- Reference Manager
- Simple TEXT file

People also looked at
Hypothesis and theory article, type 2 diabetes mellitus: a pathophysiologic perspective.

- Department of Medicine, Duke University, Durham, NC, United States
Type 2 Diabetes Mellitus (T2DM) is characterized by chronically elevated blood glucose (hyperglycemia) and elevated blood insulin (hyperinsulinemia). When the blood glucose concentration is 100 milligrams/deciliter the bloodstream of an average adult contains about 5–10 grams of glucose. Carbohydrate-restricted diets have been used effectively to treat obesity and T2DM for over 100 years, and their effectiveness may simply be due to lowering the dietary contribution to glucose and insulin levels, which then leads to improvements in hyperglycemia and hyperinsulinemia. Treatments for T2DM that lead to improvements in glycemic control and reductions in blood insulin levels are sensible based on this pathophysiologic perspective. In this article, a pathophysiological argument for using carbohydrate restriction to treat T2DM will be made.
Introduction
Type 2 Diabetes Mellitus (T2DM) is characterized by a persistently elevated blood glucose, or an elevation of blood glucose after a meal containing carbohydrate ( 1 ) ( Table 1 ). Unlike Type 1 Diabetes which is characterized by a deficiency of insulin, most individuals affected by T2DM have elevated insulin levels (fasting and/or post glucose ingestion), unless there has been beta cell failure ( 2 , 3 ). The term “insulin resistance” (IR) has been used to explain why the glucose levels remain elevated even though there is no deficiency of insulin ( 3 , 4 ). Attempts to determine the etiology of IR have involved detailed examinations of molecular and intracellular pathways, with attribution of cause to fatty acid flux, but the root cause has been elusive to experts ( 5 – 7 ).
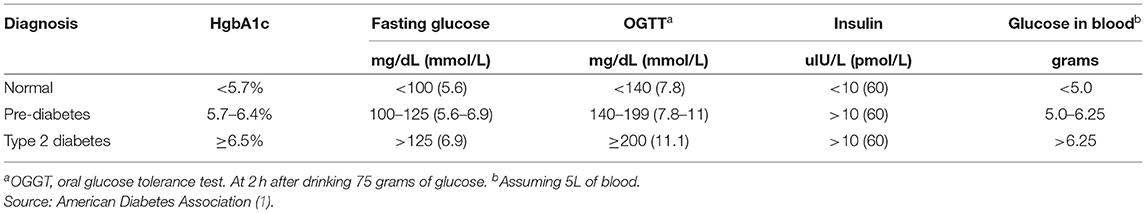
Table 1 . Definition of type 2 diabetes mellitus.
How Much Glucose Is in the Blood?
Keeping in mind that T2DM involves an elevation of blood glucose, it is important to understand how much glucose is in the blood stream to begin with, and then the factors that influence the blood glucose—both exogenous and endogenous factors. The amount of glucose in the bloodstream is carefully controlled—approximately 5–10 grams in the bloodstream at any given moment, depending upon the size of the person. To calculate this, multiply 100 milligrams/deciliter × 1 gram/1,000 milligrams × 10 deciliters/1 liter × 5 liters of blood. The “zeros cancel” and you are left with 5 grams of glucose if the individual has 5 liters of blood. Since red blood cells represent about 40% of the blood volume, and the glucose is in equilibrium, there may be an extra 40% glucose because of the red blood cell reserve ( 8 ). Adding the glucose from the serum and red blood cells totals about 5–10 grams of glucose in the entire bloodstream.
Major Exogenous Factors That Raise the Blood Glucose
Dietary carbohydrate is the major exogenous factor that raises the blood glucose. When one considers that it is common for an American in 2021 to consume 200–300 grams of carbohydrate daily, and most of this carbohydrate is digested and absorbed as glucose, the body absorbs and delivers this glucose via the bloodstream to the cells while attempting to maintain a normal blood glucose level. Thinking of it in this way, if 200–300 grams of carbohydrates is consumed in a day, the bloodstream that holds 5–10 grams of glucose and has a concentration of 100 milligrams/deciliter, is the conduit through which 200,000–300,000 milligrams (200 grams = 200,000 milligrams) passes over the course of a day.
Major Endogenous Factors That Raise the Blood Glucose
There are many endogenous contributors that raise the blood glucose. There are at least 3 different hormones that increase glucose levels: glucagon, epinephrine, and cortisol. These hormones increase glucose levels by increasing glycogenolysis and gluconeogenesis ( 9 ). Without any dietary carbohydrate, the normal human body can generate sufficient glucose though the mechanism of glucagon secretion, gluconeogenesis, glycogen storage and glycogenolysis ( 10 ).
Major Exogenous Factors That Lower the Blood Glucose
A reduction in dietary carbohydrate intake can lower the blood glucose. An increase in activity or exercise usually lowers the blood glucose ( 11 ). There are many different medications, employing many mechanisms to lower the blood glucose. Medications can delay sucrose and starch absorption (alpha-glucosidase inhibitors), slow gastric emptying (GLP-1 agonists, DPP-4 inhibitors) enhance insulin secretion (sulfonylureas, meglitinides, GLP-1 agonists, DPP-4 inhibitors), reduce gluconeogenesis (biguanides), reduce insulin resistance (biguanides, thiazolidinediones), and increase urinary glucose excretion (SGLT-2 inhibitors). The use of medications will also have possible side effects.
Major Endogenous Factors That Lower the Blood Glucose
The major endogenous mechanism to lower the blood glucose is to deliver glucose into the cells (all cells can use glucose). If the blood glucose exceeds about 180 milligrams/deciliter, then loss of glucose into the urine can occur. The blood glucose is reduced by cellular uptake using glut transporters ( 12 ). Some cells have transporters that are responsive to the presence of insulin to activate (glut4), others have transporters that do not require insulin for activation. Insulin-responsive glucose transporters in muscle cells and adipose cells lead to a reduction in glucose levels—especially after carbohydrate-containing meals ( 13 ). Exercise can increase the glucose utilization in muscle, which then increases glucose cellular uptake and reduce the blood glucose levels. During exercise, when the metabolic demands of skeletal muscle can increase more than 100-fold, and during the absorptive period (after a meal), the insulin-responsive glut4 transporters facilitate the rapid entry of glucose into muscle and adipose tissue, thereby preventing large fluctuations in blood glucose levels ( 13 ).
Which Cells Use Glucose?
Glucose can used by all cells. A limited number of cells can only use glucose, and are “glucose-dependent.” It is generally accepted that the glucose-dependent cells include red blood cells, white blood cells, and cells of the renal papilla. Red blood cells have no mitochondria for beta-oxidation, so they are dependent upon glucose and glycolysis. White blood cells require glucose for the respiratory burst when fighting infections. The cells of the inner renal medulla (papilla) are under very low oxygen tension, so therefore must predominantly use glucose and glycolysis. The low oxygen tension is a result of the countercurrent mechanism of urinary concentration ( 14 ). These glucose-dependent cells have glut transporters that do not require insulin for activation—i.e., they do not need insulin to get glucose into the cells. Some cells can use glucose and ketones, but not fatty acids. The central nervous system is believed to be able to use glucose and ketones for fuel ( 15 ). Other cells can use glucose, ketones, and fatty acids for fuel. Muscle, even cardiac muscle, functions well on fatty acids and ketones ( 16 ). Muscle cells have both non-insulin-responsive and insulin-responsive (glut4) transporters ( 12 ).
Possible Dual Role of an Insulin-Dependent Glucose-Transporter (glut4)
A common metaphor is to think of the insulin/glut transporter system as a key/lock mechanism. Common wisdom states that the purpose of insulin-responsive glut4 transporters is to facilitate glucose uptake when blood insulin levels are elevated. But, a lock serves two purposes: to let someone in and/or to keep someone out . So, one of the consequences of the insulin-responsive glut4 transporter is to keep glucose out of the muscle and adipose cells, too, when insulin levels are low. The cells that require glucose (“glucose-dependent”) do not need insulin to facilitate glucose entry into the cell (non-insulin-responsive transporters). In a teleological way, it would “make no sense” for cells that require glucose to have insulin-responsive glut4 transporters. Cells that require glucose have glut1, glut2, glut3, glut5 transporters—none of which are insulin-responsive (Back to the key/lock metaphor, it makes no sense to have a lock on a door that you want people to go through). At basal (low insulin) conditions, most glucose is used by the brain and transported by non-insulin-responsive glut1 and glut3. So, perhaps one of the functions of the insulin-responsive glucose uptake in muscle and adipose to keep glucose OUT of the these cells at basal (low insulin) conditions, so that the glucose supply can be reserved for the tissue that is glucose-dependent (blood cells, renal medulla).
What Causes IR and T2DM?
The current commonly espoused view is that “Type 2 diabetes develops when beta-cells fail to secrete sufficient insulin to keep up with demand, usually in the context of increased insulin resistance.” ( 17 ). Somehow, the beta cells have failed in the face of insulin resistance. But what causes insulin resistance? When including the possibility that the environment may be part of the problem, is it possible that IR is an adaptive (protective) response to excess glucose availability? From the perspective that carbohydrate is not an essential nutrient and the change in foods in recent years has increased the consumption of refined sugar and flour, maybe hyperinsulinemia is the cause of IR and T2DM, as cells protect themselves from excessive glucose and insulin levels.
Insulin Is Already Elevated in IR and T2DM
Clinical experience of most physicians using insulin to treat T2DM over time informs us that an escalation of insulin dose is commonly needed to achieve glycemic control (when carbohydrate is consumed). When more insulin is given to someone with IR, the IR seems to get worse and higher levels of insulin are needed. I have the clinical experience of treating many individuals affected by T2DM and de-prescribing insulin as it is no longer needed after consuming a diet without carbohydrate ( 18 ).
Diets Without Carbohydrate Reverse IR and T2DM
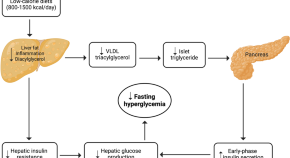
When dietary manipulation was the only therapy for T2DM, before medications were available, a carbohydrate-restricted diet was used to treat T2DM ( 19 – 21 ). Clinical experience of obesity medicine physicians and a growing number of recent studies have demonstrated that carbohydrate-restricted diets reverse IR and T2DM ( 18 , 22 , 23 ). Other methods to achieve caloric restriction also have these effects, like calorie-restricted diets and bariatric surgery ( 24 , 25 ). There may be many mechanisms by which these approaches may work: a reduction in glucose, a reduction in insulin, nutritional ketosis, a reduction in metabolic syndrome, or a reduction in inflammation ( 26 ). Though there may be many possible mechanisms, let's focus on an obvious one: a reduction in blood glucose. Let's assume for a moment that the excessive glucose and insulin leads to hyperinsulinemia and this is the cause of IR. On a carbohydrate-restricted diet, the reduction in blood glucose leads to a reduction in insulin. The reduction in insulin leads to a reduction in insulin resistance. The reduction in insulin leads to lipolysis. The resulting lowering of blood glucose, insulin and body weight reverses IR, T2DM, AND obesity. These clinical observations strongly suggest that hyperinsulinemia is a cause of IR and T2DM—not the other way around.
What Causes Atherosclerosis?
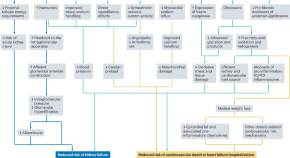
For many years, the metabolic syndrome has been described as a possible cause of atherosclerosis, but there are no RCTs directly targeting metabolic syndrome, and the current drug treatment focuses on LDL reduction, so its importance remains controversial. A recent paper compared the relative importance of many risk factors in the prediction of the first cardiac event in women, and the most powerful predictors were diabetes, metabolic syndrome, smoking, hypertension and BMI ( 27 ). The connection between dietary carbohydrate and fatty liver is well-described ( 28 ). The connection between fatty liver and atherosclerosis is well-described ( 29 ). It is very possible that the transport of excess glucose to the adipose tissue via lipoproteins creates the particles that cause the atherosclerotic damage (small LDL) ( Figure 1 ) ( 30 – 32 ). This entire process of dietary carbohydrate leading to fatty liver, leading to small LDL, is reversed by a diet without carbohydrate ( 26 , 33 , 34 ).
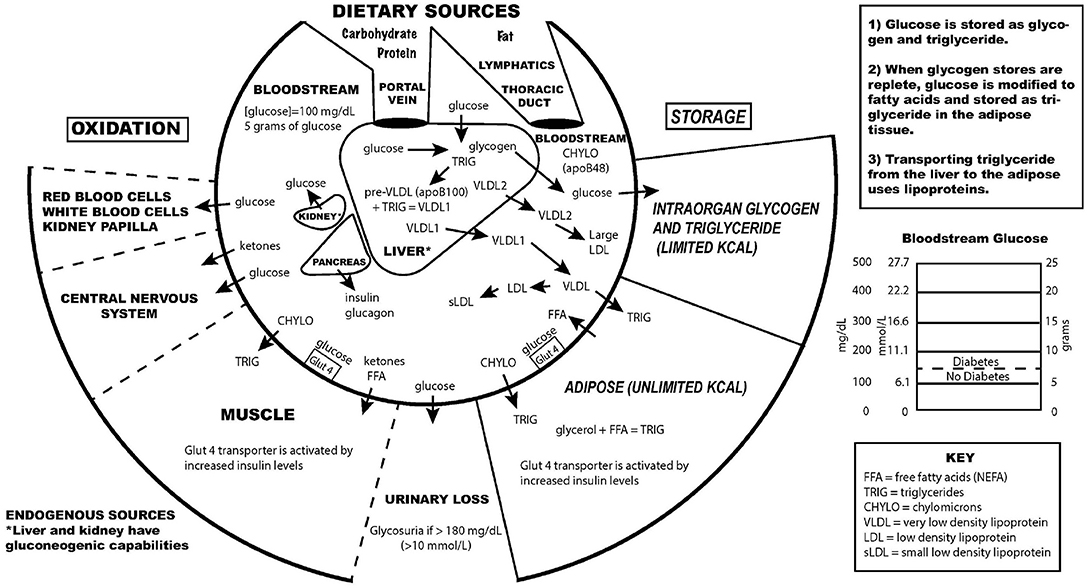
Figure 1 . Key aspects of the interconnection between glucose and lipoprotein metabolism.
Reducing dietary carbohydrate in the context of a low carbohydrate, ketogenic diet reduces hyperglycemia and hyperinsulinemia, IR and T2DM. In the evaluation of an individual for a glucose abnormality, measure the blood glucose and insulin levels. If the insulin level (fasting or after a glucose-containing meal) is high, do not give MORE insulin—instead, use an intervention to lower the insulin levels. Effective ways to reduce insulin resistance include lifestyle, medication, and surgical therapies ( 23 , 35 ).
The search for a single cause of a complex problem is fraught with difficulty and controversy. I am not hypothesizing that excessive dietary carbohydrate is the only cause of IR and T2DM, but that it is a cause, and quite possibly the major cause. How did such a simple explanation get overlooked? I believe it is very possible that the reductionistic search for intracellular molecular mechanisms of IR and T2DM, the emphasis on finding pharmaceutical (rather than lifestyle) treatments, the emphasis on the treatment of high total and LDL cholesterol, and the fear of eating saturated fat may have misguided a generation of researchers and clinicians from the simple answer that dietary carbohydrate, when consumed chronically in amounts that exceeds an individual's ability to metabolize them, is the most common cause of IR, T2DM and perhaps even atherosclerosis.
While there has historically been a concern about the role of saturated fat in the diet as a cause of heart disease, most nutritional experts now cite the lack of evidence implicating dietary saturated fat as the reason for lack of concern of it in the diet ( 36 ).
The concept of comparing medications that treat IR by insulin-sensitizers or by providing insulin itself was tested in the Bari-2D study ( 37 ). Presumably in the context of consuming a standard American diet, this study found no significant difference in death rates or major cardiovascular events between strategies of insulin sensitization or insulin provision.
While lifestyle modification may be ideal to prevent or cure IR and T2DM, for many people these changes are difficult to learn and/or maintain. Future research should be directed toward improving adherence to all effective lifestyle or medication treatments. Future research is also needed to assess the effect of carbohydrate restriction on primary or secondary prevention of outcomes of cardiovascular disease.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author Contributions
The author confirms being the sole contributor of this work and has approved it for publication.
Conflict of Interest
EW receives royalties from popular diet books and is founder of a company based on low-carbohydrate diet principles (Adapt Your Life, Inc.).
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. American Diabetes Association. Classification and diagnosis of diabetes. Diabetes Care . (2016) 39 (Suppl. 1):S13–22. doi: 10.2337/dc16-S005
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Bogardus C, Lillioja S, Howard BV, Reaven G, Mott D. Relationships between insulin secretion, insulin action, and fasting plasma glucose concentration in nondiabetic and noninsulin-dependent diabetic subjects. J Clin Invest. (1984) 74:1238–46. doi: 10.1172/JCI111533
3. Reaven GM. Compensatory hyperinsulinemia and the development of an atherogenic lipoprotein profile: the price paid to maintain glucose homeostasis in insulin-resistant individuals. Endocrinol Metab Clin North Am. (2005) 34:49–62. doi: 10.1016/j.ecl.2004.12.001
4. DeFronzo RA, Ferrannini E. Insulin resistance. A multifaceted syndrome responsible for NIDDM, obesity, hypertension, dyslipidemia, and atherosclerotic cardiovascular disease. Diabetes Care. (1991) 14:173–94. doi: 10.2337/diacare.14.3.173
5. Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. (2005) 365:1415–28. doi: 10.1016/S0140-6736(05)66378-7
6. Yaribeygi H, Farrokhi FR, Butler AE, Sahebkar A. Insulin resistance: review of the underlying molecular mechanisms. J Cell Physiol. (2019) 234:8152–61. doi: 10.1002/jcp.27603
7. Shulman GI. Cellular mechanisms of insulin resistance. J Clin Invest. (2000) 106:171–6. doi: 10.1172/JCI10583
8. Guizouarn H, Allegrini B. Erythroid glucose transport in health and disease. Pflugers Arch. (2020) 472:1371–83. doi: 10.1007/s00424-020-02406-0
9. Petersen MC, Vatner DF, Shulman GI. Regulation of hepatic glucose metabolism in health and disease. Nat Rev Endocrinol. (2017) 13:572–87. doi: 10.1038/nrendo.2017.80
10. Tondt J, Yancy WS, Westman EC. Application of nutrient essentiality criteria to dietary carbohydrates. Nutr Res Rev. (2020) 33:260–70. doi: 10.1017/S0954422420000050
11. Colberg SR, Hernandez MJ, Shahzad F. Blood glucose responses to type, intensity, duration, and timing of exercise. Diabetes Care. (2013) 36:e177. doi: 10.2337/dc13-0965
12. Mueckler M, Thorens B. The SLC2 (GLUT) family of membrane transporters. Mol Aspects Med. (2013) 34:121–38. doi: 10.1016/j.mam.2012.07.001
13. Bryant NJ, Govers R, James DE. Regulated transport of the glucose transporter GLUT4. Nat Rev Mol Cell Biol. (2002) 3:267–77. doi: 10.1038/nrm782
14. Epstein FH. Oxygen and renal metabolism. Kidney Int. (1997) 51:381–5. doi: 10.1038/ki.1997.50
15. Cahill GF. Fuel metabolism in starvation. Annu Rev Nutr. (2006) 26:1–22. doi: 10.1146/annurev.nutr.26.061505.111258
16. Murashige D, Jang C, Neinast M, Edwards JJ, Cowan A, Hyman MC, et al. Comprehensive quantification of fuel use by the failing and nonfailing human heart. Science. (2020) 370:364–8. doi: 10.1126/science.abc8861
17. Skyler JS, Bakris GL, Bonifacio E, Darsow T, Eckel RH, Groop L, et al. Differentiation of diabetes by pathophysiology, natural history, and prognosis. Diabetes. (2017) 66:241–55. doi: 10.2337/db16-0806
18. Westman EC, Yancy WS, Mavropoulos JC, Marquart M, McDuffie JR. The effect of a low-carbohydrate, ketogenic diet versus a low-glycemic index diet on glycemic control in type 2 diabetes mellitus. Nutr Metab. (2008) 5:36. doi: 10.1186/1743-7075-5-36
CrossRef Full Text | Google Scholar
19. Allen F. The treatment of diabetes. Boston Med Surg J. (1915) 172:241–7. doi: 10.1056/NEJM191502181720702
20. Osler W, McCrae T. The Principles and Practice of Medicine . 9th ed. New York and London: Appleton & Company (1923).
21. Lennerz BS, Koutnik AP, Azova S, Wolfsdorf JI, Ludwig DS. Carbohydrate restriction for diabetes: rediscovering centuries-old wisdom. J Clin Invest. (2021) 131:e142246. doi: 10.1172/JCI142246
22. Steelman GM, Westman EC. Obesity: Evaluation and Treatment Essentials . 2nd ed. Boca Raton: CRC Press, Taylor & Francis Group (2016). 340 p.
23. Athinarayanan SJ, Adams RN, Hallberg SJ, McKenzie AL, Bhanpuri NH, Campbell WW, et al. Long-term effects of a novel continuous remote care intervention including nutritional ketosis for the management of type 2 diabetes: a 2-year non-randomized clinical trial. Front Endocrinol. (2019) 10:348. doi: 10.3389/fendo.2019.00348
24. Lim EL, Hollingsworth KG, Aribisala BS, Chen MJ, Mathers JC, Taylor R. Reversal of type 2 diabetes: normalisation of beta cell function in association with decreased pancreas and liver triacylglycerol. Diabetologia. (2011) 54:2506–14. doi: 10.1007/s00125-011-2204-7
25. Isbell JM, Tamboli RA, Hansen EN, Saliba J, Dunn JP, Phillips SE, et al. The importance of caloric restriction in the early improvements in insulin sensitivity after Roux-en-Y gastric bypass surgery. Diabetes Care. (2010) 33:1438–42. doi: 10.2337/dc09-2107
26. Bhanpuri NH, Hallberg SJ, Williams PT, McKenzie AL, Ballard KD, Campbell WW, et al. Cardiovascular disease risk factor responses to a type 2 diabetes care model including nutritional ketosis induced by sustained carbohydrate restriction at 1 year: an open label, non-randomized, controlled study. Cardiovasc Diabetol. (2018) 17:56. doi: 10.1186/s12933-018-0698-8
27. Dugani SB, Moorthy MV, Li C, Demler OV, Alsheikh-Ali AA, Ridker PM, et al. Association of lipid, inflammatory, and metabolic biomarkers with age at onset for incident coronary heart disease in women. JAMA Cardiol. (2021) 6:437–47. doi: 10.1001/jamacardio.2020.7073
28. Duwaerts CC, Maher JJ. Macronutrients and the adipose-liver axis in obesity and fatty liver. Cell Mol Gastroenterol Hepatol. (2019) 7:749–61. doi: 10.1016/j.jcmgh.2019.02.001
29. Zhang L, She Z-G, Li H, Zhang X-J. Non-alcoholic fatty liver disease: a metabolic burden promoting atherosclerosis. Clin Sci Lond Engl. (1979) 134:1775–99. doi: 10.1042/CS20200446
30. Horton TJ, Drougas H, Brachey A, Reed GW, Peters JC, Hill JO. Fat and carbohydrate overfeeding in humans: different effects on energy storage. Am J Clin Nutr. (1995) 62:19–29. doi: 10.1093/ajcn/62.1.19
31. Packard C, Caslake M, Shepherd J. The role of small, dense low density lipoprotein (LDL): a new look. Int J Cardiol. (2000) 74 (Suppl. 1):S17–22. doi: 10.1016/S0167-5273(99)00107-2
32. Borén J, Chapman MJ, Krauss RM, Packard CJ, Bentzon JF, Binder CJ, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease: pathophysiological, genetic, and therapeutic insights: a consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J. (2020) 41:2313–30. doi: 10.1093/eurheartj/ehz962
33. Yancy WS, Olsen MK, Guyton JR, Bakst RP, Westman EC. A low-carbohydrate, ketogenic diet versus a low-fat diet to treat obesity and hyperlipidemia: a randomized, controlled trial. Ann Intern Med. (2004) 140:769. doi: 10.7326/0003-4819-140-10-200405180-00006
34. Tendler D, Lin S, Yancy WS, Mavropoulos J, Sylvestre P, Rockey DC, et al. The effect of a low-carbohydrate, ketogenic diet on nonalcoholic fatty liver disease: a pilot study. Dig Dis Sci. (2007) 52:589–93. doi: 10.1007/s10620-006-9433-5
35. Pories WJ, Swanson MS, MacDonald KG, Long SB, Morris PG, Brown BM, et al. Who would have thought it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann Surg. (1995) 222:339–50. doi: 10.1097/00000658-199509000-00011
36. Astrup A, Magkos F, Bier DM, Brenna JT, de Oliveira Otto MC, Hill JO, et al. Saturated fats and health: a reassessment and proposal for food-based recommendations: JACC state-of-the-art review. J Am Coll Cardiol. (2020) 76:844–57. doi: 10.1016/j.jacc.2020.05.077
37. A randomized trial of therapies for type 2 diabetes and coronary artery disease. N Engl J Med . (2009) 360:2503–15. doi: 10.1056/NEJMoa0805796
Keywords: type 2 diabetes, insulin resistance, pre-diabetes, carbohydrate-restricted diets, hyperinsulinemia, hyperglycemia
Citation: Westman EC (2021) Type 2 Diabetes Mellitus: A Pathophysiologic Perspective. Front. Nutr. 8:707371. doi: 10.3389/fnut.2021.707371
Received: 09 May 2021; Accepted: 20 July 2021; Published: 10 August 2021.
Reviewed by:
Copyright © 2021 Westman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Eric C. Westman, ewestman@duke.edu
This article is part of the Research Topic
Carbohydrate-restricted Nutrition and Diabetes Mellitus
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
Type 2 diabetes articles from across Nature Portfolio
Type 2 diabetes mellitus, the most frequent subtype of diabetes, is a disease characterized by high levels of blood glucose (hyperglycaemia). It arises from a resistance to and relative deficiency of the pancreatic β-cell hormone insulin.
Latest Research and Reviews
Urinary non-albumin protein-creatinine ratio is an independent predictor of mortality in patients with type 2 diabetes: a retrospective cohort study
- Yu-Cheng Cheng

The proteomic profile is altered but not repaired after bariatric surgery in type 2 diabetes pigs
- Karolina Ferenc
- Michał Marcinkowski
- Romuald Zabielski

Galectin-3 impairs calcium transients and β-cell function
Galectin-3, mainly produced and secreted by macrophages, is elevated in diabetes. Here, the authors show that galectin-3 directly interacts with voltage-gated channel auxiliary subunit gamma 1 (CACNG1) and blocks calcium transients and subsequent insulin secretion.
- Pingping Li
Effectiveness of DialBetesPlus, a self-management support system for diabetic kidney disease: Randomized controlled trial
- Mitsuhiko Nara
- Kazuhiko Ohe
Applications of SGLT2 inhibitors beyond glycaemic control
Here, the authors discuss the beneficial effects of sodium–glucose cotransporter 2 (SGLT2) inhibitors for a range of clinical outcomes beyond glucose lowering, including kidney and cardiovascular protection. They also discuss the need for implementation and adherence initiatives to help translate the benefits of these agents into real-world clinical outcomes.
- Daniel V. O’Hara
- Carolyn S. P. Lam
- Meg J. Jardine
Folic acid supplementation on inflammation and homocysteine in type 2 diabetes mellitus: systematic review and meta-analysis of randomized controlled trials
- Kabelo Mokgalaboni
- Given. R. Mashaba
- Sogolo. L. Lebelo
News and Comment
Response to comment on “credibility of chat-gpt in the assessment of obesity in type 2 diabetes according to the guidelines”.
- Tugba Barlas
- Alev Eroglu Altinova
- Fusun Balos Toruner


Macrophage vesicles in antidiabetic drug action
Thiazolidinediones (TZDs) are potent insulin-sensitizing drugs, but their use is accompanied by adverse side-effects. Rohm et al. now report that TZD-stimulated macrophages release miR-690-containing vesicles that improve insulin sensitization and bypass unwanted side-effects.
- Rinke Stienstra
- Eric Kalkhoven
Metformin acts through appetite-suppressing metabolite: Lac-Phe
- Shimona Starling
Slowly progressive insulin-dependent diabetes mellitus in type 1 diabetes endotype 2
- Tetsuro Kobayashi
- Takashi Kadowaki

Metformin induces a Lac-Phe gut–brain signalling axis
The mechanism by which metformin affects food intake remains controversial. Now, two studies link metformin treatment with the induction of the appetite-suppressing metabolite N -lactoyl-phenylalanine, which is produced by the intestine.
- Tara TeSlaa
Low-calorie diets for people with isolated impaired fasting glucose
Thirunavukkarasu et al. discuss how standard lifestyle interventions prove ineffective in preventing type 2 diabetes in individuals with isolated impaired fasting glucose, a highly prevalent prediabetes phenotype globally. They propose low-calorie diets as a promising strategy for diabetes prevention in this high-risk population.
- Sathish Thirunavukkarasu
- Jonathan E. Shaw
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

- Previous Article
- Next Article
Research Design and Methods
Article information, literature review of type 2 diabetes management and health literacy.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Cite Icon Cite
- Get Permissions
Rulla Alsaedi , Kimberly McKeirnan; Literature Review of Type 2 Diabetes Management and Health Literacy. Diabetes Spectr 1 November 2021; 34 (4): 399–406. https://doi.org/10.2337/ds21-0014
Download citation file:
- Ris (Zotero)
- Reference Manager
The purpose of this literature review was to identify educational approaches addressing low health literacy for people with type 2 diabetes. Low health literacy can lead to poor management of diabetes, low engagement with health care providers, increased hospitalization rates, and higher health care costs. These challenges can be even more profound among minority populations and non-English speakers in the United States.
A literature search and standard data extraction were performed using PubMed, Medline, and EMBASE databases. A total of 1,914 articles were identified, of which 1,858 were excluded based on the inclusion criteria, and 46 were excluded because of a lack of relevance to both diabetes management and health literacy. The remaining 10 articles were reviewed in detail.
Patients, including ethnic minorities and non-English speakers, who are engaged in diabetes education and health literacy improvement initiatives and ongoing follow-up showed significant improvement in A1C, medication adherence, medication knowledge, and treatment satisfaction. Clinicians considering implementing new interventions to address diabetes care for patients with low health literacy can use culturally tailored approaches, consider ways to create materials for different learning styles and in different languages, engage community health workers and pharmacists to help with patient education, use patient-centered medication labels, and engage instructors who share cultural and linguistic similarities with patients to provide educational sessions.
This literature review identified a variety of interventions that had a positive impact on provider-patient communication, medication adherence, and glycemic control by promoting diabetes self-management through educational efforts to address low health literacy.
Diabetes is the seventh leading cause of death in the United States, and 30.3 million Americans, or 9.4% of the U.S. population, are living with diabetes ( 1 , 2 ). For successful management of a complicated condition such as diabetes, health literacy may play an important role. Low health literacy is a well-documented barrier to diabetes management and can lead to poor management of medical conditions, low engagement with health care providers (HCPs), increased hospitalizations, and, consequently, higher health care costs ( 3 – 5 ).
The Healthy People 2010 report ( 6 ) defined health literacy as the “degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.” Diabetes health literacy also encompasses a wide range of skills, including basic knowledge of the disease state, self-efficacy, glycemic control, and self-care behaviors, which are all important components of diabetes management ( 3 – 5 , 7 ). According to the Institute of Medicine’s Committee on Health Literacy, patients with poor health literacy are twice as likely to have poor glycemic control and were found to be twice as likely to be hospitalized as those with adequate health literacy ( 8 ). Associations between health literacy and health outcomes have been reported in many studies, the first of which was conducted in 1995 in two public hospitals and found that many patients had inadequate health literacy and could not perform the basic reading tasks necessary to understand their treatments and diagnoses ( 9 ).
Evaluation of health literacy is vital to the management and understanding of diabetes. Several tools for assessing health literacy have been evaluated, and the choice of which to use depends on the length of the patient encounter and the desired depth of the assessment. One widely used literacy assessment tool, the Test of Functional Health Literacy in Adults (TOFHLA), consists of 36 comprehension questions and four numeric calculations ( 10 ). Additional tools that assess patients’ reading ability include the Rapid Estimate of Adult Literacy in Medicine (REALM) and the Literacy Assessment for Diabetes. Tests that assess diabetes numeracy skills include the Diabetes Numeracy Test, the Newest Vital Sign (NVS), and the Single-Item Literacy Screener (SILS) ( 11 ).
Rates of both diabetes and low health literacy are higher in populations from low socioeconomic backgrounds ( 5 , 7 , 12 ). People living in disadvantaged communities face many barriers when seeking health care, including inconsistent housing, lack of transportation, financial difficulties, differing cultural beliefs about health care, and mistrust of the medical professions ( 13 , 14 ). People with high rates of medical mistrust tend to be less engaged in their care and to have poor communication with HCPs, which is another factor HCPs need to address when working with their patients with diabetes ( 15 ).
The cost of medical care for people with diabetes was $327 billion in 2017, a 26% increase since 2012 ( 1 , 16 ). Many of these medical expenditures are related to hospitalization and inpatient care, which accounts for 30% of total medical costs for people with diabetes ( 16 ).
People with diabetes also may neglect self-management tasks for various reasons, including low health literacy, lack of diabetes knowledge, and mistrust between patients and HCPs ( 7 , 15 ).
These challenges can be even more pronounced in vulnerable populations because of language barriers and patient-provider mistrust ( 17 – 19 ). Rates of diabetes are higher among racial and ethnic minority groups; 15.1% of American Indians and Alaskan Natives, 12.7% of Non-Hispanic Blacks, 12.1% of Hispanics, and 8% of Asian Americans have diagnosed diabetes, compared with 7.4% of non-Hispanic Whites ( 1 ). Additionally, patient-provider relationship deficits can be attributed to challenges with communication, including HCPs’ lack of attention to speaking slowly and clearly and checking for patients’ understanding when providing education or gathering information from people who speak English as a second language ( 15 ). White et al. ( 15 ) demonstrated that patients with higher provider mistrust felt that their provider’s communication style was less interpersonal and did not feel welcome as part of the decision-making process.
To the authors’ knowledge, there is no current literature review evaluating interventions focused on health literacy and diabetes management. There is a pressing need for such a comprehensive review to provide a framework for future intervention design. The objective of this literature review was to gather and summarize studies of health literacy–based diabetes management interventions and their effects on overall diabetes management. Medication adherence and glycemic control were considered secondary outcomes.
Search Strategy
A literature review was conducted using the PubMed, Medline, and EMBASE databases. Search criteria included articles published between 2015 and 2020 to identify the most recent studies on this topic. The search included the phrases “diabetes” and “health literacy” to specifically focus on health literacy and diabetes management interventions and was limited to original research conducted in humans and published in English within the defined 5-year period. Search results were exported to Microsoft Excel for evaluation.
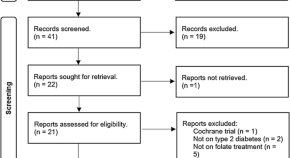
Study Selection
Initial screening of the articles’ abstracts was conducted using the selection criteria to determine which articles to include or exclude ( Figure 1 ). The initial search results were reviewed for the following inclusion criteria: original research (clinical trials, cohort studies, and cross-sectional studies) conducted in human subjects with type 2 diabetes in the United States, and published in English between 2015 and 2020. Articles were considered to be relevant if diabetes was included as a medical condition in the study and an intervention was made to assess or improve health literacy. Studies involving type 1 diabetes or gestational diabetes and articles that were viewpoints, population surveys, commentaries, case reports, reviews, or reports of interventions conducted outside of the United States were excluded from further review. The criteria requiring articles to be from the past 5 years and from the United States were used because of the unique and quickly evolving nature of the U.S. health care system. Articles published more than 5 years ago or from other health care systems may have contributed information that was not applicable to or no longer relevant for HCPs in the United States. Articles were screened and reviewed independently by both authors. Disagreements were resolved through discussion to create the final list of articles for inclusion.
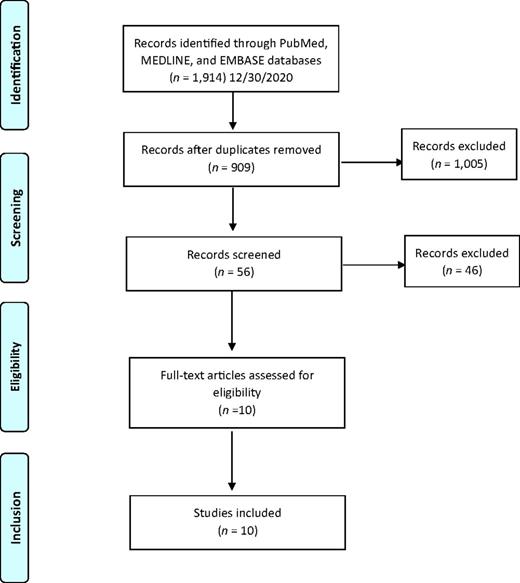
PRISMA diagram of the article selection process.
Data Extraction
A standard data extraction was performed for each included article to obtain information including author names, year of publication, journal, study design, type of intervention, primary outcome, tools used to assess health literacy or type 2 diabetes knowledge, and effects of intervention on overall diabetes management, glycemic control, and medication adherence.
A total of 1,914 articles were collected from a search of the PubMed, MEDLINE, and EMBASE databases, of which 1,858 were excluded based on the inclusion and exclusion criteria. Of the 56 articles that met criteria for abstract review, 46 were excluded because of a lack of relevance to both diabetes management and health literacy. The remaining 10 studies identified various diabetes management interventions, including diabetes education tools such as electronic medication instructions and text message–based interventions, technology-based education videos, enhanced prescription labels, learner-based education materials, and culturally tailored interventions ( 15 , 20 – 28 ). Figure 1 shows the PRISMA diagram of the article selection process, and Table 1 summarizes the findings of the article reviews ( 15 , 20 – 28 ).
Findings of the Article Reviews (15,20–28)
SAHLSA, Short Assessment of Health Literacy for Spanish Adults.
Medical mistrust and poor communication are challenging variables in diabetes education. White et al. ( 15 ) examined the association between communication quality and medical mistrust in patients with type 2 diabetes. HCPs at five health department clinics received training in effective health communication and use of the PRIDE (Partnership to Improve Diabetes Education) toolkit in both English and Spanish, whereas control sites were only exposed to National Diabetes Education Program materials without training in effective communication. The study evaluated participant communication using several tools, including the Communication Assessment Tool (CAT), Interpersonal Processes of Care (IPC-18), and the Short Test of Functional Health Literacy in Adults (s-TOFHLA). The authors found that higher levels of mistrust were associated with lower CAT and IPC-18 scores.
Patients with type 2 diabetes are also likely to benefit from personalized education delivery tools such as patient-centered labeling (PCL) of prescription drugs, learning style–based education materials, and tailored text messages ( 24 , 25 , 27 ). Wolf et al. ( 27 ) investigated the use of PCL in patients with type 2 diabetes and found that patients with low health literacy who take medication two or more times per day have higher rates of proper medication use when using PCL (85.9 vs. 77.4%, P = 0.03). The objective of the PCL intervention was to make medication instructions and other information on the labels easier to read to improve medication use and adherence rates. The labels incorporated best-practice strategies introduced by the Institute of Medicine for the Universal Medication Schedule. These strategies prioritize medication information, use of larger font sizes, and increased white space. Of note, the benefits of PCL were largely seen with English speakers. Spanish speakers did not have substantial improvement in medication use or adherence, which could be attributed to language barriers ( 27 ).
Nelson et al. ( 25 ) analyzed patients’ engagement with an automated text message approach to supporting diabetes self-care activities in a 12-month randomized controlled trial (RCT) called REACH (Rapid Education/Encouragement and Communications for Health) ( 25 ). Messages were tailored based on patients’ medication adherence, the Information-Motivation-Behavioral Skills model of health behavior change, and self-care behaviors such as diet, exercise, and self-monitoring of blood glucose. Patients in this trial were native English speakers, so further research to evaluate the impact of the text message intervention in patients with limited English language skills is still needed. However, participants in the intervention group reported higher engagement with the text messages over the 12-month period ( 25 ).
Patients who receive educational materials based on their learning style also show significant improvement in their diabetes knowledge and health literacy. Koonce et al. ( 24 ) developed and evaluated educational materials based on patients’ learning style to improve health literacy in both English and Spanish languages. The materials were made available in multiple formats to target four different learning styles, including materials for visual learners, read/write learners, auditory learners, and kinesthetic learners. Spanish-language versions were also available. Researchers were primarily interested in measuring patients’ health literacy and knowledge of diabetes. The intervention group received materials in their preferred learning style and language, whereas the control group received standard of care education materials. The intervention group showed significant improvement in diabetes knowledge and health literacy, as indicated by Diabetes Knowledge Test (DKT) scores. More participants in the intervention group reported looking up information about their condition during week 2 of the intervention and showed an overall improvement in understanding symptoms of nerve damage and types of food used to treat hypoglycemic events. However, the study had limited enrollment of Spanish speakers, making the applicability of the results to Spanish-speaking patients highly variable.
Additionally, findings by Hofer et al. ( 22 ) suggest that patients with high A1C levels may benefit from interventions led by community health workers (CHWs) to bridge gaps in health literacy and equip patients with the tools to make health decisions. In this study, Hispanic and African American patients with low health literacy and diabetes not controlled by oral therapy benefited from education sessions led by CHWs. The CHWs led culturally tailored support groups to compare the effects of educational materials provided in an electronic format (via iDecide) and printed format on medication adherence and self-efficacy. The study found increased adherence with both formats, and women, specifically, had a significant increase in medication adherence and self-efficacy. One of the important aspects of this study was that the CHWs shared cultural and linguistic characteristics with the patients and HCPs, leading to increased trust and satisfaction with the information presented ( 22 ).
Kim et al. ( 23 ) found that Korean-American participants benefited greatly from group education sessions that provided integrated counseling led by a team of nurses and CHW educators. The intervention also had a health literacy component that focused on enhancing skills such as reading food package labels, understanding medical terminology, and accessing health care services. This intervention led to a significant reduction of 1–1.3% in A1C levels in the intervention group. The intervention established the value of collaboration between CHW educators and nurses to improve health information delivery and disease management.
A collaboration between CHW educators and pharmacists was also shown to reinforce diabetes knowledge and improve health literacy. Sharp et al. ( 26 ) conducted a cross-over study in four primary care ambulatory clinics that provided care for low-income patients. The study found that patients with low health literacy had more visits with pharmacists and CHWs than those with high health literacy. The CHWs provided individualized support to reinforce diabetes self-management education and referrals to resources such as food, shelter, and translation services. The translation services in this study were especially important for building trust with non-English speakers and helping patients understand their therapy. Similar to other studies, the CHWs shared cultural and linguistic characteristics with their populations, which helped to overcome communication-related and cultural barriers ( 23 , 26 ).
The use of electronic tools or educational videos yielded inconclusive results with regard to medication adherence. Graumlich et al. ( 20 ) implemented a new medication planning tool called Medtable within an electronic medical record system in several outpatient clinics serving patients with type 2 diabetes. The tool was designed to organize medication review and patient education. Providers can use this tool to search for medication instructions and actionable language that are appropriate for each patient’s health literacy level. The authors found no changes in medication knowledge or adherence, but the intervention group reported higher satisfaction. On the other hand, Yeung et al. ( 28 ) showed that pharmacist-led online education videos accessed using QR codes affixed to the patients’ medication bottles and health literacy flashcards increased patients’ medication adherence in an academic medical hospital.
Goessl et al. ( 21 ) found that patients with low health literacy had significantly higher retention of information when receiving evidence-based diabetes education through a DVD recording than through an in-person group class. This 18-month RCT randomized participants to either the DVD or in-person group education and assessed their information retention through a teach-back strategy. The curriculum consisted of diabetes prevention topics such as physical exercise, food portions, and food choices. Participants in the DVD group had significantly higher retention of information than those in the control (in-person) group. The authors suggested this may have been because participants in the DVD group have multiple opportunities to review the education material.
Management of type 2 diabetes remains a challenge for HCPs and patients, in part because of the challenges discussed in this review, including communication barriers between patients and HCPs and knowledge deficits about medications and disease states ( 29 ). HCPs can have a positive impact on the health outcomes of their patients with diabetes by improving patients’ disease state and medication knowledge.
One of the common themes identified in this literature review was the prevalence of culturally tailored diabetes education interventions. This is an important strategy that could improve diabetes outcomes and provide an alternative approach to diabetes self-management education when working with patients from culturally diverse backgrounds. HCPs might benefit from using culturally tailored educational approaches to improve communication with patients and overcome the medical mistrust many patients feel. Although such mistrust was not directly correlated with diabetes management, it was noted that patients who feel mistrustful tend to have poor communication with HCPs ( 20 ). Additionally, Latino/Hispanic patients who have language barriers tend to have poor glycemic control ( 19 ). Having CHWs work with HCPs might mitigate some patient-provider communication barriers. As noted earlier, CHWs who share cultural and linguistic characteristics with their patient populations have ongoing interactions and more frequent one-on-one encounters ( 12 ).
Medication adherence and glycemic control are important components of diabetes self-management, and we noted that the integration of CHWs into the diabetes health care team and the use of simplified medication label interventions were both successful in improving medication adherence ( 23 , 24 ). The use of culturally tailored education sessions and the integration of pharmacists and CHWs into the management of diabetes appear to be successful in reducing A1C levels ( 12 , 26 ). Electronic education tools and educational videos alone did not have an impact on medication knowledge or information retention in patients with low health literacy, but a combination of education tools and individualized sessions has the potential to improve diabetes medication knowledge and overall self-management ( 20 , 22 , 30 ).
There were several limitations to our literature review. We restricted our search criteria to articles published in English and studies conducted within the United States to ensure that the results would be relevant to U.S. HCPs. However, these limitations may have excluded important work on this topic. Additional research expanding this search beyond the United States and including articles published in other languages may demonstrate different outcomes. Additionally, this literature review did not focus on A1C as the primary outcome, although A1C is an important indicator of diabetes self-management. A1C was chosen as the method of evaluating the impact of health literacy interventions in patients with diabetes, but other considerations such as medication adherence, impact on comorbid conditions, and quality of life are also important factors.
The results of this work show that implementing health literacy interventions to help patients manage type 2 diabetes can have beneficial results. However, such interventions can have significant time and monetary costs. The potential financial and time costs of diabetes education interventions were not evaluated in this review and should be taken into account when designing interventions. The American Diabetes Association estimated the cost of medical care for people with diabetes to be $327 billion in 2017, with the majority of the expenditure related to hospitalizations and nursing home facilities ( 16 ). Another substantial cost of diabetes that can be difficult to measure is treatment for comorbid conditions and complications such as cardiovascular and renal diseases.
Interventions designed to address low health literacy and provide education about type 2 diabetes could be a valuable asset in preventing complications and reducing medical expenditures. Results of this work show that clinicians who are considering implementing new interventions may benefit from the following strategies: using culturally tailored approaches, creating materials for different learning styles and in patients’ languages, engaging CHWs and pharmacists to help with patient education, using PCLs for medications, and engaging education session instructors who share patients’ cultural and linguistic characteristics.
Diabetes self-management is crucial to improving health outcomes and reducing medical costs. This literature review identified interventions that had a positive impact on provider-patient communication, medication adherence, and glycemic control by promoting diabetes self-management through educational efforts to address low health literacy. Clinicians seeking to implement diabetes care and education interventions for patients with low health literacy may want to consider drawing on the strategies described in this article. Providing culturally sensitive education that is tailored to patients’ individual learning styles, spoken language, and individual needs can improve patient outcomes and build patients’ trust.
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
Author Contributions
Both authors conceptualized the literature review, developed the methodology, analyzed the data, and wrote, reviewed, and edited the manuscript. R.A. collected the data. K.M. supervised the review. K.M. is the guarantor of this work and, as such, has full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation
Portions of this research were presented at the Washington State University College of Pharmacy and Pharmaceutical Sciences Honors Research Day in April 2019.
Email alerts
- Online ISSN 1944-7353
- Print ISSN 1040-9165
- Diabetes Care
- Clinical Diabetes
- Diabetes Spectrum
- Standards of Medical Care in Diabetes
- Scientific Sessions Abstracts
- BMJ Open Diabetes Research & Care
- ShopDiabetes.org
- ADA Professional Books
Clinical Compendia
- Clinical Compendia Home
- Latest News
- DiabetesPro SmartBrief
- Special Collections
- DiabetesPro®
- Diabetes Food Hub™
- Insulin Affordability
- Know Diabetes By Heart™
- About the ADA
- Journal Policies
- For Reviewers
- Advertising in ADA Journals
- Reprints and Permission for Reuse
- Copyright Notice/Public Access Policy
- ADA Professional Membership
- ADA Member Directory
- Diabetes.org
- X (Twitter)
- Cookie Policy
- Accessibility
- Terms & Conditions
- Get Adobe Acrobat Reader
- © Copyright American Diabetes Association
This Feature Is Available To Subscribers Only
Sign In or Create an Account
Introduction to diabetes mellitus
Affiliation.
- 1 Institute of Biomedical and Clinical Science, Peninsula College of Medicine and Dentistry, University of Exeter, Exeter, UK.
- PMID: 23393665
- DOI: 10.1007/978-1-4614-5441-0_1
The chronic metabolic disorder diabetes mellitus is a fast-growing global problem with huge social, health, and economic consequences. It is estimated that in 2010 there were globally 285 million people (approximately 6.4% of the adult population) suffering from this disease. This number is estimated to increase to 430 million in the absence of better control or cure. An ageing population and obesity are two main reasons for the increase. Furthermore it has been shown that almost 50% of the putative diabetics are not diagnosed until 10 years after onset of the disease, hence the real prevalence of global diabetes must be astronomically high. This chapter introduces the types of diabetes and diabetic complications such as impairment of immune system, periodontal disease, retinopathy, nephropathy, somatic and autonomic neuropathy, cardiovascular diseases and diabetic foot. Also included are the current management and treatments, and emerging therapies.
Publication types
- Chronic Disease
- Diabetes Complications / drug therapy
- Diabetes Complications / physiopathology
- Diabetes Mellitus, Type 1 / drug therapy*
- Diabetes Mellitus, Type 1 / physiopathology*
- Diabetes Mellitus, Type 2 / drug therapy*
- Diabetes Mellitus, Type 2 / physiopathology*
- Hypoglycemic Agents / therapeutic use*
- Hypoglycemic Agents
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Indian J Ophthalmol
- v.69(11); 2021 Nov
Epidemiology of type 2 diabetes in India
Rajendra pradeepa.
Madras Diabetes Research Foundation and Dr. Mohan's Diabetes Specialities Centre, IDF Centre of Excellence in Diabetes Care and ICMR Centre for Advanced Research on Diabetes, Chennai, Tamil Nadu, India
Viswanathan Mohan
The burden of diabetes is high and increasing globally, and in developing economies like India, mainly fueled by the increasing prevalence of overweight/obesity and unhealthy lifestyles. The estimates in 2019 showed that 77 million individuals had diabetes in India, which is expected to rise to over 134 million by 2045. Approximately 57% of these individuals remain undiagnosed. Type 2 diabetes, which accounts for majority of the cases, can lead to multiorgan complications, broadly divided into microvascular and macrovascular complications. These complications are a significant cause for increased premature morbidity and mortality among individuals with diabetes, leading to reduced life expectancy and financial and other costs of diabetes leading to profound economic burden on the Indian health care system. The risk for diabetes is largely influence by ethnicity, age, obesity and physical inactivity, unhealthy diet, and behavioral habits in addition to genetics and family history. Good control of blood sugar blood pressure and blood lipid levels can prevent and/or delay the onset of diabetes complications. The prevention and management of diabetes and associated complications is a huge challenge in India due to several issues and barriers, including lack of multisectoral approach, surveillance data, awareness regarding diabetes, its risk factors and complications, access to health care settings, access to affordable medicines, etc. Thus, effective health promotion and primary prevention, at both, individual and population levels are the need of the hour to curb the diabetes epidemic and reduce diabetes-related complications in India.
Diabetes is one of the largest global health emergencies of this century, ranking among the 10 leading causes of mortality together with cardiovascular disease (CVD), respiratory disease, and cancer.[ 1 , 2 ] According to the World Health Organization (WHO), noncommunicable diseases (NCDs) accounted for 74% of deaths globally in 2019, of which, diabetes resulted in 1.6 million deaths, thus becoming the ninth leading cause of death globally.[ 2 ] By the year 2035, nearly 592 million people are predicted to die of diabetes.[ 3 ] Type 2 diabetes, which constitutes 90% of all cases of diabetes, earlier considered to be a disease of the affluent “Western” countries, has now spread globally, and has become a major cause of disability and death affecting even younger age group.[ 1 ] Diabetes has reached epidemic proportions in many developing economies, such as China and India.[ 1 ] According to WHO, the prevalence of diabetes is growing most rapidly in low- and middle-income countries.[ 4 ] The rapid socioeconomic change in conjunction with urbanization and industrialization are the major factors for the global increase in the diabetes epidemic, with other associated risk factors such as population growth, unhealthy eating habits, and a sedentary lifestyle also playing an important role.[ 5 ]
Diabetes is a progressive disorder that leads to serious complications, which are associated with increased costs to the family, community, and healthcare system. Uncontrolled diabetes leads to increased risk of vascular disease and much of the burden of type 2 diabetes is caused by macrovascular (cardiovascular (CV), cerebrovascular, and peripheral artery disease) and microvascular (diabetic retinopathy, nephropathy, and neuropathy) complications.[ 5 , 6 ]
Global Burden of Diabetes
Type 2 diabetes susceptibility varies to a great extent around the globe, with Pacific Islanders, Asian Indians, and Native Americans having a significantly higher risk of developing the disorder. The number of people with type 2 diabetes began to rise globally in the 1990s, and since 2000, the world has seen a dramatic increase in the number of people with diabetes.[ 7 ] According to the International Diabetes Federation (IDF), 8.8% of the adult population have diabetes, with men having slightly higher rates (9.6%) than women (9.0%).[ 1 ] Current global statistics shows that 463 million and 374 million individuals have diabetes and impaired glucose tolerance (IGT), a prediabetic condition. These numbers are estimated to increase to 700 million people with diabetes and 548 million people with IGT by 2045, which represents a 51% increase compared to 2019.[ 1 ]
Among the IDF regions, the Western Pacific has the highest number of people with diabetes (163 million), followed by the South-East Asian region (88 million), Europe (59 million), Middle East and North Africa (55 million), and North America and Caribbean (47.6 million). Currently, the lowest numbers are found in South and Central America (36.1 million) and Africa (19.4 million).[ 1 ] Thus, it is apparent that the affluent regions of Europe and North America are not the only ones dealing with the diabetes epidemic.
According to the IDF in 2019, the top three countries with the highest number of individuals with diabetes are China (116.4 million), India (77.0 million), and the United States of America (31.0 million). This trend is expected to continue in 2030 and 2045, with China (140.5 and 147.2 million) and India (101.0 and 134.2 million) continuing to have the highest burden of diabetes.[ 1 ] This is supported by the Global Burden of Disease Study, which reported that population growth and ageing in the world's largest countries, such as China and India, are driving the absolute increase in the number of people with diabetes.[ 8 ]
According to prevalence estimates by IDF, the diabetes burden is growing faster in low- and middle-income countries (367.8 million) than in high-income countries (95.2 million).[ 1 ] The Global Burden of Disease study conducted in 195 countries and territories provided a detailed overview of the numbers, rates, and rising trends in the diabetes burden between 1990 and 2025.[ 9 ] This study also reported that the low- and middle-income regions had higher burden of diabetes, while the high-income regions had lower burden of diabetes. This study reported that the number of people with incident diabetes increased from 11.3 to 22.9 million between 1990 and 2017 (an increase by 102.9%) and the number of prevalent diabetes increased from 211.2 to 476.0 million (an increase by 129.7%), respectively. Furthermore, modifiable metabolic, environmental, and behavioral factors were found to be the major risk factors for diabetes burden.
Another cause for concern is the high percentage of individuals with undiagnosed diabetes, which is currently more than 50%. This is observed mainly in developing economies due to less developed health care systems. It is estimated that approximately 231.9 million (one in two) of adults with diabetes are undiagnosed worldwide.[ 1 ] Fig. 1 depicts the proportion and number of individuals with undiagnosed diabetes in various IDF regions.[ 1 ] According to reports, nearly 59.7% of people with diabetes in Africa are unaware of their disease (the highest such proportion among all regions), while only 37.8% of people with diabetes in North America and the Caribbean are unaware of their disease (the lowest proportion among all the regions). When compared to other IDF regions, Africa and South and Central America have a lower number of individuals with undiagnosed diabetes (11.6 and 13.3 million, respectively).[ 1 ] According to these estimates, there is an urgent need for improved diabetes screening. They also highlight the importance of identifying undiagnosed diabetes and providing appropriate and timely care as undiagnosed diabetes can have negative consequences such as an increased risk of diabetes related complications, increased healthcare use, and associated costs.[ 10 ]

Proportion and number of individuals with undiagnosed diabetes – International Diabetes Federation (IDF) [ Ref No: 1 ]
Burden of Diabetes in India
Diabetes has steadily increased in India and around the world over the last three decades, with India accounting for a sizable portion of the global burden. India's disease patterns have shown a switch due to an epidemiological transition: thus mortality from communicable, maternal, neonatal, and nutritional diseases (CMNNDs) has decreased significantly, while NCDs and injuries have markedly increased their contribution to overall disease burden and mortality.[ 11 ] In India in 1990, the total disability adjusted life years (DALYs) from CMNNDs were 61%, 30% from NCDs, and 9% from injuries. However, due to major epidemiological transitions in India over the years, total DALYs from CMNNDs have decreased to 33%, while those from NCDs and injuries have increased to 55 and 12%, respectively, in 2016 [ Fig. 2 ]. Across India, the disease burden or DALY rate in 2016 was 4-fold for diabetes, and when looked at the leading individual causes of DALYs in India, most NCDs have risen in rank since 1990, with diabetes showing a dramatic increase, from 35 th place in 1990 to 13 th place in 2016.[ 11 ]

Causes of total deaths in India, 1990 and 2016 (Communicable vs noncommunicable vs injuries) [Ref No: 11 ]
Prevalence of diabetes and trends over time
In India, the burden of diabetes has been increasing steadily since 1990 and leaps and at a faster pace from the year 2000. Fig. 3 shows the increasing trend in diabetes prevalence in India during the past decade in India as per IDF.[ 1 , 12 , 13 , 14 , 15 , 16 ] The prevalence of diabetes in India has risen from 7.1% in 2009 to 8.9% in 2019. Table 1 provides the burden of diabetes in India at a glance. Currently, 25.2 million adults are estimated to have IGT, which is estimated to increase to 35.7 million in the year 2045. India ranks second after China in the global diabetes epidemic with 77 million people with diabetes. Of these, 12.1 million are aged >65 years, which is estimated to increase to 27.5 million in the year 2045. It is also estimated that nearly 57% of adults with diabetes are undiagnosed in India, which is approximately 43.9 million. The mean healthcare expenditure on diabetes per person is 92 US dollars, and total deaths attributable directly to diabetes account for 1 million.

Trends in diabetes prevalence during the past decade in India [Source: Ref 1 , 12 , 13 , 14 , 15 , 16 ]
Burden of diabetes/prediabetes in India (Ref No. 1 )
*USD - US dollars; Source IDF Diabetes Atlas 2019 (Ref No: 1)
The report on the state-level disease burden in India stated that the percent change in diabetes prevalence among all ages in India from 1990 to 2016 was 64.3%, while the age-standardized prevalence was 29.3%.[ 11 ] The India State-Level Disease Burden Initiative Diabetes study collaborators[ 17 ] reported that the prevalence and number of people with diabetes in India increased from 5.5% and 26.0 million in 1990 to 7.7% and 65.0 million in the year 2016. According to this report, Tamil Nadu had the highest prevalence in 2016, followed by Kerala, Delhi, Punjab, Goa, and Karnataka.
Diabetes is becoming more prevalent in India, based on the data obtained from cross-sectional surveys conducted in various parts of the country.[ 18 ] The first study was conducted in Mumbai in 1963 among 18,243 individuals, and the prevalence of diabetes was found to be 1.5% based on urine analysis.[ 19 ] There have been a few national studies on the prevalence of diabetes. The national prevalence of diabetes was reported to be 2.1% in the multicenter ICMR survey conducted between 1972 and 1975 in Ahmedabad, Calcutta, Cuttack, Delhi, Poona, and Trivandrum, as well as neighboring rural areas.[ 20 ] In 2001, the National Urban Diabetes Survey conducted in India's six major cities reported an age-standardized prevalence of 12.1%,[ 21 ] while the Prevalence of Diabetes in India Study, conducted in 40 urban and 37 small towns and rural areas across India in 2004, found that the prevalence of diabetes to be 5.9 and 2.7%, respectively.[ 22 ] The WHO-ICMR NCD Risk Factor Surveillance Study, conducted between 2003 and 2005 in urban and rural areas of six different states, reported a 4.5% prevalence of self-reported diabetes.[ 23 ]
In the Indian Council of Medical Research–India DIABetes study, the largest nationally representative epidemiological survey conducted in India on diabetes and prediabetes, the data from 15 states/UT of the country [ Table 2 ] showed that the prevalence of diabetes ranged from 3.5 to 8.7% in rural to 5.8 to 15.5% in urban areas and the prevalence varied from 4.3% in Bihar to 13.6% in Chandigarh.[ 24 , 25 ] The prevalence of diabetes was higher in urban areas (11.2%) compared to rural areas (5.2%). The prevalence of prediabetes ranged from 5.8 to 14.7% in rural to 7.2 to 16.2% in urban areas. The prevalence of prediabetes exceeded that of diabetes in most states. This indicates the presence of a large number of individuals who may develop type 2 diabetes in the near future. There is also evidence that Asian Indians progress more rapidly through the prediabetes stage as compared to people of other ethnic groups.[ 25 , 26 ] The prevalence of diabetes was higher among states with higher per capita GDP and among individuals belonging to the higher SES. This study demonstrates that there is clear evidence of an epidemiological transition, with a higher prevalence of diabetes in low socioeconomic status of urban areas in more economically developed states.[ 25 ]
Weighted prevalence of diabetes and prediabetes in 15 states/Union territory of India - the ICMR INDIAB Study [Ref Nos: 24 , 25 ]
The National Family Health Survey, four survey[ 27 ] conducted in 15 Indian states/union territories during the year 2014–2015, reported that Andaman and Nicobar Islands had the highest prevalence of diabetes (26 and 14.5% among men and women, respectively), while Haryana had the lowest prevalence of diabetes (8.2%) for men and Bihar (6.1%) for women. The prevalence was higher in urban than in rural areas. The recent Secular Trends in Diabetes in India study which assessed the change in diabetes prevalence between 2006 and 2016 in urban and rural areas of Tamil Nadu reported that the prevalence of diabetes increased from 18.6% in 2006 to 21.9 in 2016 in the city, while in the smaller towns, it increased from 16.4 to 20.3, and in the periurban villages, from 9.2 to 13.4, respectively.[ 28 ]
Data from the population-based representative Center for Cardio-metabolic Risk Reduction in South Asia (CARRS) Study reports that 6 out of 10 adults in South Asian cities have either diabetes or prediabetes.[ 29 ] In Chennai, 22.8%, and in Delhi, 25.2% of the population was estimated to have diabetes. This study also reported a diabetes prevalence of 16.3% in Karachi, Pakistan, which is lower than the two cities in India. In the CARRS cohort, the lifetime diabetes risk for 20-year-old men was 55.5% compared to 64.6% for women and was high among obese women (86.0%) and men (86.9%). With increasing age (at age 60 years), the lifetime risk of diabetes decreased to 37.7% for women and 27.5% for men.[ 30 ] Recent studies contradict previous findings that migrant Indians had higher prevalence rates of type 2 diabetes than their counterparts in India. The prevalence of type 2 diabetes was reported to be higher in Asian Indians living in Chennai (38%) compared to those residing in San Francisco and Chicago, US (24%).[ 31 ] These findings highlight the fact that India's current rapid economic and nutritional transitions increase the risk of type 2 diabetes, and that the “diabetogenic” environment in India is now as bad, if not worse, as in the United States.
Incidence of diabetes
Apart to from the rising prevalence of diabetes in India, the incidence of diabetes are also rising steadily, with a fast transition from euglycemia to prediabetes and diabetes. In India, very few longitudinal studies have been conducted to assess the incidence of diabetes and prediabetes. In the Chennai Urban Population Study cohort, diabetes and prediabetes incidence rates were reported to be 20.2 and 13.1 per 1000 person-years, respectively,[ 32 ] while the follow-up study conducted in the Chennai Urban Rural Epidemiology Study (CURES) cohort reported the incidence rates of diabetes, prediabetes, and any dysglycemia to be 22.2, 29.5, and 51.7 per 1000 person-years, respectively.[ 33 ] The conversion rate to diabetes was reported to be 19.4% among those with normal glucose tolerance and 58.9% among those with prediabetes. Diabetes incidence was reported to be 78.9 per 1000 person-years among those with prediabetes.[ 33 ]
In Kerala, participants of the Study of Life Style Diseases in Central Kerala were followed up over a 10-year period from two semiurban wards of Venmony Panchayat of Alappuzha district. The incidence rate of type 2 diabetes and impaired fasting glucose (IFG) were 24.5 per 1000 person-years and 45.01 per 1000 person-years, respectively. During the follow-up period, nearly 60% of participants with baseline IFG converted to type 2 diabetes.[ 34 ]
In another follow-up study conducted in rural areas of Puducherry, the incidence rate of diabetes was reported to be 21.5 per 1,000 person-years. The incidence rate doubled among males (28.7 per 1000 person-years) compared with females (14.6 per 1000 person-years).[ 35 ]
Morbidity and mortality
Diabetes is well known for its systemic impact on a wide range of diabetes-related complications, including macrovascular and microvascular complications and death among the most feared outcomes. In addition, recently diabetes is also being linked to nontraditional complications such as mental health, cancer, disability, and liver disease.[ 36 ] Diabetic retinopathy is recognized as the most specific complication of diabetes and has been used to guide diabetes diagnostic thresholds. The prevalence of diabetic retinopathy has been estimated to be 17.6% among adults with diabetes in urban South India.[ 37 ] Spectrum of eye disorders in diabetes in India report, pan-India facility-based study, concluded that diabetic retinopathy was prevalent in one-third and sight-threatening diabetic retinopathy in one-fifth of people with type 2 diabetes presenting at 14 eye-care facilities.[ 38 ] The CURES study conducted in urban Southern India reported lower prevalences of retinopathy, nephropathy, neuropathy, and peripheral vascular disease and higher prevalence of coronary artery disease (CAD) compared to those reported for Western populations.[ 37 , 39 , 40 , 41 , 42 ] Data from rural areas indicate that the burden of complications is comparable, if not higher, in rural areas of South India than in urban areas.[ 43 ] The relatively high prevalence of diabetic complications in developing economies like India could be due to delay in diagnosis of diabetes as well as complications, coexisting illness, inadequate health care systems, and high drug cost, particularly insulin leading to poor control of diabetes.
Diabetes, along with its complications, is a leading cause of mortality. The South East Asian region has the second highest number of deaths attributable to diabetes in adults among the IDF Regions, with 1.2 million deaths in 2019, with India contributing the lion's share with more than 1 million estimated deaths accountable to diabetes and related complications.[ 1 ] The Prospective Urban Rural Epidemiology study which compared CV events, all-cause mortality, and CV mortality rates among 143,567 adults with and without diabetes in 21 countries including India with different income levels reported that CVD rates, all-cause mortality, and CV mortality were markedly higher among those with diabetes in low-income countries compared with middle- and high-income countries.[ 44 ] The India State-Level Disease Burden Initiative Diabetes study reported that diabetes contributed to 3.1% of all deaths in India, with an increase in death rates due to diabetes from 1990 to 2016 by 131%.[ 17 ]
There are as yet no large-scale Indian studies on mortality in patients with type 2 diabetes, and most available studies are from clinical settings and therefore have shown different results. In a retrospective study from Srinagar[ 45 ] of 234,776 inpatient admissions, 16,690 died, of whom 4.4% had diabetes. Of the top five causes of death, infections were reported by 41%, chronic renal failure by 33.6%, CAD by 16.9%, cerebrovascular disease by 13.2%, and chronic obstructive pulmonary disease by 6.9%. A follow-up of the CURES cohort reported overall mortality rate to be nearly 4-fold higher in people with diabetes compared to those without diabetes (27.9 per 1000 person-years vs. 8.0 per 1000 person-years). The study also illustrated that ischemic heart disease and diabetes had the highest population-attributable risk for all-cause mortality in the entire study cohort.[ 46 ]
Risk Factors
The etiology of diabetes is believed to be multifactorial. Many individual-level nonmodifiable risk factors like genetic, age, ethnicity, and family history have been prospectively associated with type 2 diabetes, but the increases in prevalence in most populations have probably been driven by a modifiable risk factors including sedentary lifestyle and/or lack of exercise, increasing prevalence of overweight/obesity, unhealthy diets (increased intake of refined grains, fat, sugar, and sweetened beverages and decreased intake of fruits and vegetables) and habits (smoking and alcohol abuse), exposure to environmental pollutants, altered intrauterine environment and mental health (stress/depression), short sleep duration, and the built environment [ Fig. 4 ].

Risk factors for type 2 diabetes
According to the India state-level disease burden report,[ 47 ] in 1990, a tenth of the total disease burden in India was caused by a cluster of risk factors that included unhealthy diet, being overweight/obese, high blood pressure, blood sugar, and cholesterol, all of which contributed to ischemic heart disease, stroke, and diabetes, which increased to a quarter of the total disease burden in India in 2016. Tobacco use, which was accountable for 6% of the total disease burden in India in 2016, is another significant contributor to CVD and diabetes, as well as cancer and some other diseases.[ 47 ] The Global Burden of Disease Study 2016, reported obesity, low-dietary intake of fruits, nuts and seeds, and whole grains, and tobacco use to be the most important risk factors for DALYs and deaths due to diabetes.[ 48 ]
Strategies to Tackle the Epidemic of Diabetes in India
The rising rates of prediabetes, diabetes, and associated complications in urban as well as in rural areas and among the young in India are of great concern. Addressing health issues related to diabetes in India, which is the second-most populous country and has a large and diverse population, poses many challenges. The specific challenges in diabetes prevention/management are (i) lack of strong national partnerships for multisectoral actions, (ii) lack of availability of robust surveillance and research data on diabetes, (iii) abysmally low disease awareness among the public, (iv) lack of access to basic prevention/management of diabetes in the primary health care setting, which includes access to affordable medicines leading to premature deaths, (v) disproportionate fund allocation for diabetes programs, (vi) difficulties in engaging the industry and private sector, (vii) limited human resources, and (viii) inadequate community mobilization and weak coordination among civil societies and between the civil societies and government agencies for diabetes.
Tackling diabetes calls for a fundamental change, from addressing each risk factor separately to collectively addressing a cluster of risk factors in an integrated manner, and from using a biomedical approach to a public health approach. Thus, when planning prevention/control programs, a multifaceted approach is essential for success. Diabetes prevention/control strategies include (i) reduction in exposure to lifestyle risk factors through health promotion and primary prevention, (ii) early detection and timely treatment, and (iii) surveillance to monitor trends in diabetes and associated risk factors. High levels of commitment and multisectoral actions are needed to reduce the growing burden of diabetes in India. Some of the policies that may help to slow down the epidemic of diabetes in India include (i) national food policies targeting availability and accessibility of healthy and nutritious foods, ensuring that the food industry strictly complies with norms of food safety and standards and supporting production and distribution of healthy foods (whole grains, fruit, vegetables, legumes, and nuts), (ii) health policies to reduce harmful behaviors such as smoking, alcohol misuse, use of trans fat, and consumption of junk foods and increase physical activity by the creation of amenities such as public spaces (e.g., parks) for walking, cycling, etc., (iii) prevention policies such as health information and communication to improve population awareness, and (iv) policies to reduce the cost of essential drugs and ensuring reasonable access to care. All these efforts need a healthy collaboration between health, information, education, and agriculture ministries to create awareness and to facilitate a healthy lifestyle among the Indian population.
Diabetes has already become a leading threat to public health globally and the picture becomes grimmer for the low- and middle-income countries like India, where the burden has risen significantly in recent decades and will continue to rise in the coming decades. This could have a great influence on morbidity and mortality associated with diabetes and, thus, on the overall healthcare expenditure in India. To curb the epidemic of diabetes and its associated complications, there is a need for a multipronged strategy involving early diagnosis of diabetes, screening for its complications, and offering optimal therapy at all levels of care for those who already have diabetes and primary prevention of diabetes in those with prediabetes.
Financial support and sponsorship
Conflicts of interest.
There are no conflicts of interest.

IMAGES
VIDEO
COMMENTS
Type 2 Diabetes Mellitus (T2DM) is characterized by chronically elevated blood glucose (hyperglycemia) and elevated blood insulin (hyperinsulinemia). When the blood glucose concentration is 100 milligrams/deciliter the bloodstream of an average adult contains about 5-10 grams of glucose. Carbohydrate-restricted diets have been used effectively to treat obesity and T2DM for over 100 years ...
I. Introduction. Diabetes mellitus, a metabolic disease defined by elevated fasting blood glucose levels due to insufficient insulin production, has reached epidemic proportions worldwide (World Health Organization, 2020).Type 1 and type 2 diabetes (T1D and T2D, respectively) make up the majority of diabetes cases with T1D characterized by autoimmune destruction of the insulin-producing ...
The diagnosis of incident diabetes was based on an oral glucose tolerance test (OGTT). The overall risk reduction of T2D by the lifestyle interventions was 0.53 (95% CI 0.41; 0.67). Most of the trials aimed to reduce weight, increase physical activity, and apply a diet relatively low in saturated fat and high in fiber.
1. Introduction. Diabetes Mellitus (DM) commonly referred to as diabetes, is a chronic disease that affects how the body turns food into energy .It is one of the top 10 causes of death worldwide causing 4 million deaths in 2017 , .According to a report by the International Diabetes Federation (IDF) , the total number of adults (20-79 years) with diabetes in 2045 will be 629 million from 425 ...
Type 2 diabetes accounts for nearly 90% of the approximately 537 million cases of diabetes worldwide. The number affected is increasing rapidly with alarming trends in children and young adults (up to age 40 years). Early detection and proactive management are crucial for prevention and mitigation of microvascular and macrovascular complications and mortality burden. Access to novel therapies ...
New estimates published this week in The Lancet indicate that more than 1·31 billion people could be living with diabetes by 2050 worldwide. That's 1·31 billion people living with a disease that causes life-altering morbidity, high rates of mortality, and interacts with and exacerbates many other diseases. The increase in prevalence (up from 529 million in 2021) is expected to be driven by ...
Type 2 diabetes mellitus (T2DM) is an expanding global health problem, closely linked to the epidemic of obesity. Individuals with T2DM are at high risk for both microvascular complications ...
Type 2 diabetes mellitus, the most frequent subtype of diabetes, is a disease characterized by high levels of blood glucose (hyperglycaemia). ... Research Open Access 27 Apr 2024 npj Digital Medicine.
In this review, we summarize the advanced research on risk factors of type 2 diabetes. Prevalence of diabetes and economic burden. In recent decades, China has undergone rapid economic development, urbanization, and transitions in lifestyles . These have contributed to an explosive increase in type 2 diabetes prevalence within a relatively ...
Abstract. Diabetes mellitus is a chronic multifaceted disease with multiple potential complications, the treatment of which can only delay and prolong the terminal stage of the disease, i.e., type 2 diabetes mellitus (T2DM). The World Health Organization predicts that diabetes will be the seventh leading cause of death by 2030.
Diabetes is the seventh leading cause of death in the United States, and 30.3 million Americans, or 9.4% of the U.S. population, are living with diabetes (1,2).For successful management of a complicated condition such as diabetes, health literacy may play an important role.
Overview. Type 2 diabetes mellitus is a costly disease, affecting individuals, health care systems, economies, and whole societies worldwide. Diabetes and its precursor, prediabetes, affect 8% and 7% of the world's population, respectively. 1,2 Type 2 diabetes mellitus (hereafter called diabetes) makes up 95% of all diabetes cases. 2 Overwhelming evidence shows that lifestyle intervention ...
Diabetes mellitus (DM) underscores a rising epidemic orchestrating critical socio-economic burden on countries globally. Different treatment options for the management of DM are evolving rapidly because the usual methods of treatment have not completely tackled the primary causes of the disease and are laden with critical adverse effects. Thus, this narrative review explores different ...
The chronic metabolic disorder diabetes mellitus is a fast-growing global problem with huge social, health, and economic consequences. It is estimated that in 2010 there were globally 285 million people (approximately 6.4% of the adult population) suffering from this disease. This number is estimated to increase to 430 million in the absence of ...
Prevention of Cardiovascular Disease in Type 1 Diabetes. C. Manrique-Acevedo, I.B. Hirsch, and R.H. EckelN Engl J Med 2024;390:1207-1217. More than half of newly diagnosed cases of type 1 diabetes ...
Introduction. Physical activity is at the cornerstone of the lifestyle management of type 2 diabetes (T2D). 1 Regular physical activity is associated with substantially lower cardiovascular and overall mortality risk. 2, 3 Getting started and sustaining a physically active lifestyle is challenging, particularly for those with established T2D. 4 Data from England show that in the general ...
Different classes of diabetes mellitus, type 1, type 2, gestational diabetes and other types of diabetes mellitus are compared in terms of diagnostic criteria, etiology and genetics. The molecular genetics of diabetes received extensive attention in recent years by many prominent investigators and research groups in the biomedical field.
Type 2 diabetes mellitus (T2D) and hypertension, the 2 leading components of the global burden of disease, are commonly found to coexist. 1-3 The coexistence of T2D and hypertension confers a dramatically increased risk (2- to 4-fold) of cardiovascular disease, end-stage kidney disease, and death, compared with the normotensive and nondiabetic adults. 3 Hence, understanding the bidirectional ...
Type 2 diabetes accounts for nearly 90% of the approximately 537 million cases of diabetes worldwide. The number afected is increasing rapidly with alarming trends in children and young adults (up to age 40 years). Early detection and proactive management are crucial for prevention and mitigation of microvascular and macrovascular complications ...
Type 2 Diabetes Mellitus (T2DM) is a widespread chronic disease that negatively impacts an individual's health and well-being, particularly when uncontrolled. ... Future research should continue to explore . iii relationships among psychosocial and contextual factors and their potential impact on ability to
Diabetes mellitus type 2 is a central challenge for health policy and healthcare in all advanced countries. For the affected persons, living with a diagnosis of type 2 diabetes is difficult because the disease and its treatment have a considerable effect on daily life. The aim of this study was to investigate the challenges associated with a ...
The study concerned 901 patients with 836 type 2 diabetes mellitus (T2DM) and 65 with type 1 diabetes mellitus (T1DM). Results The average age for T2DM and T1DM was 57.86 ± 10.44 and 45.8 ± 17. ...
The estimates in 2019 showed that 77 million individuals had diabetes in India, which is expected to rise to over 134 million by 2045. Approximately 57% of these individuals remain undiagnosed. Type 2 diabetes, which accounts for majority of the cases, can lead to multiorgan complications, broadly divided into microvascular and macrovascular ...