 2: Medical Ward
- Day 3: Medical Ward
- Day 4: Medical Ward
Case Study #3: Unstable Angina (UA)
- Patient: Harj Singh
Case Study #4: Heart Failure (HF)
- Patient: Meryl Smith
- In the Supermarket
- Day 0: Medical Ward
Case Study #5: Motor Vehicle Collision (MVC)
- Patient: Aaron Knoll
- Crash Scene
- Operating Room
- Post Anaesthesia Care Unit (PACU)
- Surgical Ward
Case Study #6: Sepsis
- Patient: George Thomas
- Sleepy Hollow Care Facility
Case Study #7: Colon Cancer
- Patient: Fred Johnson
- Two Months Ago
- Pre-Surgery Admission
Case Study #8: Deep Vein Thrombosis (DVT)
- Patient: Jamie Douglas
Appendix: Overview About the Authors
Ancillary Material
About the book.
Health Case Studies is composed of eight separate health case studies. Each case study includes the patient narrative or story that models the best practice (at the time of publishing) in healthcare settings. Associated with each case is a set of specific learning objectives to support learning and facilitate educational strategies and evaluation.
The case studies can be used online in a learning management system, in a classroom discussion, in a printed course pack or as part of a textbook created by the instructor. This flexibility is intentional and allows the educator to choose how best to convey the concepts presented in each case to the learner.
Because these case studies were primarily developed for an electronic healthcare system, they are based predominantly in an acute healthcare setting. Educators can augment each case study to include primary healthcare settings, outpatient clinics, assisted living environments, and other contexts as relevant.
About the Contributors
Glynda Rees teaches at the British Columbia Institute of Technology (BCIT) in Vancouver, British Columbia. She completed her MSN at the University of British Columbia with a focus on education and health informatics, and her BSN at the University of Cape Town in South Africa. Glynda has many years of national and international clinical experience in critical care units in South Africa, the UK, and the USA. Her teaching background has focused on clinical education, problem-based learning, clinical techniques, and pharmacology.
Glynda‘s interests include the integration of health informatics in undergraduate education, open accessible education, and the impact of educational technologies on nursing students’ clinical judgment and decision making at the point of care to improve patient safety and quality of care.
Faculty member in the critical care nursing program at the British Columbia Institute of Technology (BCIT) since 2003, Rob has been a critical care nurse for over 25 years with 17 years practicing in a quaternary care intensive care unit. Rob is an experienced educator and supports student learning in the classroom, online, and in clinical areas. Rob’s Master of Education from Simon Fraser University is in educational technology and learning design. He is passionate about using technology to support learning for both faculty and students.
Part of Rob’s faculty position is dedicated to providing high fidelity simulation support for BCIT’s nursing specialties program along with championing innovative teaching and best practices for educational technology. He has championed the use of digital publishing and was the tech lead for Critical Care Nursing’s iPad Project which resulted in over 40 multi-touch interactive textbooks being created using Apple and other technologies.
Rob has successfully completed a number of specialist certifications in computer and network technologies. In 2015, he was awarded Apple Distinguished Educator for his innovation and passionate use of technology to support learning. In the past five years, he has presented and published abstracts on virtual simulation, high fidelity simulation, creating engaging classroom environments, and what the future holds for healthcare and education.
Janet Morrison is the Program Head of Occupational Health Nursing at the British Columbia Institute of Technology (BCIT) in Burnaby, British Columbia. She completed a PhD at Simon Fraser University, Faculty of Communication, Art and Technology, with a focus on health information technology. Her dissertation examined the effects of telehealth implementation in an occupational health nursing service. She has an MA in Adult Education from St. Francis Xavier University and an MA in Library and Information Studies from the University of British Columbia.
Janet’s research interests concern the intended and unintended impacts of health information technologies on healthcare students, faculty, and the healthcare workforce.
She is currently working with BCIT colleagues to study how an educational clinical information system can foster healthcare students’ perceptions of interprofessional roles.
Contribute to this Page
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- Write for Us
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 21, Issue 1
- What is a case study?
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Roberta Heale 1 ,
- Alison Twycross 2
- 1 School of Nursing , Laurentian University , Sudbury , Ontario , Canada
- 2 School of Health and Social Care , London South Bank University , London , UK
- Correspondence to Dr Roberta Heale, School of Nursing, Laurentian University, Sudbury, ON P3E2C6, Canada; rheale{at}laurentian.ca
https://doi.org/10.1136/eb-2017-102845
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
What is it?
Case study is a research methodology, typically seen in social and life sciences. There is no one definition of case study research. 1 However, very simply… ‘a case study can be defined as an intensive study about a person, a group of people or a unit, which is aimed to generalize over several units’. 1 A case study has also been described as an intensive, systematic investigation of a single individual, group, community or some other unit in which the researcher examines in-depth data relating to several variables. 2
Often there are several similar cases to consider such as educational or social service programmes that are delivered from a number of locations. Although similar, they are complex and have unique features. In these circumstances, the evaluation of several, similar cases will provide a better answer to a research question than if only one case is examined, hence the multiple-case study. Stake asserts that the cases are grouped and viewed as one entity, called the quintain . 6 ‘We study what is similar and different about the cases to understand the quintain better’. 6
The steps when using case study methodology are the same as for other types of research. 6 The first step is defining the single case or identifying a group of similar cases that can then be incorporated into a multiple-case study. A search to determine what is known about the case(s) is typically conducted. This may include a review of the literature, grey literature, media, reports and more, which serves to establish a basic understanding of the cases and informs the development of research questions. Data in case studies are often, but not exclusively, qualitative in nature. In multiple-case studies, analysis within cases and across cases is conducted. Themes arise from the analyses and assertions about the cases as a whole, or the quintain, emerge. 6
Benefits and limitations of case studies
If a researcher wants to study a specific phenomenon arising from a particular entity, then a single-case study is warranted and will allow for a in-depth understanding of the single phenomenon and, as discussed above, would involve collecting several different types of data. This is illustrated in example 1 below.
Using a multiple-case research study allows for a more in-depth understanding of the cases as a unit, through comparison of similarities and differences of the individual cases embedded within the quintain. Evidence arising from multiple-case studies is often stronger and more reliable than from single-case research. Multiple-case studies allow for more comprehensive exploration of research questions and theory development. 6
Despite the advantages of case studies, there are limitations. The sheer volume of data is difficult to organise and data analysis and integration strategies need to be carefully thought through. There is also sometimes a temptation to veer away from the research focus. 2 Reporting of findings from multiple-case research studies is also challenging at times, 1 particularly in relation to the word limits for some journal papers.
Examples of case studies
Example 1: nurses’ paediatric pain management practices.
One of the authors of this paper (AT) has used a case study approach to explore nurses’ paediatric pain management practices. This involved collecting several datasets:
Observational data to gain a picture about actual pain management practices.
Questionnaire data about nurses’ knowledge about paediatric pain management practices and how well they felt they managed pain in children.
Questionnaire data about how critical nurses perceived pain management tasks to be.
These datasets were analysed separately and then compared 7–9 and demonstrated that nurses’ level of theoretical did not impact on the quality of their pain management practices. 7 Nor did individual nurse’s perceptions of how critical a task was effect the likelihood of them carrying out this task in practice. 8 There was also a difference in self-reported and observed practices 9 ; actual (observed) practices did not confirm to best practice guidelines, whereas self-reported practices tended to.
Example 2: quality of care for complex patients at Nurse Practitioner-Led Clinics (NPLCs)
The other author of this paper (RH) has conducted a multiple-case study to determine the quality of care for patients with complex clinical presentations in NPLCs in Ontario, Canada. 10 Five NPLCs served as individual cases that, together, represented the quatrain. Three types of data were collected including:
Review of documentation related to the NPLC model (media, annual reports, research articles, grey literature and regulatory legislation).
Interviews with nurse practitioners (NPs) practising at the five NPLCs to determine their perceptions of the impact of the NPLC model on the quality of care provided to patients with multimorbidity.
Chart audits conducted at the five NPLCs to determine the extent to which evidence-based guidelines were followed for patients with diabetes and at least one other chronic condition.
The three sources of data collected from the five NPLCs were analysed and themes arose related to the quality of care for complex patients at NPLCs. The multiple-case study confirmed that nurse practitioners are the primary care providers at the NPLCs, and this positively impacts the quality of care for patients with multimorbidity. Healthcare policy, such as lack of an increase in salary for NPs for 10 years, has resulted in issues in recruitment and retention of NPs at NPLCs. This, along with insufficient resources in the communities where NPLCs are located and high patient vulnerability at NPLCs, have a negative impact on the quality of care. 10
These examples illustrate how collecting data about a single case or multiple cases helps us to better understand the phenomenon in question. Case study methodology serves to provide a framework for evaluation and analysis of complex issues. It shines a light on the holistic nature of nursing practice and offers a perspective that informs improved patient care.
- Gustafsson J
- Calanzaro M
- Sandelowski M
Competing interests None declared.
Provenance and peer review Commissioned; internally peer reviewed.
Read the full text or download the PDF:

Move fast, think slow: How financial services can strike a balance with GenAI

Take on Tomorrow @ the World Economic Forum in Davos: Energy demand

PwC’s Global Investor Survey 2023

Climate risk, resilience and adaptation

Business transformation

Sustainability assurance

The Leadership Agenda
AI Jobs Barometer

The s+b digital issue: Corporate “power changers”

The New Equation

PwC’s Global Annual Review

Committing to Net Zero

The Solvers Challenge
Loading Results
No Match Found
Case studies
Demonstrating our purpose in our work.
PwC's purpose is to "build trust in society and solve important problems." Our Partners and staff demonstrate a commitment to this purpose every day in the work we do with our Health Services clients. We do so because of a deep and passionate recognition of the importance of health to society - because health matters. The following case studies are an example of just a few engagements that show our strong desire to make a difference.
Working with clients to make an impact
We work side by side with health organizations and community residents, to improve health and wellness. The stories featured here illustrate the importance of working together to solve the complex health challenges we face. When we collaborate, our strengths are amplified. See how we are working together to solve complex health challenges.
{{filterContent.facetedTitle}}
{{item.publishDate}}
{{item.title}}
{{item.text}}

Ron Chopoorian
Global Health Industries Leader, Partner, PwC United States
© 2017 - 2024 PwC. All rights reserved. PwC refers to the PwC network and/or one or more of its member firms, each of which is a separate legal entity. Please see www.pwc.com/structure for further details.
- Legal notices
- Cookie policy
- Legal disclaimer
- Terms and conditions
- Browse All Articles
- Newsletter Sign-Up

- 30 May 2024
- Research & Ideas
Racial Bias Might Be Infecting Patient Portals. Can AI Help?
Doctors and patients turned to virtual communication when the pandemic made in-person appointments risky. But research by Ariel Stern and Mitchell Tang finds that providers' responses can vary depending on a patient's race. Could technology bring more equity to portals?
- 21 May 2024
- Cold Call Podcast
The Importance of Trust for Managing through a Crisis
In March 2020, Twiddy & Company, a family-owned vacation rental company known for hospitality rooted in personal interactions, needed to adjust to contactless, remote customer service. With the upcoming vacation season thrown into chaos, President Clark Twiddy had a responsibility to the company’s network of homeowners who rented their homes through the company, to guests who had booked vacations, and to employees who had been recruited by Twiddy’s reputation for treating staff well. Who, if anyone, could he afford to make whole and keep happy? Harvard Business School professor Sandra Sucher, author of the book The Power of Trust: How Companies Build It, Lose It, Regain It, discusses how Twiddy leaned into trust to weather the COVID-19 pandemic in her case, “Twiddy & Company: Trust in a Chaotic Environment.”

- 09 Feb 2024
Slim Chance: Drugs Will Reshape the Weight Loss Industry, But Habit Change Might Be Elusive
Medications such as Ozempic, Wegovy, and Mounjaro have upended a $76 billion industry that has long touted lifestyle shifts as a means to weight loss. Regina Herzlinger says these drugs might bring fast change, especially for busy professionals, but many questions remain unanswered.

- 19 Dec 2023
$15 Billion in Five Years: What Data Tells Us About MacKenzie Scott’s Philanthropy
Scott's hands-off approach and unparalleled pace—helping almost 2,000 organizations and counting—has upended the status quo in philanthropy. While her donations might seem scattershot, an analysis of five years of data by Matthew Lee, Brian Trelstad, and Ethan Tran highlights clear trends and an emerging strategy.

- 09 Nov 2023
What Will It Take to Confront the Invisible Mental Health Crisis in Business?
The pressure to do more, to be more, is fueling its own silent epidemic. Lauren Cohen discusses the common misperceptions that get in the way of supporting employees' well-being, drawing on case studies about people who have been deeply affected by mental illness.

- 03 Oct 2023
- Research Event
Build the Life You Want: Arthur Brooks and Oprah Winfrey Share Happiness Tips
"Happiness is not a destination. It's a direction." In this video, Arthur C. Brooks and Oprah Winfrey reflect on mistakes, emotions, and contentment, sharing lessons from their new book.

- 12 Sep 2023
Can Remote Surgeries Digitally Transform Operating Rooms?
Launched in 2016, Proximie was a platform that enabled clinicians, proctors, and medical device company personnel to be virtually present in operating rooms, where they would use mixed reality and digital audio and visual tools to communicate with, mentor, assist, and observe those performing medical procedures. The goal was to improve patient outcomes. The company had grown quickly, and its technology had been used in tens of thousands of procedures in more than 50 countries and 500 hospitals. It had raised close to $50 million in equity financing and was now entering strategic partnerships to broaden its reach. Nadine Hachach-Haram, founder and CEO of Proximie, aspired for Proximie to become a platform that powered every operating room in the world, but she had to carefully consider the company’s partnership and data strategies in order to scale. What approach would position the company best for the next stage of growth? Harvard Business School associate professor Ariel Stern discusses creating value in health care through a digital transformation of operating rooms in her case, “Proximie: Using XR Technology to Create Borderless Operating Rooms.”

- 28 Aug 2023
How Workplace Wellness Programs Can Give Employees the Energy Boost They Need
At a time when many workers are struggling with mental health issues, workplace wellness programs need to go beyond providing gym discounts and start offering employees tailored solutions that improve their physical and emotional well-being, says Hise Gibson.
- 01 Aug 2023
Can Business Transform Primary Health Care Across Africa?
mPharma, headquartered in Ghana, is trying to create the largest pan-African health care company. Their mission is to provide primary care and a reliable and fairly priced supply of drugs in the nine African countries where they operate. Co-founder and CEO Gregory Rockson needs to decide which component of strategy to prioritize in the next three years. His options include launching a telemedicine program, expanding his pharmacies across the continent, and creating a new payment program to cover the cost of common medications. Rockson cares deeply about health equity, but his venture capital-financed company also must be profitable. Which option should he focus on expanding? Harvard Business School Professor Regina Herzlinger and case protagonist Gregory Rockson discuss the important role business plays in improving health care in the case, “mPharma: Scaling Access to Affordable Primary Care in Africa.”

- 25 Jul 2023
Could a Business Model Help Big Pharma Save Lives and Profit?
Gilead Sciences used a novel approach to help Egypt address a public health crisis while sustaining profits from a key product. V. Kasturi Rangan and participants at a recent seminar hosted by the Institute for the Study of Business in Global Society discussed what it would take to apply the model more widely.

- 23 Jun 2023
This Company Lets Employees Take Charge—Even with Life and Death Decisions
Dutch home health care organization Buurtzorg avoids middle management positions and instead empowers its nurses to care for patients as they see fit. Tatiana Sandino and Ethan Bernstein explore how removing organizational layers and allowing employees to make decisions can boost performance.
- 09 May 2023
Can Robin Williams’ Son Help Other Families Heal Addiction and Depression?
Zak Pym Williams, son of comedian and actor Robin Williams, had seen how mental health challenges, such as addiction and depression, had affected past generations of his family. Williams was diagnosed with generalized anxiety disorder, depression, and post-traumatic stress disorder (PTSD) as a young adult and he wanted to break the cycle for his children. Although his children were still quite young, he began considering proactive strategies that could help his family’s mental health, and he wanted to share that knowledge with other families. But how can Williams help people actually take advantage of those mental health strategies and services? Professor Lauren Cohen discusses his case, “Weapons of Self Destruction: Zak Pym Williams and the Cultivation of Mental Wellness.”
- 26 Apr 2023
How Martine Rothblatt Started a Company to Save Her Daughter
When serial entrepreneur Martine Rothblatt (founder of Sirius XM) received her seven-year-old daughter’s diagnosis of Pulmonary Arterial Hypertension (PAH), she created United Therapeutics and developed a drug to save her life. When her daughter later needed a lung transplant, Rothblatt decided to take what she saw as the logical next step: manufacturing organs for transplantation. Rothblatt’s entrepreneurial career exemplifies a larger debate around the role of the firm in creating solutions for society’s problems. If companies are uniquely good at innovating, what voice should society have in governing the new technologies that firms create? Harvard Business School professor Debora Spar debates these questions in the case “Martine Rothblatt and United Therapeutics: A Series of Implausible Dreams.” As part of a new first-year MBA course at Harvard Business School, this case examines the central question: what is the social purpose of the firm?
- 25 Apr 2023
Using Design Thinking to Invent a Low-Cost Prosthesis for Land Mine Victims
Bhagwan Mahaveer Viklang Sahayata Samiti (BMVSS) is an Indian nonprofit famous for creating low-cost prosthetics, like the Jaipur Foot and the Stanford-Jaipur Knee. Known for its patient-centric culture and its focus on innovation, BMVSS has assisted more than one million people, including many land mine survivors. How can founder D.R. Mehta devise a strategy that will ensure the financial sustainability of BMVSS while sustaining its human impact well into the future? Harvard Business School Dean Srikant Datar discusses the importance of design thinking in ensuring a culture of innovation in his case, “BMVSS: Changing Lives, One Jaipur Limb at a Time.”

- 31 Mar 2023
Can a ‘Basic Bundle’ of Health Insurance Cure Coverage Gaps and Spur Innovation?
One in 10 people in America lack health insurance, resulting in $40 billion of care that goes unpaid each year. Amitabh Chandra and colleagues say ensuring basic coverage for all residents, as other wealthy nations do, could address the most acute needs and unlock efficiency.

- 13 Mar 2023
The Power of Personal Connections: How Shared Experiences Boost Performance
Doctors who train together go on to provide better patient care later in their careers. What could teams in other industries learn? Research by Maximilian Pany and J. Michael McWilliams.

- 14 Feb 2023
When a Vacation Isn’t Enough, a Sabbatical Can Recharge Your Life—and Your Career
Burning out and ready to quit? Consider an extended break instead. Drawing from research inspired by his own 900-mile journey, DJ DiDonna offers practical advice to help people chart a new path through a sabbatical.

- 10 Feb 2023
COVID-19 Lessons: Social Media Can Nudge More People to Get Vaccinated
Social networks have been criticized for spreading COVID-19 misinformation, but the platforms have also helped public health agencies spread the word on vaccines, says research by Michael Luca and colleagues. What does this mean for the next pandemic?

- 12 Dec 2022

Buy-In from Black Patients Suffers When Drug Trials Don’t Include Them
Diversifying clinical trials could build trust in new treatments among Black people and their physicians. Research by Joshua Schwartzstein, Marcella Alsan, and colleagues probes the ripple effects of underrepresentation in testing, and offers a call to action for drugmakers.

- 06 Sep 2022
Curbing an Unlikely Culprit of Rising Drug Prices: Pharmaceutical Donations
Policymakers of every leaning have vowed to rein in prescription drug costs, with little success. But research by Leemore Dafny shows how closing a loophole on drugmaker donations could eliminate one driver of rising expenses.
A Lean Approach for Reducing Downtimes in Healthcare: A Case Study
- Conference paper
- First Online: 12 February 2023
- Cite this conference paper

- Stefano Frecassetti ORCID: orcid.org/0000-0002-9649-314X 19 ,
- Matteo Ferrazzi ORCID: orcid.org/0000-0001-9035-0773 19 &
- Alberto Portioli-Staudacher ORCID: orcid.org/0000-0002-9807-1215 19
Part of the book series: IFIP Advances in Information and Communication Technology ((IFIPAICT,volume 668))
Included in the following conference series:
- European Lean Educator Conference
476 Accesses
Lean Management is considered one of the most successful management paradigms for enhancing operational performance in the manufacturing environment. However, it has been applied throughout the years to several sectors and organisational areas, such as service, healthcare, and office departments. After the Covid-19 outbreak, increasing attention has been given to potential performance improvements in healthcare organisations by leveraging Lean. This paper intends to add further knowledge to this field by presenting a case study in a hospital. In this paper, a pilot project is presented carried out in a healthcare organisation. Lean methods were used to improve the operating room performance, particularly by reducing the operating room changeover time. The A3 template was used to drive the project and implement a new procedure using the Single Minute Exchange of Die (SMED) method. With the implementation of the new procedure, the changeover time between two different surgeries in the operating room was significantly reduced, together with a more stable and reliable process.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Similar content being viewed by others

Lean Healthcare
Lean Healthcare: How to Start the Lean Journey

Lean Transformation in Healthcare: A French Case Study
Amati, M., et al.: Reducing changeover time between surgeries through lean thinking: an action research project. Front. Med. 9 (2022). https://doi.org/10.3389/fmed.2022.822964
Bharsakade, R.S., Acharya, P., Ganapathy, L., Tiwari, M.K.: A lean approach to healthcare management using multi criteria decision making. Opsearch 58 (3), 610–635 (2021). https://doi.org/10.1007/s12597-020-00490-5
Article Google Scholar
Costa, F., Kassem, B., Staudacher, A.P.: Lean office in a manufacturing company. In: Powell, D.J., Alfnes, E., Holmemo, M.D.Q., Reke, E. (eds.) Learning in the Digital Era. IFIP Advances in Information and Communication Technology, pp. 351–356. Springer, Cham (2021). https://doi.org/10.1007/978-3-030-92934-3_36
Chapter Google Scholar
Costa, F., Kassem, B., Portioli-Staudacher, A.: Lean thinking application in the healthcare sector. In: Powell, D.J., Alfnes, E., Holmemo, M.D.Q., Reke, E. (eds.) Learning in the Digital Era. IFIP Advances in Information and Communication Technology, pp. 357–364. Springer, Cham (2021). https://doi.org/10.1007/978-3-030-92934-3_37
Curatolo, N., Lamouri, S., Huet, J.C., Rieutord, A.: A critical analysis of Lean approach structuring in hospitals. Bus. Process Manag. J. 20 (3), 433–454 (2014)
D’Andreamatteo, A., Iannia, L., Lega, F., Sargiacomo, M.: Lean in healthcare: a comprehensive review. Health Policy 119 (9), 1197–1209 (2015)
Guercini, J., et al.: Application of SMED methodology for the improvement of operations in operating theatres. The case of the Azienda Ospedaliera Universitaria Senese. Mecosan 24 (98), 83–203 (2016). https://doi.org/10.3280/mesa2016-098005
Henrique, D.B., Godinho Filho, M.: A systematic literature review of empirical research in Lean and Six Sigma in healthcare. Total Qual. Manag. Bus. Excell. 31 (3–4), 429–449 (2020)
Henrique, D.B., Filho, M.G., Marodin, G., Jabbour, A.B.L.D.S., Chiappetta Jabbour, C.J.: A framework to assess sustaining continuous improvement in lean healthcare. Int. J. Prod. Res. 59 (10), 2885–2904 (2020)
Holweg, M.: The genealogy of lean production. J. Oper. Manag. 25 (2), 420–437 (2007). https://doi.org/10.1016/j.jom.2006.04.001
Sales-Coll, M., de Castro, R., Hueto-Madrid, J.A.: Improving operating room efficiency using lean management tools. Prod. Plan. Control 1–14 (2021). https://doi.org/10.1080/09537287.2021.1998932
Matos, I.A., Alves, A.C., Tereso, A.P.: Lean principles in an operating room environment: an action research study. J. Health Manag. 18 (2), 239–2577 (2016)
Portioli-Staudacher, A.: Lean healthcare. An experience in Italy. In: Koch, T. (ed.) APMS 2006. ITIFIP, vol. 257, pp. 485–492. Springer, Boston, MA (2008). https://doi.org/10.1007/978-0-387-77249-3_50
Rosa, A., Marolla, G., Lega, F., et al.: Lean adoption in hospitals: the role of contextual factors and introduction strategy. BMC Health Serv. Res. 21 , 889 (2021). https://doi.org/10.1186/s12913-021-06885-4
Rosa, C., Silva, F.J.G., Ferreira, L.P., Campilho, R.D.S.G.: SMED methodology: the reduction of setup times for Steel Wire-Rope assembly lines in the automotive industry. Procedia Manuf. 13 , 1034–1042 (2017)
Shah, R., Ward, P.T.: Lean manufacturing: context, practice bundles, and performance. J. Oper. Manag. 21 (2), 129–149 (2003)
Sunder, M.V., Mahalingam, S., Krishna, M.S.N.: Improving patients’ satisfaction in a mobile hospital using Lean Six Sigma – a design-thinking intervention. Prod. Plan. Control 31 (6), 512–526 (2020)
Torri, M., Kundu, K., Frecassetti, S., Rossini, M.: Implementation of Lean in IT SME company: an Italian case. Int. J. Lean Six Sigma (2021)
Google Scholar
Welsh, I., Lyons, C.M.: Evidence-based care and the case for intuition and tacit knowledge in clinical assessment and decision making in mental health nursing practice: an empirical contribution to the debate. J. Psychiatr. Ment. Health Nurs. 8 (4), 299–305 (2001)
Yin, R.K.: Case Study Research and Applications: Design and Methods, 6th edn. Sage, Los Angeles (2018)
Download references
Author information
Authors and affiliations.
Politecnico di Milano, Department of Management, Economics and Industrial Engineering, Milano, Italy
Stefano Frecassetti, Matteo Ferrazzi & Alberto Portioli-Staudacher
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Stefano Frecassetti .
Editor information
Editors and affiliations.
University of Galway, Galway, Ireland
Olivia McDermott
LUM University "Giuseppe Degennaro", Casamassima, Italy
Angelo Rosa
Instituto Superior de Engenharia do Porto, Porto, Portugal
José Carlos Sá
Aidan Toner
Rights and permissions
Reprints and permissions
Copyright information
© 2023 IFIP International Federation for Information Processing
About this paper
Cite this paper.
Frecassetti, S., Ferrazzi, M., Portioli-Staudacher, A. (2023). A Lean Approach for Reducing Downtimes in Healthcare: A Case Study. In: McDermott, O., Rosa, A., Sá, J.C., Toner, A. (eds) Lean, Green and Sustainability. ELEC 2022. IFIP Advances in Information and Communication Technology, vol 668. Springer, Cham. https://doi.org/10.1007/978-3-031-25741-4_8
Download citation
DOI : https://doi.org/10.1007/978-3-031-25741-4_8
Published : 12 February 2023
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-25740-7
Online ISBN : 978-3-031-25741-4
eBook Packages : Computer Science Computer Science (R0)
Share this paper
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
Societies and partnerships

- Find a journal
- Track your research
- Open access
- Published: 06 June 2024
Multi-stage optimization strategy based on contextual analysis to create M-health components for case management model in breast cancer transitional care: the CMBM study as an example
- Hong Chengang 1 ,
- Wang Liping 1 ,
- Wang Shujin 1 ,
- Chen Chen 1 ,
- Yang Jiayue 1 ,
- Lu Jingjing 1 ,
- Hua Shujie 1 ,
- Wu Jieming 1 ,
- Yao Liyan 1 ,
- Zeng Ni 1 ,
- Chu Jinhui 1 &
- Sun Jiaqi 1
BMC Nursing volume 23 , Article number: 385 ( 2024 ) Cite this article
Metrics details
None of the early M-Health applications are designed for case management care services. This study aims to describe the process of developing a M-health component for the case management model in breast cancer transitional care and to highlight methods for solving the common obstacles faced during the application of M-health nursing service.
We followed a four-step process: (a) Forming a cross-functional interdisciplinary development team containing two sub-teams, one for content development and the other for software development. (b) Applying self-management theory as the theoretical framework to develop the M-health application, using contextual analysis to gain a comprehensive understanding of the case management needs of oncology nursing specialists and the supportive care needs of out-of-hospital breast cancer patients. We validated the preliminary concepts of the framework and functionality of the M-health application through multiple interdisciplinary team discussions. (c) Adopting a multi-stage optimization strategy consisting of three progressive stages: screening, refining, and confirmation to develop and continually improve the WeChat mini-programs. (d) Following the user-centered principle throughout the development process and involving oncology nursing specialists and breast cancer patients at every stage.
Through a continuous, iterative development process and rigorous testing, we have developed patient-end and nurse-end program for breast cancer case management. The patient-end program contains four functional modules: “Information”, “Interaction”, “Management”, and “My”, while the nurse-end program includes three functional modules: “Consultation”, “Management”, and “My”. The patient-end program scored 78.75 on the System Usability Scale and showed a 100% task passing rate, indicating that the programs were easy to use.
Conclusions
Based on the contextual analysis, multi-stage optimization strategy, and interdisciplinary team work, a WeChat mini-program has been developed tailored to the requirements of the nurses and patients. This approach leverages the expertise of professionals from multiple disciplines to create effective and evidence-based solutions that can improve patient outcomes and quality of care.
Peer Review reports
Female breast cancer is the second leading cause of global cancer incidence in 2022, with an estimated 2.3 million new cases, representing 11.6% of all cancer cases [ 1 ]. Due to surgical trauma, side effects of drugs, fear of the recurrence or metastasis of breast cancer, changes in female characteristics, and lack of knowledge, patients with breast cancer frequently experience a series of physical and psychological health problems [ 2 , 3 , 4 , 5 , 6 ]. These health problems seriously affected patients’ life and work [ 7 , 8 ]. At present, community nursing in China is still in the developing stage, and the oncology specialty nursing service capacity of community nurses is not enough to deal with the health problems of breast cancer patients. It made continuous care for out-of-hospital breast cancer patients a weak link in the Chinese oncology nursing service system.
Nowadays, case management is employed to manage health problems for out-of-hospital breast cancer patients worldwide [ 9 , 10 , 11 , 12 , 13 , 14 , 15 ]. Case management involves regular telephone follow-ups and home visits by case management nurses to provide educational support to patients, thereby ensuring uninterrupted continuity of care [ 16 , 17 ]. The home visits and organization of patient information required for case management tasks consume a significant amount of time, manpower, and material resources [ 17 ]. In China, case management services are primarily undertaken by oncology nursing specialists from tertiary hospitals in their spare time [ 18 ]. However, the shortage of nurses has consistently been one of the major challenges facing the nursing industry in China, especially in tertiary hospitals [ 19 ]. Consequently, the implementation and promotion of case management in China also face great difficulties in reality [ 20 ].
The Global Observatory for eHealth (GOe) of the World Health Organization (WHO) defines mobile health (M-Health) as “medical and public health practice supported by mobile devices, such as mobile phones, patient monitoring devices, personal digital assistants (PDAs), and other wireless devices” [ 21 , 22 ]. With the development of digital technology and the COVID-19 pandemic in 2019, M-Health applications were further integrated into healthcare services, which increased the demand for M-Health applications in turn [ 23 , 24 ]. Compared with the traditional health service model, M-Health service model has the advantages of high-level informatization, fast response speed, freedom from time and location constraints, and resource-saving, etc. In the context of limited nursing human resources, M-Health service provides a new solution for the case management of out-of-hospital breast cancer patients [ 23 , 25 , 26 ].
Researchers have developed a range of M-Health applications targeting breast cancer patients. To our knowledge, none of these developed M-Health applications are designed for case management nursing services.
Early M-Health applications were mostly designed for single interventional goals, such as health education, medication compliance, self-monitoring, etc. Larsen et al. applied a M-Health application to monitor and adjust the dosage of oral chemotherapy drugs in breast cancer patients, and the results suggested that the treatment adherence was effectively improved [ 27 ]. Heo and his team successfully promoted self-breast-examination behavior in women under 30 years old using a M-Health application [ 28 ]. Mccarrol carried out a M-Health diet and exercise intervention in overweight breast cancer patients and found that the weight, BMI, and waist circumference of the intervention group decreased after one month [ 29 ]. Smith’s team found that their application promoted the adoption of healthy diet and exercise behaviors among breast cancer patients [ 30 ]. The application designed by Eden et al. enhanced the ability of breast cancer patients receiving chemotherapy to recognize adverse drug reactions [ 31 ]. Keohane and colleagues designed a health educational application based on the best practices and it proved effective in improving breast cancer-related knowledge [ 32 ]. The guideline-based M-Health application developed by Eden et al. optimized breast cancer patients’ individualized health decision-making regarding mammography [ 33 ].
With the progress of computer technology and the emphasis on physical and mental rehabilitation of breast cancer patients, some universities [ 34 , 35 ] in China have separately developed M-Health applications for comprehensive health management, which provide access to online communication, health education, and expert consultation.
Analyzing these developed applications deeply, three factors could be found that hindered the promotion of applications in real life. Firstly, the developing procedure usually lacks contextual analysis based on the actual usage context during the design phase. Secondly, there is a lack of consistent and long-term monitoring and operation staff in the subsequent program implementation. These factors may be the main reasons why many M-Health applications face difficulties in promotion and continuous operation after the research phase. Furthermore, as applications need to be installed on patients’ smartphones, certain hardware requirements, such as memory, may also pose restrict the adoption of M-Health applications to some extent.
In order to meet the needs of supportive care for out-of-hospital breast cancer patients and the needs of case management for oncology nurse specialists, we formed a multidisciplinary research team and collaboratively developed a WeChat mini-program for breast cancer case management in the CMBM (M-health for case management model in breast cancer transitional care) project. WeChat is chosen as the program development platform based on the following considerations. Firstly, WeChat is the most popular and widely used social software in China. As of December 31, 2020, the monthly active users of WeChat have exceeded 1.2 billion, and the daily active users of WeChat mini-programs exceeded 450 million [ 36 ]. Secondly, users can access and use the services of the mini-program directly within the WeChat platform, without the need to download or install additional mobile applications. This reduces the hardware requirements for software applications. The above two factors allow for a positive user experience and a realistic foundation for software promotion.
The purpose of this study is to describe the process of developing a tailored M-health component for the case management model in breast cancer transitional care and to highlight methods for solving the common obstacles faced during the application of M-health nursing service.
Methods and results
The development process was conducted in four steps: (a) An interdisciplinary development team was formed, consisting of two sub-teams dedicated to content and software development. (b) Using the self-management theory as the theoretical framework, contextual analysis was used to understand the case management needs of oncology nursing specialists and the supportive care needs of out-of-hospital breast cancer patients. Through iterative discussion within the interdisciplinary team, the preliminary conception of the application framework and function was formed. (c) A multi-stage optimization strategy was adopted to develop and regularly update the WeChat mini-programs, including three stages (screening, refining, and confirming). (d) During the entire development process, a user-centered principle was followed with the involvement of oncology nursing specialists and breast cancer patients, including development, testing, and iterative development phases.
The interdisciplinary team
An important prerequisite for developing M-health applications is the formation of an interdisciplinary development team. We built a multidisciplinary team consisting of researchers, oncology nursing specialists, and software developers. Each team member brought their expertise from their respective fields, and all individuals were considered members of the same team rather than separate participants with a common goal.
Two sub-teams were established, one responsible for content development, and the other for software development. The content development team consisted of researchers and six senior breast oncology nursing specialists with bachelor’s degrees and over 10 years of clinical experience. Their work included contextual analysis, functional framework design, and content review of the “Information” module. The software development team included researchers and experienced software developers. Their tasks involved developing the mini-program based on the functional framework and requirements designed by the content development team.
The development team used contextual analysis to identify the actual usage needs of two target groups for the mini-program: oncologist nurse specialists and out-of-hospital breast cancer patients.
Involvement of oncology nursing specialists and breast cancer patients following user-centered design principle
Since the oncology nursing specialists and breast cancer patients are targeted users of the mini-program, the two groups fully participated in the development according to the user-centered principle. Nursing specialists who in charge of case management were interviewed about the preliminary functional framework of the mini-program. The interview results are presented in the section “Driving the Development Process via the Contextual Analysis Findings.” Semi-structured in-depth interviews were conducted in the testing and iteration stage to gain user feedback from nursing specialists to improve the applicability and usability of the mini-program. The interview guide can be found in the supplementary material.
Breast cancer patients fully engaged in the three developing phases (Screening, Refining, and Confirming). In the Screening Phase, since the self-management theory was selected as the theoretical framework, the supportive care needs of out-of-hospital breast cancer patients were explored, and the functional framework of the mini-program was constructed accordingly. In the Refining Phase, patients were invited to evaluate the usability and practicality of the mini-program through system tests and semi-structured in-depth interviews. The results of the system test are presented in the Results of System Test section. The feedback from interviews and corresponding iterative updates are listed in Table 1 . In the Confirming Phase, our research team is conducting clinical trials in out-of-hospital breast cancer patients to find out the actual effect of the mini-program on recovery.
The theory framework of the mini-program
This study applied the self-management theory [ 37 ] as the theoretical framework. The self-management theory explains how individual factors and environmental factors influence an individual’s self-efficacy, which ultimately affects the generation and development of individual behaviors. Self-efficacy is influenced by direct experience, indirect learning, verbal persuasion, and psychological arousal. By providing individuals with sufficient knowledge, healthy beliefs, skills, and support, their self-efficacy is increased, and they are likely to engage in beneficial health behaviors and self-management. Individuals who are confident in their abilities to apply self-management behaviors and overcome obstacles by improving their self-management skills and persevere in their efforts to manage their health [ 37 ]. Self-efficacy is directly and linearly positively related to the active adoption of health management behaviors [ 38 ]. The functions of the various parts of the mini-program designed using self-management theory can broaden the pathways and levels of efficacy information generation in four ways: direct experience, indirect learning, verbal persuasion, and mental arousal. Patients with high self-efficacy will take positive steps to achieve desired goals and possess disease-adapted behaviors. The form of the mini-application function block diagram is shown in Fig. 1 .
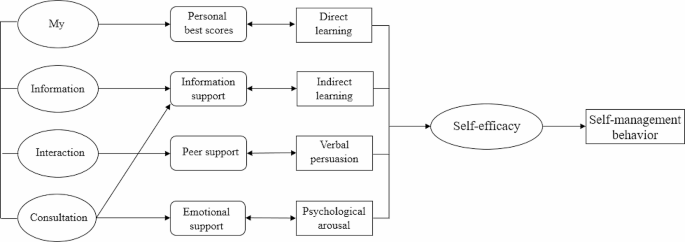
Driving the development process via the contextual analysis findings
Contextual analysis [ 39 ] is a method of discerning the profound significance and influence of language, behavior, events, and so forth, by examining them within a particular environment or background. Rather than being an afterthought, contextual analysis sheds light on the meaning and inner dynamics of our primary subject of interest. Through contextual analysis, we can gain a deeper understanding of the user’s usage scenarios, including their motivations, goals, environment, and behavior. This helps us better understand user needs, as well as the problems and challenges they may encounter when using the software.
In this paper, we adopted contextual analysis to gain a detailed understanding of the needs of oncology nurse specialists and out-of-hospital breast cancer patients. The research team adopted a mixed research strategy to achieve contextual analysis of the target users. A cross-sectional study was conducted among 286 patients and qualitative semi-structured in-depth interviews were applied in 12 patients to find out the supportive care needs of out-of-hospital breast cancer patients. According to the contextual analysis results from patients, the functional framework of the mini-program was constructed. See Fig. 2 for details.
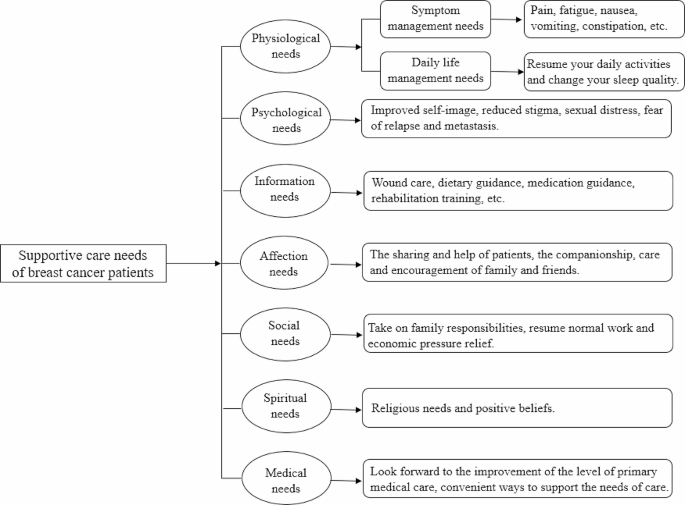
Supportive care needs of out-of-hospital breast cancer patients
Contextual analysis of breast cancer case management nurses was conducted through focus group interview. The interview results were listed as three themes: health information, personal self-management, and case management needs. Health information included breast cancer-related knowledge, the side effects of chemotherapy drugs, and symptom management measures. The key task of personal self-management contained temperature monitoring, weight management, functional exercise, and symptom management. Case management needs involved storage and management of patients’ medical records and development of a nurse-end program.
Based on the contextual analysis results of out-of-hospital breast cancer patients and the oncology case management nurses, the framework and functional block of the mini-program were formed. An overview of the CMBM Software development process is listed in Fig. 3 .
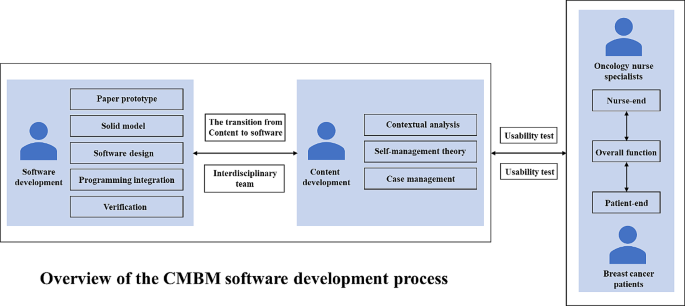
Overview of the CMBM software development process
Patient-end program functional modules
Using the results of the contextual analysis, we design the functional modules of the patient-end program based on the patient’s supportive care needs. For example, the “Information” section is designed to meet the “Information need” of breast cancer patients; the “social needs” and “spiritual needs” of patients suggest that breast cancer patients lack peer support, and for this reason, the"Interaction” section for patients has been added to the app to provide a communication platform for patients.
The patient-end program include four functional modules: “Information”, “Interaction”, “Management” and “My”. In the “Information” module, information about breast cancer treatment and health management are compiled based on clinical guildlines. The “Interaction” module allows patients to interact with fellow patients and consult an case management nurse. In the “Management” module, patients can record and review their self-management-related health status, including three medical parameters (temperature, blood pressure, weight) and three behavioral parameters (daily steps, medication, mindfulness excersice). The “My” module enables patients to input and edit their basic personal information and medical history. The main structure and information support module contents are listed in Fig. 4 .
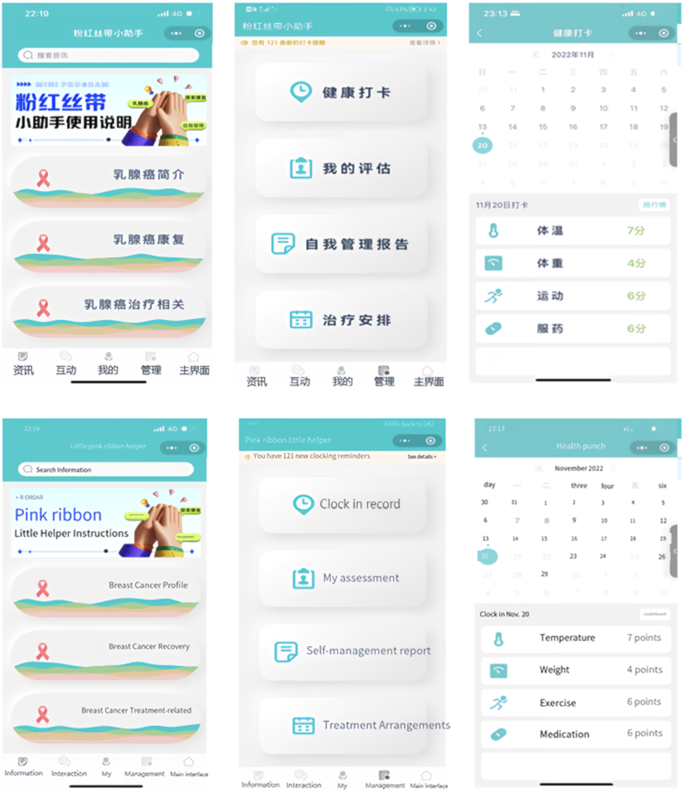
The main menu of patient-end program
Nurse-end program functional modules
The design of the functional modules of the nurse-end program was also derived from the results of contextual analyses. The nurse-end program includes three functional modules: “Consultation”, “Management”, and “My”. The “Consultation” module is mainly used for online communication between case management nurses and patients. Nurses can enter the patient’s name in the search box to open a dialog box, and communicate with each other by sending text, voice and pictures. In the “Management” module, nurses can effortlessly search for patients by entering their name, WeChat nickname, or mobile phone number in the search box. This initiates a seamless dialogue, and with a simple click of the “+” button, patients can be promptly added to the “My Concerns” list. They can view the medical record information on its homepage, and add the postoperative treatment plan for the patient. The “self-management report” feature empowers nurses to stay up-to-date with patients’ recent well-being. By monitoring vital indicators like temperature, weight, and incidents of nausea or vomiting following chemotherapy, nurses can proactively ensure patients’ safety. The “clock in record” feature meticulously logs various patient activities including weight variations, exercise regimens, and medication adherence, providing a holistic view of their health journey. “Treatment monitoring Schedule” enables nurses to create customized chemotherapy schedules. With the first postoperative chemotherapy session scheduled in the calendar, the system seamlessly computes subsequent chemotherapy sessions and associated assessments. This transition to an online system marks a significant advancement from the traditional paper-based chemotherapy planning. Its automated scheduling and data tracking functions serve to alleviate the clinical nursing workload, enhancing efficiency and freeing up valuable time for focused patient care. The “My” module offers nurses the convenience of adding patients of interest or relevant content to their “My Favorites” section, enabling streamlined one-click access for viewing and management. The core structure and informational components of this module are outlined in Fig. 5 .
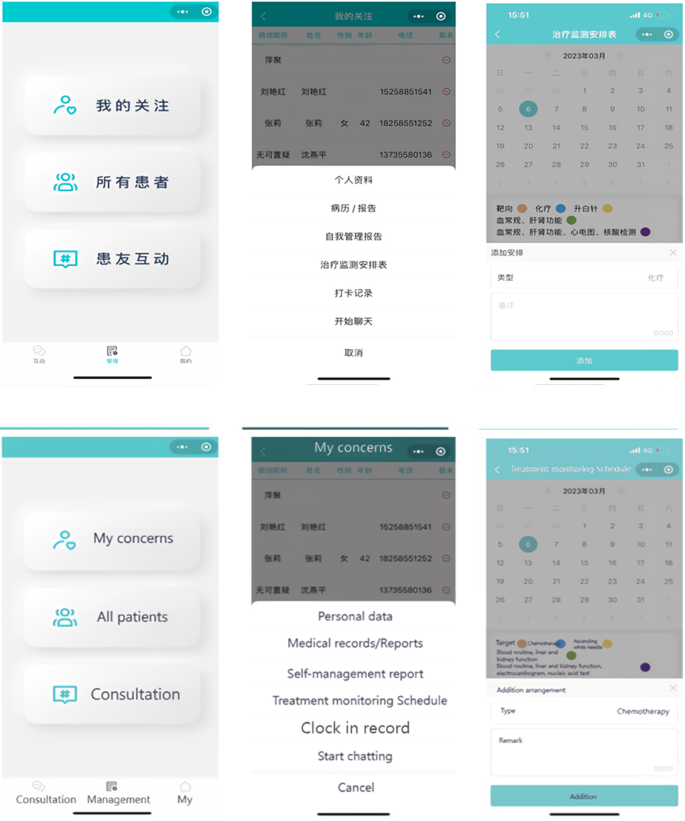
The main menu of nurse-end program
Driving the development process via the multi-stage optimization strategy
We adopted a multi-phase optimization strategy to drive the software development process. This strategy was proposed by Collins in 2005 and has become an important guiding theory for the development and evaluation of M-health interventions in recent years [ 40 ]. The strategy consists of three phases: Screening Phase, Refining Phase, and Confirming Phase. The Screening Phase need theories to identify and incorporate intervention elements. In this study, the initial version (1.0) development was based on self-management theory. Focusing on self-management, the results of contextual analysis, literature review and expert consultation were combined to design the mini-program version (1.0). The Refining Phase involves iterative adjustments to the previously version. In this study, the development team iteratively adjusted the mini-program version (1.0) according to users’ suggestions and test results. The Confirming Phase includes planning for clinical trials to test effect of the mini-program version (2.0) on self-management and recovery outcomes in out-of-hospital breast cancer patients.
Results of system test
Eight out-of-hospital breast cancer patients were recruited for system tests. The patient’s general information is listed in Table 2 .
The 10-item System Availability Scale (SUS)developed by Brooke was used [ 41 ]. The scale is a widely used method for quantitatively assessing user satisfaction with software systems. SUS is a Likert-5 and 10-item questionnaire (4 = strongly agree, 0 = strongly disagree), with Cronbach Alpha of 0.91. Generally, a system score above 60 on the SUS scale could be considered to be easy and simple to use, and the average score of SUS in our research is 78.75. The SUS scores of the mini-program system are presented in Fig. 6 .
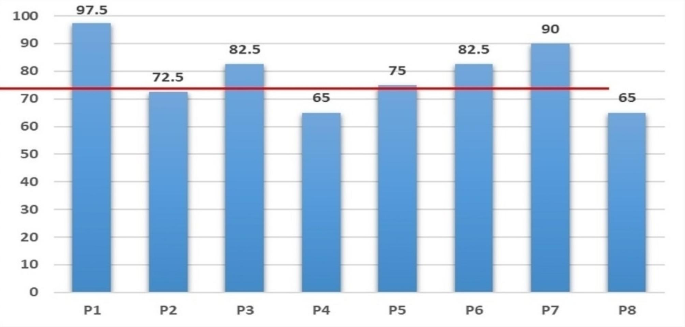
System availability scale (SUS) score of patients
The research team designed the core task tests based on the typical and necessary self-management tasks of out-of-hospital patients. The core task of the “Information” module was listed as an example (Table 3 ). Functional tests include the passing rate for each task, and performance tests include the completion time of each task. More details can be found in Table 4 .
In this article, we demonstrated how to create a customized software solution for breast cancer case management practices based on a multi-stage optimization strategy, applied the contextual analysis method, and followed the user-centered principle. Preliminary test results showed satisfaction and acceptance of the WeChat mini-program among both out-of-hospital breast cancer patients and oncology nursing specialists.
Team effort
There were two typical patterns for developing M-health applications in the past. One was led by software developers, while the other was led by medical professionals. Each of these patterns has its own advantages and disadvantages. To overcome these shortcomings, some projects [ 42 ] developing M-health applications are now utilizing interdisciplinary team collaborations. This approach not only ensures the quality of the software but also makes sure that applications meet the actual needs.
In order to develop a customized software solution, our research team consisted of researchers, oncology nursing specialists, and software developers. The interdisciplinary team work dedicated to customizing software solutions together. Our team members each played to their strengths and held regular meetings to discuss and enhance our understanding and resolution of issues encountered during the software development process. Our team also included informal members: breast cancer patients, whose suggestions contributed to the practicality of the program.
Contextual analysis and user-centered design
Contextual analysis is a valuable tool that enables developers to design systems that are more relevant and user-friendly. And it allows us to understand any context-specific characteristics, practice patterns, and the openness of the target setting’s nurses and patients towards technology [ 42 ]. User-centered design can significantly reduce the cost of program iteration. More importantly, it has a profound influence on various aspects of a program including its design, functionality, information architecture, and interactive elements [ 43 ]. By analyzing different contexts, not only did we design features that better meet user needs, but we also predicted and addressed potential issues that users may encounter when using the mini-program in advance, thereby enhancing the user experience. In the iterative development stage, we discovered and improved some deficiencies in the design through core task testing and usability testing. Notably, the completion rate of the core task test reached 100%, indicating that our application is user-friendly and easy to operate.
- Multi-stage optimization strategy
In several priority areas of public health, researchers have successfully applied multi-stage optimization strategies to enhance their work, including software development and intervention programs [ 44 , 45 , 46 ]. In this study, we also apply this strategy to software development. While the multi-stage optimization strategy provides an optimization framework, it is important to note that our optimization objectives (such as software functionality and content requirements) are determined by key users involved in the research (out-of-hospital breast cancer patients and oncology nurse spescialists). This project adopts a multi-stage optimization strategy, iteratively improving the development of the mini-program through screening, refinement, and confirmation stages. Each stage aims to optimize our program.
The research team plans to explore the feasibility of mini program development program through preliminary experiment, and verify the intervention effect of mini program on self-management behavior, self-efficacy and quality of life and other indicators through formal experiment. A randomized controlled trial (IRB-2020-408) was initiated in August 2022 at a Class III hospital in Zhejiang, China, and is currently in the data collection phase.
There is no doubt that M-health will play a core role in the future of health care. However, to successfully implement and promote M-health applications in clinical setting, it is essential to analyze the needs of the target population. Additionally, it is crucial to determine who will be the driving force behind the implementation of the entire M-health project. This study demonstrates how to integrate M-health components into existing breast cancer case management care practices. In addition to providing a reference for other teams interested in developing and integrating M-health components into case management care models, this study also provides a reference for building M-health-featured care work models in practices.
In this study, the collaborative work of an interdisciplinary team with backgrounds in nursing and computer science, along with the active involvement of patients, not only facilitated the planning, developing, updating, and testing of M-health components based on the actual needs of the target population, but also increased the chances of acceptance and long-term implementation of the M-health program in practice.
This study demonstrates how to integrate M-health components into existing breast cancer case management practices. It provides insights for other reserch teams interested in developing and integrating M-health components into daily nursingt practice.
In the context of the digital age, M-health applications are rapidly becoming information sources and decision support tools for healthcare professionals and patients. However, it is crucial not to overlook the issues of information security and digital barriers for older adults.
Through interviews with outpatients with breast cancer and oncology nurses, we have gained insights into their concerns regarding information security. Some interviewees expressed concerns about information security and were worried about the risk of their personal information being leaked during app usage. Such concerns, to some extent, hinder the widespread adoption of M-health applications. Additionally, some interviewees mentioned that older patients, in general, find it challenging to learn and use the various functions of WeChat mini-programs, making it difficult to promote and apply M-health applications among the elderly population.
Solving these issues effectively is not only vital for the patients’ rights and interests but also crucial for the comprehensive implementation of M-health in practice. It is a matter that requires careful consideration in future development of M-health applications.
Data availability
The datasets generated and/or analysed during the current study are not publicly available but are available from the corresponding author on reasonable request.
Bray F, Laversanne M, Sung H et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2024: 1–35.
Wu J, Zeng N, Wang L, Yao L. The stigma in patients with breast cancer: a concept analysis. Asia Pac J Oncol Nurs. 2023;10(10):100293.
Article PubMed PubMed Central Google Scholar
Heidkamp P, Hiltrop K, Breidenbach C, Kowalski C, Pfaff H, Geiser F, Ernstmann N. Coping with breast cancer during medical and occupational rehabilitation: a qualitative study of strategies and contextual factors. BMC Womens Health. 2024;24(1):183.
Zhao H, Li X, Zhou C, Wu Y, Li W, Chen L. Psychological distress among Chinese patients with breast cancer undergoing chemotherapy: concordance between patient and family caregiver reports. J Adv Nurs. 2022;78(3):750–64.
Article PubMed Google Scholar
Jang Y, Seong M, Sok S. Influence of body image on quality of life in breast cancer patients undergoing breast reconstruction: Mediating of self-esteem. J Clin Nurs. 2023;32(17–18):6366–73.
Oh PJ, Cho JR. Changes in fatigue, psychological distress, and Quality of Life after Chemotherapy in women with breast Cancer: a prospective study. Cancer Nurs. 2020 Jan/Feb;43(1):E54–60.
Maass SWMC, Boerman LM, Verhaak PFM, Du J, de Bock GH, Berendsen AJ. Long-term psychological distress in breast cancer survivors and their matched controls: a cross-sectional study. Maturitas. 2019;130:6–12.
Article CAS PubMed Google Scholar
De Vrieze T, Nevelsteen I, Thomis S, De Groef A, Tjalma WAA, Gebruers N, Devoogdt N. What are the economic burden and costs associated with the treatment of breast cancer-related lymphoedema? A systematic review. Support Care Cancer. 2020;28(2):439–49.
Liang Y, Gao Y, Yin G, Chen W, Gan X. Development of a breast cancer case management information platform (BC-CMIP) module based on patient-perceived value. Front Oncol. 2022;12:1034171.
Jin L, Zhao Y, Wang P, Zhu R, Bai J, Li J, Jia X, Wang Z. Efficacy of the whole-course case management model on compliance and satisfaction of breast Cancer patients with whole-course standardized treatment. J Oncol. 2022;2022:2003324.
Scherz N, Bachmann-Mettler I, Chmiel C, Senn O, Boss N, Bardheci K, Rosemann T. Case management to increase quality of life after cancer treatment: a randomized controlled trial. BMC Cancer. 2017;17(1):223.
Yamei Y, Yongfang Zh J, Sh, Xixi C, Dehong Z, Chuner J, Jianfen N. The influence of the whole course professional nursing case management model on the disease uncertainty for breast cancer patients with chemotherapy. J Nur Train. 2018;(02), 99–111.
Cuie P. The whole case management model for breast cancer patients to study the effect of quality of life and psychological society. Hunan Normal University; 2015.
Bleich C, Büscher C, Melchior H, Grochocka A, Thorenz A, Schulz H, Koch U, Watzke B. Effectiveness of case management as a cross-sectoral healthcare provision for women with breast cancer. Psycho Oncol. 2017;26(3):354–60.
Article Google Scholar
Huiting Zh J, Zh, Xiaodan W, Lijuan Zh, Wenhao H, Huiying Q. Exploration of case management model for breast cancer patients. J Nurs Sci. 2017;(14), 19–21.
Woodward J, Rice E. Case management. Nurs Clin North Am. 2015;50(1):109–21.
Luo X, Chen Y, Chen J, Zhang Y, Li M, Xiong C, Yan J. Effectiveness of mobile health-based self-management interventions in breast cancer patients: a meta-analysis. Support Care Cancer. 2022;30(3):2853–76.
Meiqin X, Lingjuan Z. The delivery and inspiration of case management model in China. Chin J Nurs. 2014;(03), 367–71.
Huanhuan L, Zhuangjie X, Yuan L, Ying L, ShouQi W, MeiLing Z, Jie Y, Pengcheng L, Huanhuan Zh, Jiao S. A review of the interventions of nurses’ intent to stay. Chin J Nurs. 2017;(08), 1007–9.
Dan W, Shanling L, Yulin X. Research status of continuous nursing at home and abroad. Nurs Res 2016;(20), 2436–8.
Mariani AW, Pêgo-Fernandes PM. Telemedicine: a technological revolution. Sao Paulo Med J. 2012;130(5):277–8.
Hamine S, Gerth-Guyette E, Faulx D, Green BB, Ginsburg AS. Impact of mHealth chronic disease management on treatment adherence and patient outcomes: a systematic review. J Med Internet Res. 2015;17(2):e52.
Mahmood S, Hasan K, Colder Carras M, Labrique A. Global preparedness against COVID-19: we must leverage the Power of Digital Health. JMIR Public Health Surveill. 2020;6(2):e18980.
Petracca F, Ciani O, Cucciniello M, Tarricone R. Harnessing Digital Health Technologies during and after the COVID-19 pandemic: context matters. J Med Internet Res. 2020;22(12):e21815.
Cong H, Yongyi C, Xiangyu C, Xuying L. Rehabilitation Effect of Chemotherapy-based adverse reactions to breast Cancer patients based on continuous care platform. Oncol Pharma. 2020;(02), 244–51.
Cong A, Liping W. Application progress of mobile health in transitional care of patients with hypertension. Chin J Mod Nurs. 2021;27(4):539–42.
Google Scholar
Larsen ME, Farmer A, Weaver A, Young A, Tarassenko L. Mobile health for drug dose optimisation. Annu Int Conf IEEE Eng Med Biol Soc. 2011;2011:1540–3.
PubMed Google Scholar
Heo J, Chun M, Lee KY, Oh YT, Noh OK, Park RW. Effects of a smartphone application on breast self-examination: a feasibility study. Healthc Inf Res. 2013;19(4):250–60.
McCarroll ML, Armbruster S, Pohle-Krauza RJ, Lyzen AM, Min S, Nash DW, Roulette GD, Andrews SJ, von Gruenigen VE. Feasibility of a lifestyle intervention for overweight/obese endometrial and breast cancer survivors using an interactive mobile application. Gynecol Oncol. 2015;137(3):508–15.
Smith SA, Whitehead MS, Sheats J, Mastromonico J, Yoo W, Coughlin SS. A Community-Engaged Approach to developing a Mobile Cancer Prevention App: the mCPA Study Protocol. JMIR Res Protoc. 2016;5(1):e34.
Eden KB, Ivlev I, Bensching KL, Franta G, Hersh AR, Case J, Fu R, Nelson HD. Use of an online breast Cancer Risk Assessment and patient decision aid in Primary Care practices. J Womens Health (Larchmt). 2020;29(6):763–9.
Keohane D, Lehane E, Rutherford E, Livingstone V, Kelly L, Kaimkhani S, O’Connell F, Redmond HP, Corrigan MA. Can an educational application increase risk perception accuracy amongst patients attending a high-risk breast cancer clinic? Breast. 2017;32:192–8.
Eden KB, Scariati P, Klein K, Watson L, Remiker M, Hribar M, Forro V, Michaels L, Nelson HD. Mammography decision aid reduces Decisional Conflict for women in their forties considering screening. J Womens Health (Larchmt). 2015;24(12):1013–20.
Zhu J, Ebert L, Liu X, Chan SW. A mobile application of breast cancer e-support program versus routine care in the treatment of Chinese women with breast cancer undergoing chemotherapy: study protocol for a randomized controlled trial. BMC Cancer. 2017;17(1):291.
Ying L. Construction of an M-Health based information support program for women with breast Cancer during diagnosis and treatment process. The Second Military Medical University; 2017.
Pengfei X, Bo Y, Yue H, Jingyun H. An empirical research on the interactive behavior of WeChat subscription number users from the perspective of the theory of interactive ritual chain. Chin J Inf Syst. 2023;(01), 69–83.
Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191Y215.
Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31(2):143Y164.
George A, Scott K, Garimella S, Mondal S, Ved R, Sheikh K. Anchoring contextual analysis in health policy and systems research: a narrative review of contextual factors influencing health committees in low and middle income countries. Soc Sci Med. 2015;133:159–67.
Collins LM, Murphy SA, Strecher V. The multiphase optimization strategy (MOST) and the sequential multiple assignment randomized trial (SMART): new methods for more potent eHealth interventions. Am J Prev Med. 2007;32(5 Suppl):S112–8.
Brooke JB. SUS: a quick and dirty usability scale. Usability Evaluation Ind. 1996;189(194):4–7.
Leppla L, Hobelsberger S, Rockstein D, Werlitz V, Pschenitza S, Heidegger P, De Geest S, Valenta S, Teynor A. SMILe study team. Implementation Science meets Software Development to create eHealth Components for an Integrated Care Model for allogeneic stem cell transplantation facilitated by eHealth: the SMILe Study as an Example. J Nurs Scholarsh. 2021;53(1):35–45.
Luna D, Quispe M, Gonzalez Z, Alemrares A, Risk M, Garcia Aurelio M, Otero C. User-centered design to develop clinical applications. Literature review. Stud Health Technol Inf. 2015;216:967.
Piper ME, Fiore MC, Smith SS, Fraser D, Bolt DM, Collins LM, Mermelstein R, Schlam TR, Cook JW, Jorenby DE, Loh WY, Baker TB. Identifying effective intervention components for smoking cessation: a factorial screening experiment. Addiction. 2016;111(1):129–41.
Spring B, Pfammatter AF, Marchese SH, Stump T, Pellegrini C, McFadden HG, Hedeker D, Siddique J, Jordan N, Collins LM. A factorial experiment to optimize remotely delivered behavioral treatment for obesity: results of the Opt-IN Study. Obes (Silver Spring). 2020;28(9):1652–62.
O’Hara KL, Knowles LM, Guastaferro K, Lyon AR. Human-centered design methods to achieve preparation phase goals in the multiphase optimization strategy framework. Implement Res Pract. 2022;3:26334895221131052.
PubMed PubMed Central Google Scholar
Download references
Acknowledgements
The authors would like to express our sincere gratitude to all the breast cancer patients who participated in this research.
This study was supported by the Zhejiang Provincial Natural Science Foundation of China (LY18H160061) and Funding for innovation and entrepreneurship of high-level overseas students in Hangzhou.
Author information
Authors and affiliations.
School of Nursing, Hangzhou Normal University, Hangzhou City, Zhejiang Province, 311100, China
Hong Chengang, Wang Liping, Wang Shujin, Chen Chen, Yang Jiayue, Lu Jingjing, Hua Shujie, Wu Jieming, Yao Liyan, Zeng Ni, Chu Jinhui & Sun Jiaqi
You can also search for this author in PubMed Google Scholar
Contributions
HCG conceived the entire paper framework and was responsible for writing the paper. WSJ and CC conducted all interviews and managed the mini-programs. YJY, LJJ and HSJ were responsible for the collection of clinical nurse data. CJH and SJQ were responsible for patient data collection. Data analysis was conducted by WJM, YLY and ZN. WLP was responsible for the revision, editing and approval of manuscripts. All authors have rigorously revised and edited successive drafts of the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Correspondence to Wang Liping .
Ethics declarations
Ethics approval and consent to participate.
The study was reviewed and approved by the Ethics Committee of ZheJiang Cancer Hospital (Ethic ID: ZJZLYY IRB-2020-408). All the participants signed written informed consent forms. This study was conducted in accordance with the 1964 Declaration of Helsinki guidelines.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Chengang, H., Liping, W., Shujin, W. et al. Multi-stage optimization strategy based on contextual analysis to create M-health components for case management model in breast cancer transitional care: the CMBM study as an example. BMC Nurs 23 , 385 (2024). https://doi.org/10.1186/s12912-024-02049-x
Download citation
Received : 22 November 2023
Accepted : 29 May 2024
Published : 06 June 2024
DOI : https://doi.org/10.1186/s12912-024-02049-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- User-centered design
- Contextual analysis
- Breast cancer patients
- Case management
- Transitional care
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
- Open access
- Published: 05 June 2024
A quality improvement study on how a simulation model can help decision making on organization of ICU wards
- Danielle Sent ORCID: orcid.org/0000-0002-4703-5345 1 , 2 ,
- Delanie M. van der Meulen ORCID: orcid.org/0000-0002-1678-2057 1 ,
- Andres Alban ORCID: orcid.org/0000-0002-9552-4039 3 ,
- Stephen E. Chick ORCID: orcid.org/0000-0002-8026-1571 4 ,
- Ilse J.A. Wissink ORCID: orcid.org/0000-0002-5551-9868 5 ,
- Alexander P.J. Vlaar ORCID: orcid.org/0000-0002-3453-7186 5 &
- Dave A. Dongelmans ORCID: orcid.org/0000-0001-8477-6671 5
BMC Health Services Research volume 24 , Article number: 708 ( 2024 ) Cite this article
10 Accesses
Metrics details
Intensive Care Unit (ICU) capacity management is essential to provide high-quality healthcare for critically ill patients. Yet, consensus on the most favorable ICU design is lacking, especially whether ICUs should deliver dedicated or non-dedicated care. The decision for dedicated or non-dedicated ICU design considers a trade-off in the degree of specialization for individual patient care and efficient use of resources for society. We aim to share insights of a model simulating capacity effects for different ICU designs. Upon request, this simulation model is available for other ICUs.
A discrete event simulation model was developed and used, to study the hypothetical performance of a large University Hospital ICU on occupancy, rejection, and rescheduling rates for a dedicated and non-dedicated ICU design in four different scenarios. These scenarios either simulate the base-case situation of the local ICU, varying bed capacity levels, potential effects of reduced length of stay for a dedicated design and unexpected increased inflow of unplanned patients.
The simulation model provided insights to foresee effects of capacity choices that should be made. The non-dedicated ICU design outperformed the dedicated ICU design in terms of efficient use of scarce resources.
Conclusions
The choice to use dedicated ICUs does not only affect the clinical outcome, but also rejection- rescheduling and occupancy rates. Our analysis of a large university hospital demonstrates how such a model can support decision making on ICU design, in conjunction with other operation characteristics such as staffing and quality management.
Peer Review reports
Introduction
During the 1900s it became clear that clustering of the most critically ill patients was beneficial for their clinical outcomes [ 1 ]. As a result of these findings, Intensive Care Units (ICUs) were developed. At present the question has arisen to what degree clustering of ICU patients by their condition is beneficial for patients and society. In other words, whether a specialized ‘dedicated ICU’ is in favor of a ‘non-dedicated ICU’ with a mixed patient population [ 2 , 3 ]. According to literature, both designs have pros and cons, while strong evidence in favor of one of the two designs is lacking [ 4 , 5 , 6 ].
As a result of an ageing population, a continuous increase of healthcare expenditures and shortages in the available medical workforce, a supply-demand mismatch in ICU capacity has arisen in recent years [ 7 , 8 ]. The capacity strain resulting from this mismatch inevitably leads to increased rescheduling of elective ICU admissions, and to rejection of unplanned patients in need of critical care. To serve as many patients as possible and make efficient use of scarce labor and capital resources, unnecessary capacity loss resulting from unoccupied available beds should be minimized. This raises the question on the ideal ICU design. In this study the non-dedicated ICU refers to general pooling of resources in an ICU with a mixed patient population, and a dedicated ICU refers to an ICU design with specific wards for patients with similar conditions in which dedicated resources are available that are not shared with other wards. In the context of this paper ‘efficient’ is used for a design with as less rejections, rescheduling, and empty beds as possible. In a situation where resources are scarce it is important to be able to see the effects of choices that should be made. By providing a model we give insights into the effects on performance of various designs of ICUs. Based on the principals of pooling, a higher quantity of patients has access to ICU care in a non-dedicated design [ 9 ]. Besides, if certain specialisms regularly deal with long-stay patients, this quickly leads to stagnation of admissions and an increase in the number of cancellations in a dedicated design. However, all this only holds when lengths of ICU stays and other process metrics are otherwise the same for both designs.
According to some studies a dedicated-ICU is associated with lower mortality rates, shorter length of stay, shorter duration of intubation and less blood-stream-infections [ 2 , 10 , 11 , 12 , 13 ], whilst other studies were not able to confirm these findings [ 14 , 15 , 16 ]. One optimistic paper regarding dedicated ICU was from Mirski et al. which showed a dedicated ICU design to be related to a 25–45% reduced length of stay, resulting in reduced healthcare expenditures [ 13 ]. We still find the idea that a dedicated ICU could result in decreased length of ICU stay interesting and want to explore whether these effects could outweigh the efficiency of a non-dedicated ICU. Song et al. as well as Li et al. [ 17 , 18 ] suggest that behaviours might change in a dedicated ICU, for example in reducing rework or overhead associated with multi-tasking, or with greater sense of ownership, resulting in somewhat shorter length of stay and without loss of quality of care. There is a general trend towards decreased length-of-stay in hospitals has been observed in the past decades [ 19 ], and studies show the importance of admissions and discharge policies on ICU performance [ 18 ], where admission policy may include features of the likelihood a bed might be immediately available or alternatively a wait or a rerouting of patients might be required, or potentially a need to reschedule elective surgeries. Together, these and other studies suggest that technology and organization changes have roles to play in improving length of stay and quality of care. Taken together, it remains unclear whether a dedicated ICU results in improved outcomes for individual patients. If length of ICU stay and other process metrics do not outperform the efficiency of a non-dedicated design, a dedicated ICU is expected to lead to increased capacity strain which in itself is associated with deterioration in healthcare delivery, suboptimal patient outcomes and decreased job satisfaction among medical staff [ 7 ].
In this paper we aim to describe and use a simulation model to help ICU departments to visualize trade-offs between a dedicated and a non-dedicated ICU design. Department-specific characteristics can be imported in such a model to study performance of both designs in terms of bed occupancy, rejection, and rescheduling rates. Depending on local preferences, a model can be optimized for one of the performance measures, at the expense of other measures. In conjunction with other operation characteristics such as staffing and quality management, a simulation model can be useful to gain insights into the effects of decisions that should be made. Besides, models such as these can be utilized to reorganize the ICU department and manage expectations to staff and policy makers in case of abrupt changes in circumstances [ 20 ]. We did not also include a wait room, as did [ 21 ], because our application was motivated by COVID-19 response, where scenarios of capacity expansion, allocation of that capacity, and the potential need to reroute urgent patients to other facilities, space permitting, was more relevant, as well as the potential role of rescheduling elective procedures in support of urgent critical care needs. That said, the model’s scenario selection allows for an assessment for potential total bed capacity planning, as well as estimates of performance metrics for tradeoffs between allocating that capacity for specialisms versus having a non-dedicated design.
This paper followed the SQUIRE 2.0 guideline for reporting on quality improvement studies [ 22 ]. The ICU from which admission data are used in this paper, is a large academic hospital in the Netherlands housing a multidisciplinary non-dedicated ICU with a bed capacity of 28 beds divided over four units. INSEAD and Amsterdam UMC cooperated to create a base simulation model which enables to model the performance of a dedicated or non-dedicated design in hypothetical scenarios. It visualizes performance of both designs in terms of rescheduling, rejection, and bed occupancy rates.
Patient inflow data of the local non-dedicated ICU were used, and patients were labeled either as being planned or unplanned. Planned patients were defined as patients that arrived at the ICU via other medical wards in which they had a planned admission. Unplanned patients came straight from the emergency room or from other wards in emergency situations. Arrival, length of ICU stay, rejection, and rescheduling data were also obtained from the local ICU over the years 2015 ( N = 1881) and 2016 ( N = 2170). Out of those, 1,779 and 2,043 patients were admitted, and 102 and 127 patients were rejected, respectively. The overall average arriving patients per day was therefore 5.55. In total, 66% of all arrived patients (2,668 patients) were unplanned, and out of them 9% (229 patients) were rejected. Among all patients, 82% (3,117 patients) were admitted on weekdays and 18% (705 patients) were admitted on weekends. Only unplanned patients could be rejected, planned patients were rescheduled if necessary, and in our model the bed partition was, at the expense of rescheduling rates, optimized for rejection rates. Furthermore, all ICU patients were assigned to a medical specialism based on their diagnose on admission (CAPU = cardiopulmonary surgery, CARD = cardiology, INT = internal medicine, CHIR = surgery, NEC = neurosurgery or NEU = neurology or other). The simulation model was coded in R, and an online version is available at https://daniellesent.shinyapps.io/ICU-model/ . Parameters of the model were calibrated to hospital scheduling and LOS data for both planned and unplanned patients for each specialism, and bed capacity characteristics of the hospital. Since no association between arriving patients is expected, the arrival of the unplanned patients is assumed to be a Poisson process. The Poisson assumption was tested using the number of unplanned arrivals per day with a chi-squared test and find p -values of 0.42 and 0.39, respectively, not rejecting our assumption. The arrival process was estimated independently for weekday and weekend arrivals. The arrival of planned patients is follows a categorical distribution, where the probabilities are given by the fraction of days in the two-year period that a given number of patients arrived. The distribution family of the LOS was chosen using the tool Stat::FitTM. The simulation ran for a period of 3,770 days (approximately ten and a half years), where the first 120 days were burned-in to warm up the queue. The remaining ten years were use for evaluation purposes. The model was verified by checking several special cases of inputs to theoretical values provided by queueing theory. More in depth specifications of the model and it evaluation can be found in the article of Alban et al. [ 23 ].
For this study, we extended the base model to be able to run four clinically relevant scenarios that help decision-making on ICU design under varying hypothetical circumstances. First the base case model will be shown with a maximum capacity of 28 beds, the total number of beds that were available at the ICU of the hospital the data was obtained from. The base case model compares a dedicated with a non-dedicated ICU design. In this scenario the dedicated ICU is divided into four specialized units, based on the current infrastructure of the building. This structure uses a partition of six beds for unit CAPU, eleven beds for a combination unit of CARD/INT/Other, five beds for unit CHIR and six beds for a combination unit of NEC and NEU. This partition was found to be optimal for 28 beds in terms of all three performance measures. Yet, in practice bed capacity fluctuates due to specific circumstances such as workforce constraints, a pandemic or holidays either increasing or decreasing the number of beds available for patients. Therefore, a second model shows the performance for a dedicated and a non-dedicated ICU under varying bed capacities, to complement other studies of ICU dedicated versus flexible capacity [ 17 ], which may be influenced as well by patient mix [ 21 ]. A third scenario visualizes the situation in which a dedicated ICU design decreases length of ICU stay (LOS) in advance of a non-dedicated ICU, as was shown by Mirski et al. [ 13 ]. Finally, a scenario with an increased inflow of unplanned patients is simulated, motivated by the COVID pandemic in which the inflow increased dramatically. To do so, a new simulation population was created by decreasing the original inter-arrival rates. Taken together, the graphs may show the numbers of beds required in dedicated or non-dedicated settings in order to achieve a given threshold for metrics of interest, thereby presenting a guage with which to assess potential behavioural effects that might be active [ 18 ]. Ethical approval was not required, only anonymized data containing date and time of admission and (if applicable) departure and specialism were used for the model. No further patient data was used.
The simulation of the first scenario is shown in Fig. 1 and presents the base-case model with 28 beds for a non-dedicated and a dedicated ICU design in terms of a (occupancy), b (rejection) and c (rescheduling) rates.
Each measure is reported for the overall performance and for performance of the four different clinical diagnose groups (CAPU, CHIR, INT/CAR, NEU/NEC). As the general ICU is not divided into units, the values correspond to the performance specific to the cluster of patients assigned to the respective dedicated unit. The overall rejection rate for the non-dedicated ICU is 7.7% versus 18.1% for the dedicated ICU. The overall rescheduling rates are 13.0% versus 100.5% (meaning that some patients had to be rescheduled more than once). The overall occupancy rate lies lower in the dedicated ICU (75.1% versus 67.4% for non-dedicated and dedicated respectively). Note that the non-dedicated ICU has lower rejection and rescheduling rates despite the higher occupancy rate. The rescheduling simulation model shows a high standard error, which originates from the fact that the number of rescheduled patients per day is mostly very low, and binary (yes rescheduled or not rescheduled).

Comparison of the non-dedicated and dedicated ICU in terms of occupancy ( a ), rejection ( b ) and rescheduling ( c ) rates in base-case situation
Figure 2 shows the performance of a dedicated (a) and a non-dedicated (b) ICU with varying bed capacity, ranging from 14 to 50 beds. While the non-dedicated ICU starts out with a higher occupancy rate than the dedicated ICU (86.9% vs. 76.8%), both end up with a similar occupancy rate at the capacity of 50 beds (44.9% vs. 44.6%). Between the minimum and maximum bed capacity that we tested, the occupancy rate in the non-dedicated ICU is constantly higher than in the dedicated ICU. Note that for the dedicated ICU it is observed that at a capacity of 34, 37, 42 and 46 beds, the rescheduling rate drops. At these steps, the capacity for the specialism with most planned patients was increased with one bed, resulting in dropping of the rescheduling rate. For the non-dedicated ICU, the rejection rate and rescheduling rate both come close to their minimum around a bed capacity of 30 beds, while for the dedicated ICU this is seen at a bed capacity of 45 beds. The rescheduling rate is steadily higher than the rejection rate. The comparison of Fig. 2 a and b also allows for comparison of the minimum number of beds required to reach a rejection rate below 5%, which is a target in ICU organization management in the Netherlands [ 24 ]. In the non-dedicated ICU setting, 30 beds are required to meet this target, while in the dedicated ICU 38 beds would be needed. With a bed capacity of 30 beds, the non-dedicated ICU would have an average occupancy of 71.7%, while a bed capacity of 38 beds in the dedicated ICU leads to an average occupancy of 56.3%. The average rescheduling rates for this number of beds lie at 7.4% - and 39.4%, for the non-dedicated and dedicated ICU respectively.

Performance of a dedicated ( a ) and a non-dedicated ( b ) ICU with a varying bed capacity
Figure 3 shows a simulation of the dedicated ICU setting, where an average length of ICU stay (LOS) reduction is assumed. It demonstrates that in the dedicated ICU, bed occupancy rates decrease steadily as the average LOS becomes shorter. In the base-case situation, with no LOS reduction, the overall occupancy rate was 67.4% in the dedicated ICU, while at a hypothetical 30% LOS reduction it lies at 53.3%. With a hypothetical 30% reduction in LOS, rejection rates decrease to 7.5% and rescheduling rates decrease to 28.6%. As described in the first scenario, in the non-dedicated ICU setting the average rejection, rescheduling and occupancy rates were 7.7%, 13% and 75.1%, respectively.

Hypothetical lengths of stay reduction in a dedicated ICU design
The last scenario is shown in Fig. 4 for a non-dedicated design (a) and a dedicated design (b). In this scenario the simulation model ran for various increases (10%, 20% and 30%) of unplanned patients of each specialism. The 0% increase bar shows the results for the base-case patient inflow. In the non-dedicated ICU design the occupancy rates are 75.1%, 78.8% and 83.4% for a patient inflow of 0%, and an increase of unplanned patients of 10%, 20% and 30% respectively. In the dedicated ICU the occupancy remains lower with rates of 67.4%, 70.2%, 74.7% and 77.5% respectively. In the non-dedicated ICU setting the rejection rates (7.7%, 9.7%, 16.3% and 22.8%) and rescheduling rates (13%, 17.2%, 33.1% and 51.5%) increase gradually as the inflow of unplanned patients increases. In a dedicated ICU design the rejection rates are higher for the same increase in inflow, 18.1%, 21.3%, 27.9% and 34.0%, respectively. The rescheduling rates for 0, 10, 20 and 30% increase in unplanned patient inflow are 100.5%, 106.3%, 129.5% and 151.2% respectively, meaning that some patients will be rescheduled more than once.

Increase in unplanned patient inflow in a non-dedicated ( a ) and a dedicated ( b ) ICU design
This study aimed to provide insights in the capacity performance of a dedicated ICU in comparison with a non-dedicated ICU by using a discrete event simulation model. Previous literature shows no consensus on a preferred design [ 2 , 10 , 12 , 13 , 14 , 15 , 16 ]. However, it is known that organising a non-dedicated ICU has its challenges because effective management is amongst other factors depending on the establishment of continuous professional development, ensuring that all personnel is equipped to respond to the diverse needs characteristic of non-dedicated ICUs we note that our simulations do not answer the question of whether a non-dedicated ICU should or should not be preferred over a dedicated ICU. We quantify the performance, in terms of the number of rejected and rescheduled patients and the occupancy rate of the ICU’s. Our simulation model was developed using admission data of a large university hospital ICU in the Netherlands.
The first scenario showed that the non-dedicated ICU design dominates the dedicated ICU design in terms of occupancy, rejection, and rescheduling rates in the base-case scenario. The second scenario showed that the dedicated ICU needed eight more beds to accomplish a desired rejection rate below 5%, when compared to the non-dedicated ICU design. Yet, the model showed that scaling up with eight beds to a total of 38 beds in a dedicated design resulted in a bed occupancy rate of 56.3%, which can be seen as inefficient use of expensive and scarce ICU resources. The non-dedicated ICU should scale up with at least two more beds to be able to have a rejection rate below 5%, as is described in the national guidelines [ 24 ]. Figure 2 b shows that the rescheduling rates for the dedicated ICU remain high, up to a high number of available beds. This is likely because in our analysis the bed partition was optimized for rejection rates, clearly at the expense of rescheduling rates. The third scenario explored the theory that a dedicated ICU leads to a shorter average LOS due to the specialization of healthcare delivery as was shown by Mirski et al. in 2001 [ 13 ]. The simulation model showed that if a dedicated design would lead to a 30% reduction in average LOS, the non-dedicated ICU would still outperform the dedicated ICU in terms of lower rescheduling rates and higher occupancy rates of available beds. The rejection rates for the dedicated (7.5%) and non-dedicated (7.7%) ICU would be almost equal. One might wonder whether a significant decrease in LOS is still realistic today. The fourth scenario studied unexpected increases in unplanned patient inflow. The non-dedicated ICU adapts easier to the situation in terms of higher bed occupancy rates. In the case of a 30% increase in unplanned patients, 22.5% of the beds remains empty in a dedicated design, while this is 16.6% for the non-dedicated ICU. Thus, more beds remain empty while at the same time rejection and rescheduling rates increase in the dedicated ICU.
The simulation models made clear that from a resource efficient perspective a non-dedicated ICU outperforms a dedicated ICU. Yet, some studies found improved individual patient outcomes in a dedicated ICU design [ 2 , 10 , 11 , 12 , 13 ], whilst others did not [ 14 , 15 , 16 ]. We quantified some surprising ‘jump’ effects for the specialisms that some other papers have not seen – e.g. when there is a long-hauler. Song et al. [ 17 ] as well as Li et al. [ 18 ] suggest that behaviours might change in the dedicated – a greater sense of ownership of patients, and in our case greater sense of specialization for a given specialism. This would suggest that using the same service rates for both the simulation of the non-dedicated ICU as well as the dedicated ICU, might not be realistic, since dedicated ICU’s might have slightly better length of stay for instance. In this light, it should be noted that it remains unclear whether these potential positive effects in the dedicated ICU are associated with the level of specialization or are a result of structural lower bed occupancy rates in this setting. Contrary to low bed occupancy, high occupancy rates could result in higher rejection and rescheduling rates, which are associated with higher mortality rates and inferior patient prognosis [ 7 , 25 , 26 , 27 , 28 , 29 ]. Hence, the previously found positive effects of a dedicated design in some studies could also have been effects of structural lower bed occupancy rates in this setting, instead of being an effect of a higher level of specialization. Furthermore, specialization and impact on outcome may also follow a U-shape curve in which higher level of specialization may also result in not being able to diagnose and treat complications of another domain. Taken together with other studies that did not find evidence for improved outcomes for individual patients in a dedicated ICU design, the potential gains of a dedicated design remain uncertain, while capacity benefits of a non-dedicated design are evident [ 14 , 15 , 16 ].
Strengths of this study are the development and application of a simulation model that quantifies trade-offs that are important in capacity management in ICUs. ICU’s can use local admission data to personalize the model. Limitations of this study are that while designing our simulation model, we were not able to include daily practice issues such as the limitation of the number of available beds due to sickness or holiday leave of nursing staff, changes in inflow of patients throughout the year, etcetera. The simulation furthermore quantifies three capacity trade-off measures, but does not include assessment of quality, survival, service times, costs and other measures that are also involved in the multi-criteria decision of ICU design. Further, the simulation model was only used in one single-center case, and we did not explore other ICU designs or more flexible models. Other industries showed for example that if products are interchangeable in a multi-factory supply network (long-chain-model), in which each factory has a backup (e.g. factory one has two as backup, factory two has three as backup, etc.) then the performance improves [ 30 ]. However, for ICU care delivery, it is unknown what the quality and safety effects are if for example a dedicated surgery patient, is admitted to a dedicated cardiology ward.
Future research could expand the simulation model and add for example a dedicated ‘isolation’ unit to support ICU design decision making during a pandemic such as COVID-19 or outbreak of more regular infectious diseases that require patients to be treated isolated from other patients.
The model we present shows how a simulation can be utilized to make trade-offs between clinical goals in terms of rejection and rescheduling rates and efficiency in terms of occupancy rates. It helps to find a bed occupancy rate at which the rejection and rescheduling rates are acceptable for a specific ICU in different scenarios. The insights gained from the model can support decision making on the local ICU design. The model showed that a non-dedicated design outperforms a dedicated ICU in terms of higher efficiency. These metrics, as a function of capacity and design, are useful inputs to complement local data on quality and local specialization skills to support a local ICU design decision.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Online access to the R code of the event simulation model is available on reasonable request.
Gullo A, Besso J, Lumb PB, et al. Intensive and critical care medicine. World Federation of Societies of Intensive and Critical Care Med; 2009.
Diringer MN, Edwards DF. Admission to a neurlogic/neurosurgical intensive care unit is associated with reduced mortality rate after intracerebral hemorrhage. Crit Care Med. 2001;29:635–40. https://doi.org/10.1097/00003246-200103000-00031 .
Article CAS PubMed Google Scholar
Van der Sluijs AF, Van Slobbe-Bijlsma ER, Chick SE, et al. The impact of changes in intensive care organization on patient outcome and cost-effectiveness-a narrative review. J Intensive Care. 2017;5:13. https://doi.org/10.1186/s40560-016-0207-7 .
Article PubMed PubMed Central Google Scholar
Bennett S. Design, organization and staffing of the intensive care unit, Surgery (Oxford). 2012;30(5):214–218. https://doi.org/10.1016/j.mpsur.2015.02.002 .
Clancy H, Johnson C. Design, organization and staffing of the intensive care unit. Surg (Oxford). 2020;39(1):7–14. https://doi.org/10.1016/j.mpsur.2020.11.007 .
Article Google Scholar
Yartsev A. Design and staffing of intensive care units , https://derangedphysiology.com/required-reading/administration-and-data-management/Chapter%20111/design-and-staffing-intensive-care-units , 2015. [Online]. Last updated: 11/12/2021, Accessed on: 07/01/2022.
Rewa OG, Stelfox HT, Ingolfsson A et al. Indicators of intensive care unit capacity strain: a systematic review, Crit Care. Mar 27 2018;22(1):86. https://doi.org/10.1186/s13054-018-1975-3 .
EuropeanCommision. Commision staff working document: on an action plan for the EU health workforce, European Commision, Strasbourg, 2012. [Online]. Available: https://op.europa.eu/nl/publication-detail/-/publication/402bad92-c66f-4d45-9984-70e199dfd312/language-en .
Hopp WJ, Spearman ML, Press W, editors. Factory Physics , 3rd ed. 2011.
Balachandran R, Nair SG, Gopalraj SS et al. Jul : Dedicated pediatric cardiac intensive care unit in a developing country: Does it improve the outcome? Ann Pediatr Cardiol. 2011;4(2):122-6. https://doi.org/10.4103/0974-2069.84648 .
Menaker J, Dolly K, Rector R, et al. The lung rescue unit-does a dedicated intensive care unit for venovenous extracorporeal membrane oxygenation improve survival to discharge? J Trauma Acute Care Surg. Sep 2017;83(3):438–42. https://doi.org/10.1097/ta.0000000000001524 .
Bukur M, Habib F, Catino J et al. Does unit designation matter? A dedicated trauma intensive care unit is associated with lower postinjury complication rates and death after major complication. J Trauma Acute Care Surg, 78, 5, pp. 920–7; discussion 927-9, May 2015, https://doi.org/10.1097/ta.0000000000000613 .
Mirski MA, Chang CWJ, Cowan R. Impact of a neuroscience intensive care unit on neurosurgical patient outcomes and cost of care. J Neurosurg Anesthesiol. 2001;13:83–92. https://doi.org/10.1097/00008506-200104000-00004 .
Timmers TK, Joore HC, Leenen LP. Changes after transformation from a specialized surgical unit to a general mixed intensive care unit. Crit Care Nurs Q. Jan-Mar 2014;37(1):115–24. https://doi.org/10.1097/cnq.0000000000000010 .
Checkley W, Martin G, Brown SM, States Critical Illness and Injury Trials Group Critical Illness Outcomes Study. Feb : Structure, process, and annual ICU mortality across 69 centers: United, Crit Care Med. 2014;42(2):344–56. https://doi.org/10.1097/ccm.0b013e3182a275d7 .
Lott JP, Iwashyna TJ, Christie JD et al. Critical illness outcomes in specialty versus general intensive care units, Am J Respir Crit Care Med. Apr 15 2009;179(8):676–83. https://doi.org/10.1164/rccm.200808-1281oc .
Song H, Tucker AL, Murrel KL. The diseconomies of Queue Pooling: an emperical investigation of Emergency Department length of Stay. Manage Sci. 2015;61(12):3032–53. https://doi.org/10.1287/mnsc.2014.2118 .
Li X, Liu D, Yang M, Fry MJ, Xie X. Staffing decisions in a tele-ICU: dedicated versus flexible resources. IISE Trans Healthc Syst Eng. 2020;10(3):172–83. https://doi.org/10.1080/24725579.2020.1749911 .
Article CAS Google Scholar
OECD. Healthcare use - Lenght of hospital stay. https://data.oecd.org/healthcare/length-of-hospital-stay.htm , accessed 31-05-2022.
Alban A, Chick SE, Dongelmans DA et al. ICU capacity management during the COVID-19 pandemic using a process simulation. Intensive Care Med. Aug 2020;46(8):1624–6. https://doi.org/10.1007/s00134-020-06066-7 .
Hasan I, Bahalkeh E, Yih Y. Evaluating intensive care unit dmission and discharge policies using a discrete event simulation model. Simulation 96(6), 501–18. https://doi.org/10.1177/0037549720914749 .
Ogrinc G, Davies L, Goodman D, et al. SQUIRE 2.0 (standards for QUality Improvement Reporting Excellence): revised publication guidelines from a detailed consensus process. Volume 25. ed. BMJ Quality & Safety: BMJ journals,; 2016. pp. 986–92.
Alban A, Chick SE, Lvova O et al. A simulation model to evaluate the patient flow in an intensive care unit under different levels of specialization, presented at the Winter Simulation Conference, 2020. [Online]. Available: https://ieeexplore.ieee.org/xpl/conhome/9383852/proceeding .
Institute DHIDH. 2016. [Online]. Available: https://www.zorginstituutnederland.nl/publicaties/publicatie/2016/07/07/kwaliteitsstandaard-organisatie-van-intensive-care .
Azcarate C, Esparza L, Mallor F. The problem of the last bed: contextualization and a new simulation framework for analyzing physician decisions. Omega. 2020;96. https://doi.org/10.1016/j.omega.2019.102120 .
Halpern SD. ICU capacity strain and the quality and allocation of critical care. Curr Opin Crit Care. Dec 2011;17(6):648–57. https://doi.org/10.1097/mcc.0b013e32834c7a53 .
Bagshaw SM, Wang X, Zygun DA, et al. Association between strained capacity and mortality among patients admitted to intensive care: a path-analysis modeling strategy. J Crit Care. Feb 2018;43:81–7. https://doi.org/10.1016/j.jcrc.2017.08.032 .
Fergusson NA, Ahkioon S, Nagarajan M et al. Association of intensive care unit occupancy during admission and inpatient mortality: a retrospective cohort study. Can J Anaesth. Feb 2020;67(2):213–24. https://doi.org/10.1007/s12630-019-01476-8 .
Cardoso LTQ, Grion CMC, Matsuo T, et al. Impact of delayed admission to intensive care units on mortality of critically ill patients: a cohort study. Crit Care. 2011;1–8. https://doi.org/10.1186/cc9975 .
Jordan WC, Graves SC. Principles on the Benefits of Manufacturing Process Flexibility, vol. Vol. 41, 4, pp. 577–594, 1995. https://doi.org/10.1287/mnsc.41.4.577 .
Download references
Acknowledgements
The authors would like to thank Nathalie Nikodym, MSc and Alice Lvova, MSc for their work on earlier parts of the (original) model.
Alban and Chick acknowledge the support of the European Union through the MSCA-ESA-ITN project (676129).
Chick acknowledges research funding as the Novartis Chair of Healthcare Management at INSEAD.
Author information
Authors and affiliations.
Department of Medical Informatics, Amsterdam UMC location University of Amsterdam, Amsterdam, The Netherlands
Danielle Sent & Delanie M. van der Meulen
Jheronimus Academy of Data Science, Tilburg University, Eindhoven University of Technology, ‘s-Hertogenbosch, The Netherlands
Danielle Sent
Management Department, Frankfurt School of Finance & Management, Frankfurt am Main, Germany
Andres Alban
Technology and Operations Management, INSEAD, Fontainebleau, France
Stephen E. Chick
Department of Intensive Care Medicine, Amsterdam UMC location University of Amsterdam, Amsterdam, The Netherlands
Ilse J.A. Wissink, Alexander P.J. Vlaar & Dave A. Dongelmans
You can also search for this author in PubMed Google Scholar
Contributions
Substantial contributions to the conception and design of the work: Danielle Sent, Andres Alban, Stephen E. Chick, Dave A. Dongelmans. Substantial contributions to the acquisition, analysis, or interpretation of data for the work: Danielle Sent, Delanie M. van der Meulen, Ilse J.A. Wissink, Alexander P.J. Vlaar, Dave A. Dongelmans. Wrote the first draft of the manuscript: Delanie M. van der Meulen, Danielle Sent. Revised the manuscript: Andres Alban, Stephen E. Chick, Ilse J.A. Wissink, Dave A. Dongelmans. Final approval of the version to be submitted for publication and agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: all authors.
Corresponding author
Correspondence to Danielle Sent .
Ethics declarations
Ethics approval and consent to participate.
No IRB review was necessary because it did not fall under the board’s guidelines as human subjects research.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Sent, D., van der Meulen, D.M., Alban, A. et al. A quality improvement study on how a simulation model can help decision making on organization of ICU wards. BMC Health Serv Res 24 , 708 (2024). https://doi.org/10.1186/s12913-024-11161-2
Download citation
Received : 23 December 2022
Accepted : 31 May 2024
Published : 05 June 2024
DOI : https://doi.org/10.1186/s12913-024-11161-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Critical care
- Computer Simulation
- Organizational decision making
- Quality of Healthcare
- Hospital Bed Capacity
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
More From Forbes
Genai for aiops catapults digital transformation in healthcare.
- Share to Facebook
- Share to Twitter
- Share to Linkedin
Shailesh Manjrekar is the Chief Marketing Officer at CloudFabrix , the inventor of Robotic Data Automation Fabric and an AIOps Leader.
Regulated industries like healthcare and FinTech always have to adopt technology transformations with caution. AI has the potential to make a profound impact on these industries; however, leveraging AI for operational efficiencies is a good, cautious first step. I want to highlight how healthcare is one such industry leveraging AIOps—artificial intelligence for operations—to improve not just operational (IT) but also business (people and processes) and organizational efficiencies.
The healthcare industry is experiencing a profound transformation, driven by the digitalization of patient records via electronic health records (EHRs), the use of connected devices and a move toward data analytics, precision medicine and telemedicine. These advancements offer unparalleled opportunities for improving patient care and efficiency, but they also add IT complexity and regulatory challenges, including HIPAA compliance.
Moreover, patients now demand services and accessibility similar to those in retail and banking. Fulfilling these demands necessitates IT systems that are secure, user-friendly and always on. Downtime isn't just inconvenient—it can delay vital care, increasing patient risks and potentially endangering lives.
The Evolution Of AIOps
Gartner coined the term AIOps in 2016, as part of an effort to understand how data analytics were enabling new efficiencies for the ITOps team, and it stands for "AI for IT operations." AIOps differs from other disciplines like MLOps and DataOps.
Best High-Yield Savings Accounts Of 2024
Best 5% interest savings accounts of 2024.
Since then, generative AI and large language models (LLMs) have democratized AIOps. Another major transformation is how AIOps has morphed into AI for operations (not just IT, but the entire organization).
AIOps must offer insights not only into operational awareness but also into business awareness, encompassing people and processes, particularly in the context of healthcare practitioners, users and providers. Ultimately, it should extend to organizational awareness, where it should be able to answer the question: "Are we OK?" It needs the ability to ingest data from all kinds of organizational data sources, enrich the data with active metadata and glean insights with AI—all functions of a data-centric AIOps platform .
Prerak Garg, a senior director at Microsoft and partner, highlights the importance of managing the performance of IT systems in healthcare in his paper excerpt. The metrics around patient care, speed of care and job satisfaction are all heavily influenced by the performance of the system that the physicians rely on. For instance, delays in accessing EHRs can hinder timely decision-making in critical care, while downtime in imaging services can delay diagnoses and treatments.
In an environment where every second counts, traditional IT operations management strategies, reliant on manual intervention and reactive troubleshooting, are often ill-equipped to meet these demands.
AIOps And Its Relevance To Healthcare
AIOps offers an innovative approach to managing this complexity in healthcare IT environments, ensuring a seamless experience for both providers and patients when using these digital tools.
According to Garg, "The significance of AI in healthcare is underscored by its unparalleled capability to process and analyze vast datasets far beyond human capacity, thus offering insights and predictions with unprecedented accuracy."
Implementing AIOps In Healthcare
Choosing the right type of AIOps platform is pivotal. While industry-agnostic solutions offer a broader overview of the IT environment, they could lack the depth required for industry-specific challenges.
GenAI is set to transform AIOps in healthcare. The potential of a healthcare-specific foundational model is transformative. However, there are challenges around eliminating hallucinations and biases and grounding the models with the right context. Enriching data across adjacent domains is crucial, as illustrated in the article " Transformative Potential of a Healthcare-Specific Foundational Model ."
It's also essential to evaluate the current IT infrastructure for AIOps integration, with a focus on system compatibility and interoperability. OpenTelemetry (OTel)-based AIOps solution facilitates this by aligning with standards like HL7, DICOM or FHIR. It standardizes telemetry data collection (metrics, traces, logs) via OTel collectors, helping healthcare organizations monitor and ensure efficient system integration and information exchange across their IT ecosystem.
Implementing a solid data governance policy is equally vital, ensuring that data handling meets healthcare regulations like HIPAA. Starting with pilot projects and adopting a feedback-driven, iterative approach to implementation facilitates smoother AIOps integration, tailored to the organization's specific needs.
Case Studies: AIOps In Action
• Our company worked with a leading integrated healthcare provider that utilized a data-centric AIOps platform as part of its seven-year data center refresh strategy, spanning 10 data centers, 500,000 assets and 15,000 healthcare applications. This implementation enabled asset inventory insights, capacity utilization optimization, lifecycle analytics, change management, alert noise reduction and incident management.
• Using AIOps to analyze network usage, a telehealth provider that we worked with identified and preemptively managed high-demand periods, maintaining quality video consultations during peak times by adjusting bandwidth.
• Microsoft's DAX Copilot is a good case study of AI as a healthcare copilot, after its Nuance acquisition . DAX leverages voice-activated queries to relieve clinicians from the administrative burdens of clinical documentation and diagnostic assistance while becoming a virtual provider.
The Future Of AIOps In Healthcare
The evolution of AIOps in healthcare IT signifies a paradigm shift toward more efficient, secure and patient-centered operations. From what I've seen, experts across the field concur that AIOps is not merely a trend but a foundational shift.
The future of AIOps lies in even more sophisticated predictive analytics capabilities, enabling the prediction of patient health trends based on real-time data analysis. For example, AIOps can analyze vast streams of data from health monitors to smart hospital beds in real time, offering unprecedented insights into patient health and system performance.
In embracing AIOps, healthcare IT leaders can help ensure their organizations are not just keeping pace with technological advancements but are pioneering the future of healthcare delivery. It's a strategic move toward a future where healthcare is more responsive, resilient and aligned with the needs of patients and providers alike.
Forbes Technology Council is an invitation-only community for world-class CIOs, CTOs and technology executives. Do I qualify?

- Editorial Standards
- Reprints & Permissions
Bias of American Thinker
- Balanced News
- Story of the Week
- News Curation Principles
- Newsletters
- Balanced Search
A case study in the challenges facing health care

In 2023, the top six health insurers collectively earned over one trillion dollars in revenue, a staggering figure that has raised questions about whether the current healthcare dynamic is sustainable and serving all stakeholders effectively. There's no question that health insurance provides a valuable service to millions of Americans. But when that much money winds up concentrated in such few hands, things are probably not working within the healthcare marketplace as they should. At a time when many hospitals are struggling to stay afloat and private health insurance premiums have...
American Thinker
Related Coverage

Similarity Hub is a project between AllSides and More Like Us that highlights survey data on topics on which Americans largely agree. Its goal is to correct political misperceptions, highlight common ground, and help people feel calmer and more united.
Explore more data in the Similarity Hub
Discover more common ground on Healthcare
AllSides Picks

June 7th, 2024

Ethan Horowitz
June 6th, 2024

Discuss & Debate healthcare
LGBTQIA+: Author Talk & Living Room Conversation
Discover hundreds more upcoming events
More News about Healthcare from the Left , Center and Right
From the left, from the center, from the right.

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Integr Care
- v.16(4); Oct-Dec 2016

What Is Case Management? A Scoping and Mapping Review
Ms sue lukersmith.
1 Faculty of Health Sciences, Centre for Disability Research and Policy, University of Sydney, Sydney, Australia
2 Mental Health Policy Unit, Brain & Mind Centre, University of Sydney, Sydney, Australia
Dr Michael Millington
Luis salvador-carulla.
The description of case management in research and clinical practice is highly variable which impedes quality analysis, policy and planning. Case management makes a unique contribution towards the integration of health care, social services and other sector services and supports for people with complex health conditions. There are multiple components and variations of case management depending on the context and client population. This paper aims to scope and map case management in the literature to identify how case management is described in the literature for key complex health conditions (e.g., brain injury, diabetes, mental health, spinal cord injury). Following literature searches in multiple databases, grey literature and exclusion by health condition, community-based and adequate description, there were 661 potential papers for data extraction. Data from 79 papers (1988–2013) were analysed to the point of saturation (no new information) and mapped to the model, components and activities. The results included 22 definitions, five models, with 69 activities or tasks of case managers mapped to 17 key components (interventions). The results confirm the significant terminological variance in case management which produces role confusion, ambiguity and hinders comparability across different health conditions and contexts. There is an urgent need for an internationally agreed taxonomy for the coordination, navigation and management of care.
Introduction
Case management, also known as care coordination is a complex integrated health and social care intervention and makes a unique contribution to the health, social care and participation of people with complex health conditions.[ 1 , 2 , 3 , 4 ]. In the 1960’s case management emerged in response to the de-institutionalisation of large numbers of people with severe mental health conditions who required referral to outpatient health and other community services. During the 1970’s and 1980’s, the increasing cost of health care and de-centralisation of health services influenced the role of case managers [ 5 , 6 ]. Since the 1990’s, case management has existed in a range of settings including acute, post-acute hospital, rehabilitation, long term care and community-based settings. Case management tasks are now performed by people from various disciplines, for people with different problems in diverse contexts and communities. These multiple interdependent and interacting parameters of case management produce variability in the description of case management [ 5 , 7 , 8 , 9 ]. The significant terminological variance, lack of understanding and a common language for case management and care coordination has impeded quality analysis, policy and planning [ 4 , 10 , 11 , 12 ]. There is an urgent need for a common international language, but which first requires an understanding of the terms used to describe case management in the literature.
There are multiple parameters that influence case management. Case management operates in very different service sectors (health, social, correctional, work/vocational, veterans, legal sectors) and different settings (public sector, private and non-government organisations) and with different community and support resources (high and low resource settings). Its presence in diverse contexts demonstrates the importance of case management in the horizontal integration of care across health services, social services and other sectors as well as the vertical integration across primary, community, hospital and tertiary health care services [ 13 ].
In the health sector, case management and care coordination occurs within an inpatient setting, or mobile and community-based. In this scoping review we only considered community-based case management. Community-based case management is a mobile rather than office based health service. Case manager contact with the client (and/or their family) may occur in a different setting such as the client’s home, workplace or other community venue as considered appropriate by the case manager and client. Community-based case management is the most holistic and person-centred of the approaches (model) as it meets at the junction of the client in their own context. Due to its holistic and comprehensive approach, community-based case management is also likely to involve most of the components of case management of other models that have a narrower focus.
Health sector case managers are from different disciplines (e.g. nursing, occupational therapy, physiotherapy, psychology, rehabilitation counselling, social work, speech pathology) and different practice areas (social and welfare, primary care). Further, there are a number of case management models and theories underpinning practice approaches, due in part to the different sectors where case management operates, the age and health conditions of the client [ 9 ]. Hence, both in practice and the literature, a range of names are applied to the role and tasks of a case manager such as: community/care coordinator, support facilitator or broker, case monitor, discharge planner, planning facilitator, case worker, clinical/rehabilitation case manager. Other client characteristics and temporal factors (e.g. whether the client’s problem is new, acute or chronic) also affect the tasks and actions of the case manager. All these different factors related to the case manager, client and context influence what case managers do (i.e. case management tasks as interventions). Whilst there are differences between case management tasks and context, there are also similarities, yet there is no common language to describe these variations.
In spite of the abundance of literature on case management in all its forms, case management descriptors are often non-existent or poorly described with mixed concepts and constructs. There appears to be no consensus on what is, and importantly what is not case management. The heterogeneity, complexity and inadequate descriptions of the components of case management demands a flexible exploratory approach and consideration of a breadth of literature compared to the methods of a focused and narrower systematic review. This review aims to characterise and map how case management has been described in the literature. The review did not seek to assess the quality, nor synthesise the evidence on effectiveness of case management interventions. The focus in this research programme was on the components and definitions. It is the first step of a larger study to develop a taxonomy, a knowledge map and common language for community-based case management. Community-based case management was the focus because it is likely to contain elements of other approaches. People with key complex and chronic health conditions were selected, as case management is frequently used to support their management and the integration of their care.
Aim of the research
The objective of this study was to scope and map ‘How case management is described in the literature’ in particular the definition, the theoretical basis, the components and activities (interventions) performed by the case manager.
Theory and Methods
Study design.
The study design was a scoping and mapping review. As exploratory research, scoping reviews are particularly appropriate when the area is complex, and used to map the key concepts underpinning a research area [ 14 ]. A scoping study aims ‘to map the literature on a particular topic or research area and provide an opportunity to identify key concepts; gaps in the research; and types and sources of evidence to inform practice, policymaking, and research’ (p. 8) [ 15 ]. A scoping review balances the feasibility of the literature search with the breadth and comprehensiveness in the scoping process [ 16 ].
The scoping review used five of the six steps in the framework articulated by Arskey et al [ 17 ] and extended by Levac [ 16 ] which are: 1) identifying the research question; 2) identifying relevant studies; 3) study selection; 4) charting (mapping) the data; 5) collating, summarizing and reporting the results. Consistent with many scoping reviews, quality appraisal was not undertaken as the focus was on language and descriptions of the concepts and components of case management rather than the methodology, outcomes and efficacy of the included studies [ 15 , 16 , 18 , 19 , 20 ].
Scoping and mapping methodology
We used an iterative process in the scoping review that allowed for flexibility in the search, reviewing and mapping steps. A flexible approach was necessary due to the diversity in the terms around case management, the model or approach taken, the contexts in which it operates and the health conditions of the recipients of case management. The steps taken for the scoping review are outlined below:
1. The research question
The main research question was ‘How was case management described in the literature’. The sub-questions were:
- How was case management for complex and chronic health conditions, described in the literature (brain injury, diabetes, mental health, spinal cord injury)?
- What was the theoretical basis (the model) (if any) linked to the case management approach?
- What were the components, and activities performed in case management; and how are they described?
2. Identify relevant studies
This scoping study used quantitative, qualitative research literature as well as the grey literature. Peer reviewed papers provide information from observational and experimental research. Grey literature provides information from expert practice knowledge and expert experience knowledge [ 21 ]. In this study we consider grey literature to be literature ‘ produced at all levels of government, academics, business, industry in print and electronic formats, but which is not controlled by commercial publishers ’ [ 22 ]. It includes papers, reports, technical notes or other documents produced and published by governmental agencies, academic institutions, professional associations such as case management societies, and other case management organisations and groups that develop standards or describe services and the activities of case managers.
The search terms and strategy were developed, trialled and discussed then refined with the co-authors and an information specialist. Over three meetings, the co-author team reviewed examples of the literature and refined the selection of studies. This refinement involved combining key words for case management and key words for definition in the final search strategy with limits to specific health conditions. Our decisions on key words and limits are outlined below:
- – The variation in names, and complexities of contexts and health conditions posed challenges to systematic searching across multiple databases. We collectively identified the relevant descriptors of case management for the key word search terms based on our familiarity with the literature and community-based case management context.
- – There were no limits on the type of study as the range of literature of interest included qualitative, quantitative intervention and non-intervention studies for key health conditions, reports on case management standards, service descriptions, literature reviews and theoretical papers.
- – Literature on case management not provided in the community was excluded. However, research papers and grey literature that referred to general case management activities and actions were included.
- – The number of descriptions for case management required limits established for the range of health conditions. Five complex or chronic health conditions were included: brain injury, diabetes, mental health conditions and spinal cord injury. Brain injury was included as it is complex health condition and potentially impacts multiple domains of health. It was also of interest to the industry partner (Lifetime Care) involved in the larger study [ 23 ]. Mental health conditions were included because of the complex impact of the conditions but also because of its history in case management. Diabetes was included as it is a common chronic health condition. Although less common, spinal cord injury was included as it provides its own set of unique challenges around long term community-based and integrated supports.
Multiple databases were searched for published literature, complemented by searches on key organisation websites and snowballing with hand searching of references lists. The database search was carried out in Week 3 July 2013. The databases were Medline, Cochrane, OTseeker, and PsycBITE. The grey literature key websites searches were conducted in August 2013 and February 2014. The organisational websites were: Australia : Case Management Society of Australian and New Zealand (CMSA); Transport Accident Commission (TAC); Lifetime Care and Support Authority (LTC); National Disability Insurance Agency (NDIA); WorkCover Authority (NSW), Brain Injury Rehabilitation Directorate (New South Wales – NSW); Department of Health NSW; Canada- National Case Management Network; United Kingdom (UK) – Case Management Society of the United Kingdom (CMSUK); British Association of Brain Injury Case Managers (BABICM); National Health Service (NHS); United States of America (USA) Agency for Healthcare Research and Quality; Commission for Case Manager Certification; Case Management Health System; Case Management Society of America; American Case Management Association.
The limits were English language, humans with no limits on study type. The inclusion criteria were:
- – No limits on publication dates (Medline 1946- Week 2 July 2013)
- – Community-based case management
- – Case management related to health conditions of brain injury, diabetes, mental health conditions, spinal cord injury
- – A definition of the case management and description of the actions, activities, interventions.
3. Study selection
The authors agreed that an iterative process to the exclusion, selection of studies and data extractions was appropriate. In order to manage the copious amounts of literature located, a hierarchy of steps for the exclusion of literature was developed in consultation with co-authors. A bibliographic manager database (EndNote X7) supported the management of the body of literature and exclusion process. The steps for exclusion after the removal of duplicated papers were:
- Exclusion by health conditions, social issues (e.g. ex-prisoners or offenders, homeless persons), single health conditions in low health service resource settings (e.g. Malaria in a developing country),
- Exclusion by case management setting (inpatient, acute care or residential settings such as nursing home, correctional institution), telehealth (no face to face).
- Exclusion because of inadequate (or absence) of a description of case management, the case manager actions or interventions.
4. Mapping the data (charting)
The scoping review involved conceptual mapping to the point of saturation when no new descriptions, concepts or components were identified [ 17 , 24 ]. The focus was on the components and definitions of case management interventions. The information was extracted and stored on an Excel spreadsheet for data management and to enable numerical summation and qualitative analysis. SL extracted data from a sample of 6 papers, which was then reviewed and checked by LSC and MM. The information variables to be extracted were then revised and reduced in agreement with all authors. SL continued with the data extraction and mapping. The final extraction table was reviewed by all authors. Obvious inconsistencies noted were discussed and revisions made.
Extraction and mapping of the case management information began at a global level of the country and type of paper, followed by high level information on the model or approach, theoretical basis, then more detailed components and then finally the description of these components. The final variables mapped were: paper author, year of publication, title, type of study where relevant (or paper), health condition of population, country of study, name of case management model, linked theoretical basis, case management definition, components of case management, descriptors, actions/activities described (sometimes called steps, activities, actions or interventions in the literature) and additional comments. The mapping of information was done to the point of saturation, where no new information (concepts, descriptions, components) were identified. Once it was apparent that no new information was extracted, a further six papers were reviewed and data extracted and mapped, to ensure that the point of saturation had been reached.
5. Collating, summarizing and reporting the results
The information and mapping results from the studies were collated, analysed, summarised and reported. The results were also used as one step in a larger study to develop a taxonomy on case management [ 23 ].
Our search yielded a total of 6,847 peer reviewed research study papers and 22 grey literature papers, a total of 6,869 references. This was reduced to 6,314 after duplicates were removed (see Figure Figure1 1 for a summary of the screening and eligibility process). After reviewing the titles and abstracts from the search results for health condition (excluded n = 3,600), and removing practice context other than community-based (excluded n = 1,199), and finally removing those with inadequate description in the paper (excluded n = 854), we had 661 potential references for data extraction and mapping. A total of 12 grey literature papers and 61 randomly selected research papers were included in the data extraction and mapping to the point of saturation, when no new information was provided. We selected the grey literature papers because of their focus and the content related to the components to be mapped (model, definition, description of activities or interventions by case managers), such as model descriptions or statements from professional case management associations. To ensure the point of saturation was reached, the data from a further 6 research papers was extracted and mapped making a total of 79 papers.

Flow of Study Selection.
The papers analysed included 65 papers from peer reviewed journals published 1988–2013 and 14 papers from the grey literature. Appendix 2 provides the details of the 79 included papers. Table Table1 1 describes the global analysis of the papers. In 63 papers there was 10 different countries of focus and 14 there was an international perspective (e.g. literature review). There were 26 papers on mental health, eight on diabetes or chronic/long term health conditions, 12 brain injury, two on spinal cord injury and 31 were not related to specific health conditions. There was one systematic review, 42 qualitative research methods papers, 7 intervention studies, 11 theoretical papers, 5 editorial perspectives or expert opinion, 11 papers were practice guidance and professional association standards and two conference papers.
Description of the mapped papers.
The next layer of data extraction resulted in an increasing level of detail on case management as described in the literature. Twenty-three specifically identified definitions of case management, (rather than general statements) are provided in Appendix 3. Some definitions were repeated in a number of papers, for example a case management society definition was used in a number of papers.
We found descriptions of different models and theoretical descriptions of the case management approaches in 23 papers. These were mapped to five different models. Exploration on the most common or frequently adopted model was not in the study scope. In some instances, there was a specific model or theoretical basis. For other papers, the approach was broadly described. On this basis, we could map the approach to a model. In other papers several models were discussed (e.g. systematic review). There was a total of 57 papers which did not identify the theoretical basis of the case management approach nor refer to a model. The mapped models of case management, related terms, theoretical description and case management features are provided in Table Table2. 2 . In this table, we have not provided examples of papers providing a description as many papers such as literature reviews, opinion or theoretical papers and systematic reviews referred to a number of these models or their variations.
Mapped models of case management, and related names, theoretical description and case management features.
*refer to Appendix 2 for details of the articles in scoping study.
The key components of case management described in the papers were extracted. Terms used for these components include activities, functions, tasks, responsibilities, duties, steps and interventions, standards. Across the 79 papers, we mapped 69 of the various terms used in the literature to 17 component headings, which were broadly defined. Only examples of the terms extracted from the literature and mapped to the component are provided in Table Table3 3 .
Examples of the terms in the literature mapped to component heading.
The results of the scoping and mapping review confirms that there is a huge body of peer reviewed and grey literature on case management, yet there is significant terminological variance. Following literature searches, exclusions by health conditions, case management context (community-based) and papers with inadequate descriptions we extracted data and mapped the components of case management from papers (n = 79) to the point of saturation. There was a broad range of literature included in the study (quantitative, qualitative, theoretical and practice guidance papers) and from 11 countries and international perspectives (n = 14).
The mapping of extracted data was complicated because of the variability in the language to describe case management. There was heterogeneity in the descriptions, terms and phrases to describe the models, which reflects the difficulties in the articulation of the differences and similarities between the models and the interventions provided by case managers. For the purposes of this scoping review, we mapped the models described to five key models of case management based on a theoretical description of each. Whilst there are more than five case management models, many are variations, adaptations and interpretations of a model to the specific context.
We extracted 69 components in the literature to describe what case managers do (the interventions/activities). We identified 17 key components and mapped the 69 descriptions to these. Each key component had multiple different but related terms to describe the intervention. There was also complexities mapping of the components (activities and interventions) performed by the case manager. In the literature, there was semantic confusion between the components (interventions) of case managers with skills, standards, aims and objectives. For example, ‘stable person- invested but not involved’ [ 54 ] is a description of a standard or skill of the case manager (the ‘how’) rather than a component of case management (the ‘what’ is done). The component descriptions were also variously defined from different perspectives of the client, case manager, project or team organisation, program, service or organisation. For example, the description of ‘gatekeeper’ (clinical and financial) [ 9 , 55 , 56 ] listed as a case manager activity, is aimed at the sustainability of the service or system, at most is an (administrative) responsibility of the case manager to the service or organisation rather than an intervention directed at the client. These difficulties confirm the complexity around case management resulting in terminological variance used. The literature in this scoping study spanned a 25 year period (1988 to 2013). While case management to coordinate services has been used since the late 19 th century and contemporary case management emerging since the 1960’s [ 57 ], this scoping review confirms that over time the description and terminological variance remains.
The terminological variance reflects the ambiguity and confusion about roles and the interventions performed by case managers. Specificity and replicability of case management are essential to evaluation of effectiveness [ 58 ]. There are complex interdependent and dependent factors influencing what case management interventions are done, when, with whom and in what context. A clear understanding and consensus on the components and a common language to describe these factors will provide the tool for measuring outcomes, and making comparisons for effectiveness and quality evaluations.
Limitations
The study was limited to the descriptions and terms used in the literature to refer to the same or similar concept including the model, theory and components. A limitation in the search strategy was not including all possible databases. Databases such as EMBASE were not searched as it is primarily a biomedical and pharmacological database and considered unlikely to host a significant body of community-based case management literature. Search of the database CINAHL may have revealed additional relevant literature. Whilst other databases could have been considered, the volume of literature from the four databases provided more than sufficient material to use for data extraction to the point of saturation. The extensive search for grey literature added to the volume of peer reviewed literature. However, the point of saturation was reached after the data extraction from 79 articles retrieved through the four databases and multiple grey literature websites.
The search restricted to only four health conditions is a study limitation. The trial of searches without health conditions limits produced in excess of 10,000 hits on Medline alone. For pragmatic reasons, the search strategy was subsequently limited to include four health conditions. Those selected by the authors were known to have community-based case managers involved in health, social care and education sectors.
The study did not undertake quality analysis of the research papers. It is recognised that this meant that equal weight was given to all papers and grey literature, which we consider was justified given the purpose of the scoping study to examine descriptors of case management components and context not efficacy of case management. There can also be concerns about potential bias in scoping reviews related to the reviewers own interests, lack of training and limited view due to discipline or language [ 59 ]. Others suggest that there is a ‘trade off’ of potential source of bias in perception and interpretation of a subject and conversely that subject matter experts are necessary [ 59 , 60 , 61 , 62 ]. In this instance, considering the complexity in case management, the three researchers background and expert knowledge was considered an advantage to the scoping and conceptual mapping.
The scoping review used five of the six steps in the framework articulated by Arskey et al [ 17 ] and extended by Levac [ 16 ]. The 6 th step it the Arskey/Levac methodology is consultation with a broader group of experts and stakeholders to discuss the findings. This step was not performed as part of the scoping review but did occur in a subsequent step of the larger study to develop a taxonomy on case management. In the larger study, a nominal group of case management experts extensively discussed the results of the scoping review to develop the Beta 2 version of the case management taxonomy [ 23 ].
Case management with all its different names, variations and contexts continues to support the coordination, integration and management of health and social care in many different contexts for different health conditions. The results of this scoping and mapping study confirms the significant terminological variance which produces role confusion, ambiguity and hinders comparability across different health. There is an urgent need for an internationally agreed taxonomy for the coordination, navigation and management of care. The result of this scoping and mapping review was the first of four steps to develop the case management taxonomy finalised in 2015. [ 23 ].
Future research
The results from this scoping and mapping study is part of a larger study to develop a knowledge map and common language, the case management taxonomy which has an intervention tree, service tree and glossary [ 23 ].
Supplementary Files
The supplementary files for this article can be found as follows:
- Supplementary File 1: Appendix 1. ijic-16-4-2477-s1.pdf
- Supplementary File 2: Appendix 2. ijic-16-4-2477-s2.pdf
- Supplementary File 3: Appendix 3. ijic-16-4-2477-s3.pdf
Helen Killaspy, Professor of Rehabilitation Psychiatry, University College London, UK.
Two anonymous reviewers.
Competing Interests
The authors declare that they have no competing interests.
Author contribution
All authors contributed to the research and manuscript.
Translational medicine 101: The future of personalized care
- Published on June 7, 2024
- By Diana Nichols
In an era marked by rapid advancements in healthcare , translational medicine emerges as a critical field, acting as the bridge between groundbreaking genetic research and practical clinical applications. This new discipline is pivotal, ensuring that scientific discoveries are not just published in journals but are swiftly and effectively transformed into treatments that improve patient outcomes.
What is translational medicine?
Translational medicine is the process by which biologists, clinicians, and technologists collaborate to expedite the journey of scientific discoveries from the “bench” to the “bedside.” This involves refining, developing, and applying new technologies , treatments, and diagnostics to solve pressing clinical needs. It’s about making the connection between molecular insights and medical practice as seamless and as quick as possible.
The role of data management systems
“Translational medicine requires sophisticated data management systems that act less like a map and more like a compass,” explains Dr. Augustine Annan , PhD, a Senior Data Scientist at IMO Health.
His analogy underscores the navigational challenges faced by healthcare professionals who must steer through vast amounts of complex biological data to find clinical applications. These systems are not just repositories of information but are active tools for guiding research towards practical application.
Impact of translational medicine on patient care
One of the most visible impacts of translational medicine is its transformation of electronic health records (EHRs) . By integrating comprehensive, personalized treatment plans into EHRs, translational medicine ensures that clinicians have instant access to the tailored information they need to treat their patients effectively.
Annan highlights this effect: “The impact on EHR systems is transformative, embedding advanced personalized plans that directly influence patient care.”
The core of translational medicine is its ability to tailor treatments based on individual genetic profiles. This personalization is particularly important in the treatment of diseases like cancer, where genetic variations can significantly influence how well a treatment works. For instance, translational researchers use genetic insights to develop targeted therapies that specifically attack cancer cells without harming healthy tissue, significantly improving patient outcomes.
Challenges and solutions
Despite its benefits, translational medicine faces several challenges. The path from discovery to treatment is fraught with technical, regulatory, and ethical obstacles. For every successful therapy, countless others never make it through the necessary trials due to these complexities.
However, innovations in machine learning and artificial intelligence (AI) are beginning to pave the way for more streamlined processes. AI algorithms can predict how new drugs will perform based on vast datasets of clinical trial results, speeding up the development phase and reducing the likelihood of failures.
Case studies in success
Numerous case studies exemplify the success of translational medicine. For example, the development of mRNA vaccines for COVID-19 is a recent, prominent example of translational medicine in action. Researchers were able to design, test, and begin distributing these vaccines in under a year, thanks to decades of prior research into mRNA vaccine technology, showcasing the rapid capabilities of translational approaches.
The future of healthcare
Looking ahead, the implications of translational medicine for the future of healthcare are vast. As technologies evolve, the pace at which new treatments can be developed and approved is expected to increase dramatically. This will not only enhance the ability to treat and cure disease but also significantly reduce the costs associated with long-term healthcare.
Translational medicine stands at the forefront of modern healthcare, a beacon of hope for countless patients and a testament to the power of integrating research, technology, and clinical practice. For healthcare professionals, staying engaged with developments in this field is more than a requirement—it is a responsibility to the future of patient care.
As Annan succinctly puts it, “Embracing translational medicine is essential for driving the innovations that will shape the future of healthcare.”
Want to read more 101 guides? Master the basics of everything from HCPCS codes to NLP and more by clicking here .
Ideas are meant for sharing., sign up today and have ideas delivered straight to your inbox., latest ideas.
- IMO Portfolio
- IMO Core global
IMO Core Procedure
IMO Core Periop
- IMO Discovery for Problems
IMO Precision Sets
IMO Precision Normalize
Top Articles
- SNOMED CT 101
- Medicare Advantage and HCC V28
- Resource Library
- IMO Core Value Calculator
- Product Finder
- Request A Demo
Headquarters
- 9600 West Bryn Mawr Ave. Ste 100, Rosemont, IL 60018
Do Not Sell / Do Not Track
©2024 Intelligent Medical Objects, Inc.
- Terms of Use
Web Design by Solid Digital
POINT OF CARE WORKFLOW
IMO Core and IMO Discovery for Problems
DATA QUALITY MANAGEMENT
- Life Science and Clinical Research
- Health Tech
- EHRs and Point of Care Solutions
- Healthcare Providers
- Health Plans
- Public Health
- Health Information Exchanges (HIEs)
- Our Experts
- Partnerships
IMO is now IMO Health
New name. new logo. same unwavering commitment to data quality in healthcare..
HIMSS Global Health Conference & Exhibition is part of the Informa Markets Division of Informa PLC
- Informa PLC
- INVESTOR RELATIONS
This site is operated by a business or businesses owned by Informa PLC and all copyright resides with them. Informa PLC's registered office is 5 Howick Place, London SW1P 1WG. Registered in England and Wales. Number 8860726.
- Claim HIMSS24 CE Credits
- Get HIMSS25 Email Updates

Global Conference & Exhibition
CREATING TOMORROW'S HEALTH
Save the Date
March 3-6, 2025
Las Vegas, Nevada
Here’s Where Tomorrow Starts
Building the Future of Health IT
Reserve Your Exhibit Space for HIMSS25 Today

TERMS & CONDITIONS

Copyright © 2024. All rights reserved. Informa Markets, a trading division of Informa PLC.
- Accessibility
- Privacy Policy
- Terms of Use
- Visitor Terms And Conditions

COMMENTS
This study systematically synthesizes and critically evaluates evidence in systematic reviews of health care utilization outcomes from case management interventions for the care of chronic illnesses. Results are synthesized from seven English language systematic reviews published between January 1990 and June 2017.
Health Care Management During Covid-19: Insights from Complexity Science. Six case examples demonstrate that health care leaders and clinicians can effectively respond to the Covid-19 pandemic with extensive communication, collaboration, and innovation. Authors: James W. Begun, PhD, and H. Joanna Jiang, PhD Author Info & Affiliations.
Case management programs (CMP) for frequent users of healthcare services with complex needs constitute an effective strategy to improve patient experience of integrated care and to decrease healthcare overuse and cost [10,11,12]. Case management is a dynamic, systematic and collaborative approach used to ensure, coordinate, and integrate care ...
Older patients with multiple chronic conditions are major users of health care, as they often see multiple specialists, frequently visit the emergency department (ED), and have multiple hospital admissions per year. One model to improve care for these high-risk patients is case management, with a nurse or social worker (SW) taking responsibility for coordinating and implementing a patient's ...
Methods. Using a descriptive case study approach, 27,28 we sought to compare the path of the development of the profession of healthcare management in Ethiopia with experiences in the professionalization of healthcare management in the United States. We selected these two countries as paradigmatic cases 29 through which to identify convergent and divergent experiences between country settings ...
Impact Case Studies. AHRQ's evidence-based tools and resources are used by organizations nationwide to improve the quality, safety, effectiveness, and efficiency of health care. The Agency's Impact Case Studies highlight these successes, describing the use and impact of AHRQ-funded tools by State and Federal policy makers, health systems ...
Responding to complex needs calls for integrating care across providers, settings and sectors. Among models to improve integrated care, case management demonstrates a good evidence base of facilitating the appropriate delivery of healthcare services. Since case management is a complex, multi component intervention, with its component parts interacting in a non-linear manner, effectiveness is ...
The case management process. Case management is a collaborative process in which a case manager works with clients to ensure they obtain the proper health care in the most cost-effective manner. This is what the process typically looks like: 1. Screening: The case manager reviews a client's medical records, medical history, and current ...
Health Services Management: A Case Study Approach offers a diverse collection of case studies to help readers learn and apply key concepts of management, with an emphasis on the use of evidence in management practice. The case study authors, many of whom are practitioners or academics who work closely with practitioners, present realistic management challenges across a variety of settings.
Understanding Health Care Management: A Case Study Approach is an independent publication and has not been authorized, sponsored, or otherwise approved by the owners of the trademarks or service marks referenced in this product. This publication is designed to provide accurate and authoritative information in regard to the Subject Matter covered.
The Harvard Chan Case Library is a collection of teaching cases with a public health focus, written by Harvard Chan faculty, case writers, and students, or in collaboration with other institutions and initiatives. Use the filters at right to search the case library by subject, geography, health condition, and representation of diversity and identity to find cases to fit your teaching needs.
Electronic Prior Authorization: The Future of Care Coordination. View the real world case studies of payers and providers who have achieved improvement through use of the healthcare management solutions we provide.
Healthcare case studies provide a unique opportunity to dissect real-world scenarios, understand the decisions made, and measure the outcomes of those choices. One notable success story is the implementation of telemedicine in rural areas. ... Another critical case study involves the management of electronic health records (EHRs). When a large ...
Health Case Studies is composed of eight separate health case studies. Each case study includes the patient narrative or story that models the best practice (at the time of publishing) in healthcare settings. ... The book is useful for non-clinical healthcare management students to introduce various healthcare-related concepts and terminology ...
Case study is a research methodology, typically seen in social and life sciences. There is no one definition of case study research.1 However, very simply… 'a case study can be defined as an intensive study about a person, a group of people or a unit, which is aimed to generalize over several units'.1 A case study has also been described as an intensive, systematic investigation of a ...
Healthcare Quality Management: A Case Study Approach is the first comprehensive case-based text combining essential quality management knowledge with real-world scenarios. With in-depth healthcare quality management case studies, tools, activities, and discussion questions, the text helps build the competencies needed to succeed in quality management.
Health System Innovation in Lesotho: Design and early operations of the Maseru Public Private Integrated Partnership. This PwC case study details the design and launch of an innovative partnership to dramatically improve delivery of healthcare in Lesotho in southern Africa. 07 Jun 2012.
One in 10 people in America lack health insurance, resulting in $40 billion of care that goes unpaid each year. Amitabh Chandra and colleagues say ensuring basic coverage for all residents, as other wealthy nations do, could address the most acute needs and unlock efficiency. 13 Mar 2023. Research & Ideas.
Lastly, this paper will enrich the existing literature dealing with the topics of Lean Management in the Healthcare sector, bringing a successful case study in which the implementation of the Lean techniques is addressed through the use of the A3 methodology. This paper also has some limitations that need to be remarked on and explained here.
None of the early M-Health applications are designed for case management care services. This study aims to describe the process of developing a M-health component for the case management model in breast cancer transitional care and to highlight methods for solving the common obstacles faced during the application of M-health nursing service. We followed a four-step process: (a) Forming a cross ...
Intensive Care Unit (ICU) capacity management is essential to provide high-quality healthcare for critically ill patients. Yet, consensus on the most favorable ICU design is lacking, especially whether ICUs should deliver dedicated or non-dedicated care. The decision for dedicated or non-dedicated ICU design considers a trade-off in the degree of specialization for individual patient care and ...
Reorienting health systems through a primary health care (PHC) lens is the best way to advance the goal of affordable health care for all. However, the realization of this vision hinges upon both political leadership and financial commitment to put the evidence into practice. This was emphasized by PHC experts during a side event of the 77th World Health Assembly in Geneva on 27 May 2024.The ...
• Microsoft's DAX Copilot is a good case study of AI as a healthcare copilot, after its Nuance acquisition. DAX leverages voice-activated queries to relieve clinicians from the administrative ...
A case study in the challenges facing health care. In 2023, the top six health insurers collectively earned over one trillion dollars in revenue, a staggering figure that has raised questions about whether the current healthcare dynamic is sustainable and serving all stakeholders effectively. There's no question that health insurance provides a ...
Introduction. Case management, also known as care coordination is a complex integrated health and social care intervention and makes a unique contribution to the health, social care and participation of people with complex health conditions.[1,2,3,4].In the 1960's case management emerged in response to the de-institutionalisation of large numbers of people with severe mental health ...
The role of data management systems "Translational medicine requires sophisticated data management systems that act less like a map and more like a compass," explains Dr. Augustine Annan, PhD, a Senior Data Scientist at IMO Health.. His analogy underscores the navigational challenges faced by healthcare professionals who must steer through vast amounts of complex biological data to find ...
Health Care Home State/Federal Funded Programs Affordable Care Act HRSA-Supported Health Centers Mental Health Parity Act Tricare. Assistive Devices ; My Account . My Account Dashboard Events Favorites My PHR Messages Emergency Card Care Coordination Card Visitor Access Manage Profile Change Password.
The good news is that security investments tend to pay off. The same IBM report found that organizations who use security AI and automation identify and contain breaches in 108 fewer days (on average). In addition, their data breach costs are USD 1.76 million lower. In this article, we'll look at the case study of the medical manufacturer MediTouch and explore best practices for healthcare ...
Leading Healthcare Innovation, Education, Collaboration at the 2024 HIMSS Global Health Conference and Exhibition. Operations. Informa Markets and HIMSS Join Forces to Expand the HIMSS Global Health Conference & Exhibition, the Leading Healthcare Technology Show in the U.S. Digital Health. Celebrating the 2023 HIMSS Changemaker in Health Award ...
As you age, you may notice changes that affect your eyes and vision. Common age-related problems include presbyopia, glaucoma, dry eyes, cataracts and age-related macular degeneration. Eye specialists can maintain or correct your vision or slow the symptoms of severe disease. Regular exams protect your eye health as you age.